Abstract
Purpose
There is little evidence of the ergogenic effect of flow-resistive masks worn during exercise. We compared a flow-resistive face mask (MASK) worn during high-intensity interval training (HIIT) against pressure threshold loading inspiratory muscle training (IMT).
Methods
23 participants (13 males) completed a 5 km time trial and six weeks of HIIT (3 sessions weekly). HIIT (n = 8) consisted of repeated work (2 min) at the speed equivalent to 95% \({\dot{\text{V}}}\)O2 peak with equal rest. Repetitions were incremental (six in weeks 1, 2 and 6, eight in weeks 3 and 4 and ten in week 5). Participants were allocated to one of three training groups. MASK (n = 8) wore a flow-resistive mask during all sessions. The IMT group (n = 8) completed 2 × 30 breaths daily at 50% maximum inspiratory pressure (PImax). A control group (CON, n = 7) completed HIIT only. Following HIIT, participants completed two 5 km time trials, the first matched identically to pre-intervention trial (ISO time), and a self-paced effort.
Results
Time trial performance was improved in all groups (MASK 3.1 ± 1.7%, IMT, 5.7 ± 1.5% and CON 2.6 ± 1.0%, p < 0.05). IMT improved greater than MASK and CON (p = 0.004). Post intervention, PImax and diaphragm thickness were improved in IMT only (32% and 9.5%, respectively, p = 0.003 and 0.024).
Conclusion
A flow-resistive mask worn during HIIT provides no benefit to 5 km performance when compared to HIIT only. Supplementing HIIT with IMT improves respiratory muscle strength, morphology and performance greater than HIIT alone.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inspiratory Muscle Training (IMT) increases the strength of the chest wall inspiratory muscles and the diaphragm (Brown et al. 2014) and attenuates exercise-induced inspiratory muscle fatigue (Romer and McConnell 2004) and may improve exercise performance, for a review see HajGhanbari et al. (2013). Inspiratory flow-resistive loading (FRL) is a method of IMT that improves respiratory muscle strength and endurance, leading to increased time to exhaustion in cycling (Enright et al. 2006) and treadmill running (Mickleborough et al. 2010). FRL training at 80% of PImax, performed 3 times weekly attenuates minute ventilation (\(\dot{\text{V}}\)E), oxygen consumption (\(\dot{\text{V}}\)O2), heart rate, blood lactate (La-) and perceptual responses during cycling exercise (Gething et al. 2004; Enright et al. 2006).
FRL targets the inspiratory muscles according to Ohms law of resistance. The use of high-force/low-velocity or low-force/high-velocity contractions through a variable size aperture creates a resistive load for the inspiratory muscles (Romer and McConnell 2004). Despite the documented benefits, FRL and other IMT methods have been criticised for poor ecological validity as they fail to reflect dynamic inspiratory muscle function during exercise (McConnell 2013). Recently, there has been a rise in the popularity of affordable FRL devices that can be worn during exercise. These mask-type devices, create a seal around the nose and mouth and require participants to inspire through a variable-sized aperture, providing an inspiratory load to breathing during exercise tasks (Shei et al. 2016). Whilst the stimulus to respiratory and other physiological systems are still to be determined, these approaches are suggested to provide a time-efficient approach to conducting IMT methods during exercise training and addressing previous concerns with ecological validity.
Despite increased popularity, no study has compared these masks with more established forms of IMT. Porcari et al. (2016) observed improved markers of endurance performance (ventilatory threshold, respiratory compensation threshold and power output at both ventilatory threshold and respiratory compensation threshold) when compared to a control group, following 6 weeks of wearing an Elevation training mask during high-intensity cycle ergometer training. However, there were no between-group differences in \(\dot{\text{V}}\)O2peak and peak power output in between the experimental and control group. The authors concluded by stating that the mask did not simulate altitude but rather demonstrated properties (i.e. increased respiratory muscle loading) associated more closely with respiratory muscle training techniques. Further to this, Segizbaeva and Aleksandrova (2018) demonstrated a 12% increase in maximum inspiratory pressure (PImax) alongside a 3% and 7% improvement in 100 m and 3000 m running performance when using an FRL mask during a 12-week intervention. This study used the device in conjunction with a 12-week training programme consisting of middle distance and whole-body resistance activities that were conducted twice weekly.
The need for inspiratory muscle training techniques that can be used during exercise conditions and specifically target the ventilatory profiles achieved during exercise could address previous validity concerns and offer increased benefit to performance. Although research in this space has demonstrated improved respiratory muscle function (i.e. strength) and endurance performance characteristics, no study has compared the ergogenic properties against pressure threshold IMT. Accordingly, this study aimed to test the efficacy of an FRL mask worn during interval training sessions against pressure threshold methods to determine the benefits to time-trial running performance, diaphragm thickness and respiratory muscle strength.
Methods
Participants
Following ethics, approval from the host University, twenty-three (M = 13, F = 10, Table 1) healthy, non-smoking and recreationally trained runners (mean indoor 5 km personal best 26.15 ± 3.19 min; range: 20.73–33.17 min) provided informed written consent. All female participants were taking oral contraceptives throughout their involvement in this study. Before each trial, participants were instructed to avoid exercise on the day preceding and the day of each exercise test. Participants abstained from alcohol and caffeine in the 24 h preceding all trials and completed a 24 h diet record before their first preliminary trial which was replicated in subsequent visits.
Experimental design
Participants completed a total of five laboratory visits, which were separated by a 6-week training intervention. During visit 1, participants were familiarised with all experimental methods and completed an incremental \(\dot{\text{V}}\)O2peak test. During visit 2, diaphragm thickness was assessed and participants completed a 5 km treadmill time-trial. Following visit 2, participants were randomly allocated to one of three training groups and completed six weeks of HIIT. Group 1 consisted of HIIT whilst wearing an FRL training mask (MASK, n = 8, F = 4), group 2, completed IMT as an adjunct to HIIT (IMT, n = 8, F = 4) and group 3, a control group (CON, n = 8, F = 3) who completed HIIT only. In visit 3, participants were re-familiarised with all experimental measures and completed a 5 km time trial. In visit 4, an ISO trial that was matched identically to visit 2. Following a minimum of seven days’ rest, diaphragm thickness was re-assessed, and participants completed a self-paced time-trial (visit 5) Table 2.
Preliminary trials
Peak oxygen uptake (\(\dot{\text{V}}\)O2peak) was determined on a motorised treadmill (Desmo, Woodway, Germany) using a maximal incremental exercise test for the baseline assessment of aerobic fitness. Following a 5 min warm-up at 8 km h−1 and 1% gradient, the gradient was subsequently increased to 4% and speed increased by 1 km h−1 min−1 until the limit of volitional tolerance. Participants wore a Hans Rudolph reusable face mask and online breath by breath gas analysis was conducted (Metalyzer 3B, Cortex Biophysik, Leipzig, Germany). Two-point calibration was completed before each test to ensure the accuracy of the gas (O2; chemical fuel cell and CO2; non dispersive infrared) and flow (TripleV) sensors. Gas concentrations and flow characteristics of exhaled breath were measured to determine \(\dot{\text{V}}\)O2peak, defined as the highest rolling 30 s mean \(\dot{\text{V}}\)O2 recorded during the test. Previously published guidelines were used to calculate \(\dot{\text{V}}\)O2peak (Howley et al. 1995). Following a minimum of seven days’ rest after this test, participants completed a familiarisation of the 5 km time-trial which is described in full below.
During visit 2, diaphragm thickness (Tdi) was assessed via ultrasound (Philips iU22, Guilford, UK) as previously described by our group (Brown et al. 2013). Briefly, the diaphragm was assessed in the zone of apposition with an L17-5 MHz linear array transducer that was adjusted accordingly to the depth of the diaphragm. Participants were positioned upright with their right arm raised and the transducer position was then adjusted between the 7th and 10th intercostal space in the mid-axillary line where a coronal view of the right hemidiaphragm was identified. Fine adjustment of the transducer position was used to place the diaphragm in a horizontal plane across the field of view and to ensure a 90° angle of insonation. Measurements were recorded from functional residual capacity following a passive expiration from total lung capacity. Tdi was defined by onscreen callipers positioned at 90° to the diaphragm from the leading edge of the pleural membrane to the leading edge of the peritoneum membrane (see Fig. 1). Measurements were repeated in triplicate and averaged for subsequent analyses. The within-trial coefficient of variation for Tdi was 2.6% with a within-participant intra-class correlation coefficient of 0.99 which was in accordance with our previous work (Brown et al. 2013).
Experimental trials
Participants completed a 5 km time trial on a motorised treadmill using the protocol of Driller et al. (2017). Participants were blinded to their elapsed time and standardised verbal encouragement was given (in line with the collection of physiological measures and perceptual responses) throughout the trial. The trial was commenced from a stationary start and running speed was manually adjusted by the participant to complete the distance in the quickest time possible. Changes in speed and the time of adjustment were recorded for the subsequent ISO trial. Prior to exercise, pulmonary function, inspiratory (PImax) and expiratory (PEmax) muscle pressures were measured following published guidelines (American Thoracic Society and European Respiratory Society 2002). Briefly, a hand-held mouth pressure meter (MicroRPM; CareFusion, Hampshire, UK) measured PImax and PEmax, with manoeuvres initiated from residual volume and total lung capacity, respectively, and sustained for at least 3 s. A minimum of five attempts was recorded with a 30 s rest between each attempt. Dynamic Pulmonary function for the measurement of lung function (FEV1, FVC, FEV1/FVC, and PEF) was assessed using an electronic flow sensor (MS03, Micro Medical, Buckinghamshire, UK). Respiratory mouth pressures and then pulmonary function were assessed immediately post exercise.
Blood lactate concentration (La-) was measured pre- and post-trial using fingertip capillary samples (Biosen, EKF Diagnostics, Barleben, Denmark). All other parameters including heart rate (Polar T31, Kempele, Finland) and perceptual responses including whole body perceived effort (Borg 1982) and breathing discomfort (using a visual analogue scale: where 0 = no exertion and 10 = maximal exertion, Verges et al. 2007) were measured, upon completion of each kilometre and during the final 50 m of the time-trial. Expired pulmonary gases (O2, and CO2) and flow characteristics (breathing frequency, tidal volume, and minute ventilation) were measured continuously throughout the trial (averaged over 30 s during analysis) using online gas analysis (Metalyzer II; Cortex Biophysik, Leipzig, Germany).
Following training and re-familiarisation, Tdi was re-assessed and participants completed two additional experimental 5 km time trials. The first was an ISO trial which was matched identically to the speed recorded during the pre-intervention trial. Changes in treadmill speed for the ISO trial were automated using Metasoft® Studio (Cortex Biophysik, Leipzig, Germany). Following a minimum of seven days, a second self-paced, all-out time trial was completed. Training activities were reduced to a maintenance load for all participants between experimental trials and consisted of two HIIT sessions (6 repetitions), IMT was also reduced to a maintenance load (3 × sessions weekly) following previous recommendations (Romer and McConnell 2003).
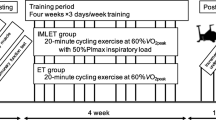
Training interventions
Participants were randomly allocated to one of the three training groups: inspiratory FRL training using a mask (MASK), pressure threshold Inspiratory Muscle Training (IMT) or a control group. Participants completed six weeks of high-intensity interval training (hereon referred to as HIIT). HIIT sessions were conducted at the velocity equivalent to 95% \(\dot{\text{V}}\)O2peak, calculated via linear regression derived from the relationship between \(\dot{\text{V}}\)O2 and velocity. All sessions were supervised and established using the guidelines of Buchheit and Laursen (2013). Briefly, participants exercised for 2-min intervals followed by 2 min of static rest on the same treadmill used in previous sessions. Training frequency (3 sessions weekly) was separated by at least 24 h, with a mean rest of 52.8 ± 27.0 h and 2.2 ± 1.1 days between individual sessions. Exercise intensity remained constant throughout the intervention; however, the number of repetitions was incremental throughout the intervention (six in weeks 1, 2 and 6, eight in weeks 3 and 4 and ten in week 5).
Participants allocated to the MASK group completed whole-body HIIT training sessions whilst wearing an FRL mask (Phantom Training Mask, Phantom Athletics, Salzburg, Austria). The resistance was set at level 4 (of 4) for all participants irrespective of baseline PImax. The mask was worn for the duration of each session, including during recovery periods providing an inspiratory resistance but no expiratory resistance. The IMT group completed HIIT but used a pressure threshold IMT device (POWERbreathe® classic series, HaB International, Warwickshire, UK) twice daily (morning and evening) throughout the intervention and the time between IMT and HIIT sessions was at least 1 h. Training load was set at 50% PImax and comprised thirty consecutive dynamic inspiratory efforts, twice daily, for six weeks. Each inspiratory effort was initiated from residual volume and participants endeavoured to maximise tidal volume (Faghy and Brown 2016). PImax was assessed bi-weekly during the training intervention, allowing the training load to be adjusted. CON completed HIIT only. Training compliance in all groups was monitored using a self-report training diary.
Statistical analysis
Statistical analysis was performed using SPSS for Windows (SPSS, Chicago, IL, USA). A Shapiro–Wilk test was used to determine normality of the data. A repeated-measures, three-way ANOVA (independent variables: time, pre- and post-intervention across three groups) was used to assess changes over time in each time-trial, pre–post intervention and between each group. A Fishers Least Significant Difference (LSD) test was used to identify statistically different pre- to post-intervention changes. A priori α was set at 0.05, all results are presented as mean ± SD and effect size (ES) reported for pairwise comparisons. Effect sizes were calculated using Cohen’s d (d = (x1–x2)/pooled σ) and interpreted accordingly (small effect d = 0.2, moderate effect d = 0.5 and large effect d = 0.8).
Results
Pre-intervention descriptive characteristics of participants are shown in Table 1 and there were no between-group differences in any variable (p > 0.05). Training compliance was high IMT (IMT 94 ± 8%) and in line with previous work in this area.
Time-trial performance
Baseline, time-trial performance was not different between groups (MASK 26.14 ± 2.21 min, IMT 25.97 ± 2.07 min and CON 26.36 ± 2.42 min, p > 0.05). For time-trial performance, there was a main effect for pre–post intervention (p = 0.027, Fig. 2) and group (p = 0.018). Pre–post changes in time-trial performance were highlighted with a two-way interaction for group and time (p = 0.015). Time-trial performance was most improved in IMT (absolute reduction = 1.43 ± 0.48 min, 5.7 ± 1.5%, p = 0.007; effect size: d = 0.40). MASK (absolute reduction = 0.76 ± 0.33 min, 3.13 ± 1.7%, p = 0.034; effect size: d = 0.19) and CON (absolute reduction = 0.74 ± 0.47 min, 2.64 ± 1.0%, p = 0.043; effect size: d = 0.17) were also improved, but changes in performance were similar (p > 0.05).
Respiratory function and diaphragm thickness
Pre-intervention values of PImax were not different between groups and unchanged following exercise (pooled mean pre: 124 ± 25 cmH2O vs post: 114 ± 21 cmH2O, absolute reduction 11 ± 13 cmH2O, 9 ± 10%, p = 0.358). Post-intervention PImax was improved in IMT only (pre: 112 ± 29 cmH2O vs post 140 ± 20 cmH2O, p = 0.008, absolute increase 34 ± 12 cmH2O, 32 ± 16%, effect size: d = 0.81). PImax was unchanged in MASK (pre: 115 ± 18 cmH2O vs post 114 ± 26 cmH2O, p = 0.445, effect size: d = 0.14) and CON (pre: 112 ± 31 cmH2O vs post 115 ± 22 cmH2O, p = 0.217, effect size: d = 0.25).
Tdi was not different between groups at baseline (pooled mean 1.8 ± 0.3 mm) but was increased in IMT only (pre: 1.8 ± 0.2 mm vs post: 2.0 ± 0.2 mm, absolute change = 0.2 ± 0.2 mm, 9.5 ± 3.4%, p = 0.032, effect size d = 0.73) and was unchanged in MASK (pre: 1.9 ± 0.2 mm vs post: 1.9 ± 0.3 mm, absolute change = 0.1 ± 0.2 mm, p = 0.417, effect size d = 0.29) and CON (pre: 1.8 ± 0.3 mm vs post: 1.8 ± 0.2 mm, absolute change = 0.0 ± 0.2 mm, p = 0.283, effect size d = 0.12).
Pulmonary function
Pre-intervention values of pulmonary function were not different between groups (Table 1) and were unchanged following both exercise and the intervention.
Physiological and perceptual responses
Baseline and post-exercise values of HR were not different between groups (Tables 2, 3 and 4). All physiological and perceptual responses were similarly increased in each trial. La- was lower post exercise following the ISO trial post-intervention in all groups (see Tables 3, 4 and 5, p < 0.05). All other variables where unchanged.
Discussion
This study aimed to determine whether a flow-resistive device worn during exercise led to increased time-trial performance above the benefits to performance provided by HIIT. The key finding demonstrates that flow-resistive masks worn during HIIT training provided no additional benefit to 5 km running performance when compared to HIIT training only. Second, all interventions improved 5 km running performance but the relative improvement in IMT was greater than the improvement observed in MASK and CON. No change in physiological and perceptual responses with masks was observed when compared to baseline, post-intervention ISO trial and post-intervention all-out trial.
Typically, respiratory muscle training techniques are conducted as an adjunct to exercise training regimes. The use of face masks during exercise poses an inspiratory resistive load that is proportional to inspiratory flow rates observed during exercise, therefore increasing the work of breathing. However, the effectiveness and supporting datasets for these devices are limited and have not been compared against other IMT methods. Porcari et al. (2016), incorporated the Elevation Training Mask 2.0 into 6 weeks of high-intensity cycle ergometer training and reported increased endurance performance (power output at ventilatory threshold) but there were no changes in maximal exercise performance (\(\dot{\text{V}}\)O2max or peak power output) when expressed relative to the improvement observed in the control group. This may be expected as it is well documented that \(\dot{\text{V}}\)O2max is unaffected by IMT methods since it fails to influence any point of the physiological determinants that comprise \(\dot{\text{V}}\)O2max (Brown et al. 2010). More recently Segizbaeva and Aleksandrova (2018) demonstrate improved respiratory muscle strength and endurance after 12 weeks of using an FRL face mask during running exercise and improved 100 m and 3000 m running performance (3% and 7%, respectively). Whilst the mechanism of improved performance is not explored by the authors, it is likely the result of acclereated O2 kinteics at the onset of exercise, as previously demonstrated by our group (Brown et al. 2012). It is, however, unclear how 100 m sprint performance would be improved following FRL training as the combined time and exercise intensity is unlikely to result in a significant contribution from ventilatory parameters (Harms et al. 2000). The onset of respiratory muscle fatigue, the respiratory muscle metaboreflex and associated sensations of respiratory and/or locomotor discomfort are also unlikely when considering the known determinants of respiratory muscle work that influence performance (Dempsey et al. 2006). Furthermore, Jagim et al. (2018) report that wearing an FRL mask during resistance exercise does not impede the ability to complete resistance training sessions. The authors noted acute increases in metabolic stress markers (La-), ratings of mental fatigue and a reduction in the peak velocity during inspiratory efforts measured during resistance activities (back squat and bench press). The authors did report concerning side effects, which included reduced alertness and focus during resistance exercises, the underlying mechanism causing this change was not determined and increased mechanistic understanding is needed here.
The results of this current study demonstrate that the mask which mimics FRL yields no additional benefit to treadmill running performance when used in conjunction with HIIT training. As previously mentioned, FRL specifically loads the inspiratory muscles using either high-force/low-velocity or low-force/high-velocity contractions. A determinant of this methods is the need to maintain a sufficient load to the inspiratory muscles, according to Ohms law of resistance. Although previous work demonstrates that HIIT produces high flow rates and leads to increased PImax (Dunham and Harms 2012), these improvements were not observed in the current study. This is likely due to the absence of high flow rates providing an insufficient stimulus for the respiratory muscles to adapt, as demonstrated in previous research adopting FRL techniques where ventilation is controlled (Mickleborough et al. 2010). Recent data support this notion and emphasise the need for sufficiently strenuous, inspiratory flow-resistive loads (> 50% PImax) to elicit an adaptive response and whilst this did not influence peak transdiaphragmatic pressure, markers of oxidative stress were elevated (Briskey et al. 2020). Although not measured as part of this study, the resistance posed by the masks during exercise is an important consideration in their overall effectiveness and future research should look to quantify the inspiratory load and the work of breathing during exercise with a flow-resistive load mask to determine whether these methods provide a sufficient and consistent overload stimulus that could lead to chronic adaptations within the respiratory muscles.
The present study demonstrates that pressure threshold IMT that is conducted as an adjunct to exercise training continues to be an effective ergogenic aid for sports performance. The results here demonstrate a 5.7 ± 1.5% (mean reduction 1.43 ± 0.48 min) increase in 5 km TT performance which is greater than the improvement in HIIT alone 2.7 ± 1.0% (mean reduction = 0.74 ± 0.47 min). It is important here to acknowledge that the absence of a placebo group and that further research is needed to confirm true ergogenic properties of IMT. PTL methods use progressive overload to the respiratory muscles which results in beneficial adaptations and increases exercise performance (for a full review see (HajGhanbari et al. 2013). Our findings are consistent with previous data that demonstrate improved performance in a range of exercise modalities which include but is not limited to, middle distance and endurance running (Ross et al. 2008; Edwards et al. 2008), cycling (Romer et al. 2002; Gething et al. 2004) (including during hypoxic conditions (Salazar-Martínez et al. 2017), swimming (Shei et al. 2016), rowing (Griffiths and McConnell 2007) and during occupational performance tests (Faghy and Brown 2014; Shei et al. 2018). The mechanism by which IMT improved performance is in line with previous work in the area which demonstrates increased PImax and Tdi. Chronic interventions (typically 4–6 weeks) repeatedly demonstrate neural adaptations (Hawkes et al. 2007) and structural changes (Enright et al. 2006; Downey et al. 2007) which augment respiratory muscle strength, endurance and efficiency and during exercise allows the respiratory muscles to work at a lower relative intensity during exercise.
Despite attempts to improve the ecological validity of FRL methods, the findings of this study demonstrate that these masks that are worn during exercise training yield no additional benefit to running performance above those posed by HIIT training. This is likely, although yet to be confirmed due to insufficient stimuli that are presented to the inspiratory muscles during exercise tasks, thus resulting in no adaptation to respiratory muscle strength and/or endurance. The use of PTL IMT techniques that are used as an adjunct to training demonstrate improved respiratory strength, endurance and exercise performance and should be used in favour of methods that seek to combine exercise and IMT.
Conclusion
IMT used as an adjunct to training improves running performance above the benefits provided by HIIT training. The use of a flow-resistive training mask worn during HIIT sessions yields no additional benefit to HIIT alone. We suggest that this is due to insufficient inspiratory load and further research should seek to quantify the work of breathing and flow rates during exercise which are known determinants of the adaptions associated with flow-resistive loading methods.
Abbreviations
- \(\dot{\text{V}}\)CO2 :
-
Carbon dioxide production
- \(\dot{\text{V}}\) E :
-
Minute ventilation
- \(\dot{\text{V}}\)O2 :
-
Oxygen consumption
- \(\dot{\text{V}}\)sO2peak:
-
Peak oxygen uptake
- ANOVA:
-
Analysis of variance
- CON:
-
Control
- FEV1 :
-
Forced expired volume in one second
- FRL:
-
Flow resistive loading
- FVC:
-
Forced vital capacity
- HIIT:
-
High-intensity interval training
- HR:
-
Heart rate
- IMT:
-
Inspiratory muscle training
- La:
-
Blood lactate
- PEF:
-
Peak expiratory flow
- P Emax :
-
Maximal expiratory pressure
- P Imax :
-
Maximal inspiratory pressure
- RER:
-
Respiratory exchange ratio
- T di :
-
Diaphragm thickness
References
American Thoracic Society, European Respiratory Society (2002) ATS/ERS statement on respiratory muscle testing. Am J Respir Crit Care Med 166:518–624. https://doi.org/10.1164/rccm.166.4.518
Borg GAV (1982) Psychophysical bases of perceived exertion. Med Sci Sports Exerc 14:377–381
Briskey D, Vogel K, Johnson MA et al (2020) Inspiratory flow resistive breathing, respiratory muscle induced systemic oxidative stress and diaphragm fatigue in healthy humans. J Appl Physiol 129(1):185–193
Brown PI, Johnson M, Sharpe GR (2014) Determinants of inspiratory muscle strength in healthy humans. Respir Physiol Neurobiol 196:50–55. https://doi.org/10.1016/j.resp.2014.02.014
Brown PI, Sharpe GR, Johnson MA (2010) Loading of trained inspiratory muscles speeds lactate recovery kinetics. Med Sci Sports Exerc 42:1103–1112
Brown PI, Sharpe GR, Johnson MA (2012) Inspiratory muscle training abolishes the blood lactate increase associated with volitional hyperpnoea superimposed on exercise and accelerates lactate and oxygen uptake kinetics at the onset of exercise. Eur J Appl Physiol 112:2117–2129
Brown PI, Venables HK, Liu H et al (2013) Ventilatory muscle strength, diaphragm thickness and pulmonary function in world-class powerlifters. Eur J Appl Physiol 113:2849–2855
Buchheit M, Laursen PB (2013) High-intensity interval training, solutions to the programming puzzle. Sports Med 43:927–954. https://doi.org/10.1007/s40279-013-0066-5
Dempsey JA, Romer LM, Rodman J et al (2006) Consequences of exercise-induced respiratory muscle work. Respir Physiol Neurobiol 151:242–250
Downey AE, Chenoweth LM, Townsend DK et al (2007) Effects of inspiratory muscle training on exercise responses in normoxia and hypoxia. Respir Physiol Neurobiol 156:137–146
Driller M, Brophy-Williams N, Walker A (2017) The reliability of a 5 km run test on a motorized treadmill. Meas Phys Educ Exerc Sci 21:121–126. https://doi.org/10.1080/1091367X.2016.1264402
Dunham C, Harms CA (2012) Effects of high-intensity interval training on pulmonary function. Eur J Appl Physiol 112:3061–3068
Edwards AM, Wells C, Butterly R (2008) Concurrent inspiratory muscle and cardiovascular training differentially improves both perceptions of effort and 5000 m running performance compared with cardiovascular training alone. Br J Sports Med 42:823–827. https://doi.org/10.1136/bjsm.2007.045377
Enright SJ, Unnithan VB, Heward C et al (2006) Effect of high-intensity inspiratory muscle training on lung volumes, diaphragm thickness, and exercise capacity in subjects who are healthy. Phys Ther 86:345–354
Faghy MA, Brown PI (2016) Training the inspiratory muscles improves running performance when carrying a 25 kg thoracic load in a backpack. Eur J of Sport Science 16(5):585–594. https://doi.org/10.1080/17461391.2015.1071878
Gething AD, Williams M, Davies B (2004) Inspiratory resistive loading improves cycling capacity: a placebo controlled trial. Br J Sports Med 38:730–736. https://doi.org/10.1136/bjsm.2003.007518
Griffiths LA, McConnell AK (2007) The influence of inspiratory and expiratory muscle training upon rowing performance. Eur J Appl Physiol. https://doi.org/10.1007/s00421-006-0367-6
HajGhanbari B, Yamabayashi C, Buna TR et al (2013) Effects of respiratory muscle training on performance in athletes: a systematic review with meta-analyses. J Strength Cond Res 27:1643–1663
Harms CA, Wetter TJ, Croix CMS et al (2000) Effects of respiratory muscle work on exercise performance. J Appl Physiol 89:131–138
Hawkes EZ, Nowicky AV, McConnell AK (2007) Diaphragm and intercostal surface EMG and muscle performance after acute inspiratory muscle loading. Respir Physiol Neurobiol 155:213–219
Howley ET, Bassett DR, Welch HG (1995) Criteria for maximal oxygen uptake: review and commentary. Med Sci Sports Exerc 27:1292–1292
Jagim AR, Dominy TA, Camic CL et al (2018) Acute effects of the elevation training mask on strength performance in recreational weight lifters. J Strength Cond Res 32:482–489. https://doi.org/10.1519/JSC.0000000000002308
McConnell AK (2013) Respiratory muscle training: theory and practice. Elsevier Health Sciences, Amsterdam
Mickleborough TD, Nichols T, Lindley MR et al (2010) Inspiratory flow resistive loading improves respiratory muscle function and endurance capacity in recreational runners. Scand J Med Sci Sports 20:458–468. https://doi.org/10.1111/j.1600-0838.2009.00951.x
Porcari JP, Probst L, Forrester K et al (2016) Effect of wearing the elevation training mask on aerobic capacity, lung function, and hematological variables. J Sports Sci Med 15:379–386
Romer LM, McConnell AK, Jones DA (2002) Effects of inspiratory muscle training on time-trial performance in trained cyclists. J Sports Sci 20:547–590
Romer LM, McConnell AK (2004) Respiratory muscle training in healthy humans: resolving the controversy. Int J Sports Med 25:284–293
Romer LM, McConnell AK (2003) Specificity and reversibility of inspiratory muscle training. Med Sci Sports Exerc 35:237–244
Ross E, Middleton N, Shave R et al (2008) Changes in respiratory muscle and lung function following marathon running in man. J Sports Sci 26:1295–1301
Salazar-Martínez E, Gatterer H, Burtscher M et al (2017) Influence of inspiratory muscle training on ventilatory efficiency and cycling performance in normoxia and hypoxia. Front Physiol 8:133
Segizbaeva MO, Aleksandrova NP (2018) Effect of the elevation training mask on the functional outcomes of the respiratory muscles. Hum Physiol 44:656–662
Shei R-J, Chapman RF, Gruber AH, Mickleborough TD (2018) Inspiratory muscle training improves exercise capacity with thoracic load carriage. Physiol Rep 6:e13558
Shei R-J, Lindley M, Chatham K, Mickleborough TD (2016) Effect of flow-resistive inspiratory loading on pulmonary and respiratory muscle function in sub-elite swimmers. J Sports Med Phys Fit 56:392–398
Verges S, Lenherr O, Haner AC et al (2007) Increased fatigue resistance of respiratory muscles during exercise after respiratory muscle endurance training. Am J Physiol-Regul Integr Comp Physiol 292:R1246–R1253
Author information
Authors and Affiliations
Contributions
MF and TMW conceived the conceived and designed research and were assisted by PB in the analysis and preparation of the manuscript. ND and JPM were responsible for data collection which was overseen by MF. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Additional information
Communicated by Susan Hopkins.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Faghy, M.A., Brown, P.I., Davis, N.M. et al. A flow resistive inspiratory muscle training mask worn during high-intensity interval training does not improve 5 km running time-trial performance. Eur J Appl Physiol 121, 183–191 (2021). https://doi.org/10.1007/s00421-020-04505-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00421-020-04505-3