Abstract
Purpose
As climate change accelerates, healthcare workers (HCW) are expected to be more frequently exposed to heat at work. Heat stress can be exacerbated by physical activity and unfavorable working requirements, such as wearing personal protective equipment (PPE). Thus, understanding its potential negative effects on HCW´s health and working performance is becoming crucial. Using wearable sensors, this study investigated the physiological effects of heat stress due to HCW-related activities.
Methods
Eighteen participants performed four experimental sessions in a controlled climatic environment following a standardized protocol. The conditions were (a) 22 °C, (b) 22 °C and PPE, (c) 27 °C and (d) 27 °C and PPE. An ear sensor (body temperature, heart rate) and a skin sensor (skin temperature) were used to record the participants´ physiological parameters.
Results
Heat and PPE had a significant effect on the measured physiological parameters. When wearing PPE, the median participants’ body temperature was 0.1 °C higher compared to not wearing PPE. At 27 °C, the median body temperature was 0.5 °C higher than at 22 °C. For median skin temperature, wearing PPE resulted in a 0.4 °C increase and higher temperatures in a 1.0 °C increase. An increase in median heart rate was also observed for PPE (+ 2/min) and heat (+ 3/min).
Conclusion
Long-term health and productivity risks can be further aggravated by the predicted temperature rise due to climate change. Further physiological studies with a well-designed intervention are needed to strengthen the evidence for developing comprehensive policies to protect workers in the healthcare sector.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Climate change is one of the major challenges of our time (Trenberth 2018; UNEP 2021). In Germany, the average temperature has increased by more than 1.5 °C since 1881 and extreme weather events such as hot summer days (> 30 °C) and heat waves (multiple consecutive days with > 30 °C) will occur more frequently (Papalexiou et al. 2018; IPCC 2019; van Rüth et al. 2019).Climate change affects many occupations in terms of heat stress, e.g. road and agricultural workers. However, indoor temperatures may also reach subjectively uncomfortable but also health-relevant levels as air-conditioned workplaces are not common in Germany (Lenzer et al. 2020). In Germany, the German Society for Occupational and Environmental Medicine (Deutsche Gesellschaft für Arbeitsmedizin und Umweltmedizin e. V. (DGAUM)) defines “working under heat stress” as climatic stress in the workplace caused by an extreme increase in indoor/outdoor temperature due to heat (DGAUM 2012). Increased indoor temperatures due to hot weather are known to cause heat strain (Simister and Cooper 2005). Amongst others, healthcare workers (HCW) such as nurses have an increased risk of heat strain due to comparatively high job-related physical activity (Schoierer et al. 2019). This may be further aggravated by the use of personal protective equipment (PPE) (Dorman and Havenith 2009).
Heat strain is the overall physiological response resulting from heat stress. If the core body temperature exceeds normal levels (36.8–37.5 °C) and the thermoregulatory system fails to compensate the heat stress, the risk of heat strain increases (Mazlomi et al. 2017; Ebi et al. 2018). A core body temperature above 38 °C can lead to fatigue, headache, dizziness, loss of appetite and rapid breathing (Gostimirovic et al. 2020). Heat stress triggers the production of stress hormones such as adrenaline, noradrenaline, and cortisol (McMorris et al. 2006). This may explain in part the physiological responses of heat stress such as an increase of core and peripheral temperature, heart rate, and sweating (Mazlomi et al. 2017). Multiple studies have shown that long-term exposure to heat reduces the work capacity and increase mortality rates within the general population (Rowell 1974; Arbury et al. 2014; Steul et al. 2018; an der Heiden et al. 2019; Bisolli et al. 2019; Vicedo-Cabrera et al. 2021).
Although body temperature and other physiological parameters can help to detect symptoms of heat strain, their monitoring in occupational settings is still challenging. As wearable devices are becoming more advanced, the online monitoring of selected health parameters may help to better understand and monitor changes due to increased temperature (Notley et al. 2018). In general, wearable devices consist of three main components: (1) the hardware measuring physiological and/or activity data, (2) the communication hardware and software to relay data to a (remote) processing unit and (3) the data analysis techniques to extract clinically relevant information from the obtained data (Patel et al. 2012). Their current capabilities include physiological, biochemical and motion sensing (Teng et al. 2008; Bonato 2010). However, wearable devices to assess physiological parameters related to heat strain due to occupational heat stress among HCW, have not been used thus far.
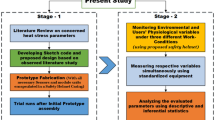
Therefore, the goal of this study was the feasibility assessment of wearable devices for the monitoring of physiological parameters of HCW during controlled heat stress conditions. Furthermore, the individual effects of high temperatures and PPE on these parameters were investigated.
Materials and methods
Study design and experimental setup
This study was designed as a crossover trial, which took place between October 2021 and March 2022. The experiments took place in climate chamber (5 × 3 × 2.2 m (L/W/H)) with temperature and humidity control. The interior included a table with a chair, a treadmill, a 170 patient bed and patient dummy (CLA1®, 21 kg, Coburger Lehrmittelanstalt, Coburg, Germany). A photo of the climate chamber setting can be found in the supplemental information (Fig. S1).
Four independent experiments were performed by each the participants: (1) at 22.0 °C without PPE (NN), at 22 °C with PPE (NP), (3) at 27 °C without PPE (WN) and (4) at 27 °C with PPE (WP). The selection of the higher temperature was based on the guidelines of the German Federal Ministry of Labour and Social Affairs, recommending that the ambient temperature in workspaces should not exceed 26 °C (BMAS 2022). However, we chose 27 °C in order to achieve a sufficient temperature difference to the reference temperature of 22 °C. The relative humidity was set to 40% for all four scenarios to limit the number of experimental variables. Participant wore a standard hospital gown and additional PPE (disposable plastic gown, FFP2 face mask, face shield and gloves) if applicable. To alleviate a habituation or training effect, the setting´s sequence was randomized. During the experiment participants performed HCW-related activities within a given time. These activities include, amongst others, walking up to 5.8 km/h on a treadmill, mobilization and washing of a dummy and the simulation of administrative tasks. The full protocol can be found in the supplementary information. Except for temperature and PPE, all other conditions were identical. One experiment lasted 3.5 h. Each participant conducted all experiments at the same time of the day (either mornings or afternoons) and the interval between two individual experiments was at least seven but maximum ten days. These prerequisites aimed to minimize interfering effects of circadian rhythms and differences in the participants´ physiological condition (Goel et al. 2013).
Participants
Inclusion of eligible participants was based on the medical history, by considering the following criteria: (1) age 18–60 years; (2) medical background or experience as HCW, since they had to perform several HCW-related activities; (3) no sensitivity against heat (e.g., dizziness, redness on the skin); (4) no obesity (BMI < 30); and (5) no severe chronic diseases. Prior to each experiment, participants were asked about their general state of health. Furthermore, heart rate, blood pressure and body temperature (forehead) were measured to exclude illnesses that may interfere with the study.
Monitoring of the environmental conditions
A QUESTemp 34 Heat Stress Monitor® (Quest Technologies, Wisconsin, USA) was utilized for assessing the heat stress by the environmental conditions in the climate chamber. The instrument was placed on a table at a height of approximately one meter. It was also ensured that this device was placed away from any barriers that might block radiant heat or flow. The participants were also requested not to move too close to this instrument in order to minimize variations in temperature and radiant heat. The sampling interval was one minute.
Monitoring of physiological parameters
A cosinuss° Two® (Cosinuss GmbH, Munich, Germany) in-ear sensor was utilized to monitor participants´ in-ear temperature (IET) and heart rate (HR) during the experiments (Fig. 1). For each participant, the appropriate sensor size (small or medium) was selected during the anamnesis. The sampling interval was one second. After 14 min of recording, the data were sent to the cosinuss° Health cloud server via a Gateway within one minute. This cycle was repeated during the whole experiment.
Moreover, skin temperatures were monitored using Thermochron iButton® temperature loggers (CK electronic GmbH, Cologne, Germany) (Fig. 1). The sensors were placed at five different central and peripheral locations (left/right infraclavicular, belly and left/right midthigh). The sampling interval was one minute. Finally, to evaluate the participants´ clinical state, their weight, forehead temperature, blood pressure, and heart rate were measured before and after each experiment using a digital body scale, an infrared thermometer and a medical blood pressure cuff, respectively.
Data handling and statistical analysis
Prior to the analysis, all data were pre-processed. In detail, sections outside the trials, including those with apparent sensor malfunctions, were removed and the remaining measured data were used for the analysis. Furthermore, only physiological data measured under the dry bulb indoor temperature between 20 and 24 °C for normal conditions and between 25 and 29 °C for warm conditions were included in the analysis. For in-ear temperature and heart rate, one-minute medians were calculated to match the interval of the skin sensors. Additionally, only heart rate results with corresponding signal quality index above 50 were used. The signal quality index is an algorithm quantitatively assesses the functional near-infrared spectroscopy signal quality on a numerical scale from 0 (very low quality) to 100 (very high quality). Moreover, longitudinal data from the five skin temperature measurements were corrected using an external calibration. For the calculation of the mean skin temperature (MST) for one experiment, the results of all five sensors were averaged.
Each physiological parameter was tested for normality using the Kolmogorov–Smirnov test. The analysis of variance (ANOVA) test was utilized to compare the measured data. All parameters were found to be non-normally distributed. Therefore, the Wilcoxon rank-sum test was considered. Since this method is not robust against systematic interindividual variability, a linear mixed-effects model analysis was used to properly consider the interindividual differences. The mixed model approach was broadly used in previous accelerometer studies (Van Dongen et al. 2004; Haapalainen et al. 2008; Pfeiffer et al. 2009; Bolton et al. 2021). In particular, we were interested in making conclusions about how the trial settings over time (fixed effects) impact the measured physiological parameters by controlling the individual differences (random effects). Alpha (α) level at 0.05 was set for all statistical tests. All p-values were two-tailed. The data cleaning process and statistical analysis were performed using R statistical software (version 4.1.2.®).
Results
Participants´ clinical characteristics
Eighteen participants (n = 11 females, n = 7 males) completed all four experimental sessions (with a mean interval of 8 days). The majority of them are actively working as HCW (nurses). Their mean age was 35.2 ± 10.4 years old (22–57). Pre-post-increases were observed in participants´ weight and forehead temperature. Table 1 presents all participants’ clinical characteristics from the medical history.
Measured data from the used instruments
For trials under normal temperature (NN and NP), the average dry bulb temperature was 23.0 °C (heat index of 21.2 °C) and the value was 27.3 °C (heat index of 27.2 °C) for the trials under warm temperatures (WN and WP). The measured mean relative humidity for all settings was 34 ± 5.2%. The results of in IET, HR and MST during all experimental sessions are shown in Fig. 2: The data is presented as one-minute-medians calculated from the results of all participants (n = 18). Additionally, a non-time-resolved representation of the data as box-whisker-plots can be found in the supplemental information (Fig S2).
Concerning participants´ IET, the median values during experimental sessions under warm temperatures were higher than those under normal temperatures (37.3 °C, 37.4 °C, 37.8 °C, and 37.9 °C for NN, NP, WN and WP, respectively). Using the identical order, the median values for participants´ HR were 76, 78, 79, and 83 beats/min. The median values for participants´ MST were 32.0 °C, 32.4 °C, 33.0 °C, and 33.4 °C for NN, NP, WN and WP, respectively.
Using the ANOVA (i.e., Wilcoxon rank-sum test), the differences in each physiological parameter between all four trial settings were found as significant (p < 0.001). However, as this method is not robust against systematic interindividual variability, the data were re-analyzed and predicted using the linear mixed-model regression.
Prediction model using linear mixed regression analysis
To analyze the interindividual differences in the physiological data, a mixed-model regression analysis was performed. This model takes within- and between-subjects variance into account. The term “mixed model” refers to the inclusion of both fixed effects, which are model components used to define systematic relationships such as the physiological changes over time and/or experimentally induced group differences, as well as random effects, which account for variability among participants around the systematic relationships captured by the fixed effects (Van Dongen et al. 2004; Ravindra et al. 2019). Figure 3 illustrates our regression model.
Despite individual variances, among 18 participants, compared to the initial session (NN), significant increments were found within all trials (p < 0.001), particularly during the session WP (+ 0.5 °C for IET; + 5 beats/min for HR and + 1.1 °C for MST). The regression coefficients of all measured parameters are listed in Table 2.
Discussion
In our study, we focused on HCW since there is a substantial research gap on heat strain for this occupation. We postulated that the heat strain among HCW generated from their physical activities is exacerbated by the heat stress due to increased indoor temperatures. This situation can be further aggravated due to the wearing of PPE, as it has been mandatory caring for patients with SARS-CoV-2 or other infectious diseases. Based on these hypotheses, our cross-over study revealed that the combination of internal and external heat stress while conducting HCW-related activities in the climate chamber induces a significant increase in all observed physiological parameters. This increment was particularly high when performing the experimental scenario wearing PPE at 27 °C. Such findings support previous studies concerning the adverse effects of occupational heat strain, particularly attributable to the wearing of PPE (Dorman and Havenith 2009; Eggenberger et al. 2018; Foster et al. 2020b).
The measurement of the IET as a proxy of the body temperature and HR using wearables was based on existing studies as it has been shown that such physiological parameters can provide indicators of health status and have tremendous diagnostic value (Eggenberger et al. 2018). Additionally, we realized that measuring participants´ MST is also important, as it is considered an indicator of thermal sensation. Although the thermoregulatory mechanisms of healthy humans allow only minor changes in core temperature, peripheral skin temperatures respond clearly to changes in ambient temperature or metabolism (Krishnamurthy et al. 2017).
Besides the increase in the observed physiological parameters (IET, HR and MST), participants frequently reported drinking more water, feeling tired, and sweating excessively during the experiments with PPE (Quartucci et al., Effects of heat and personal protective equipment on thermal strain in health care workers—Part A: Application of a standardized protocol and assessment of subjective well-being, submitted for publication).
It is well known that heat stress reduces the human capability to perform activities at full capacity due to the physiological dysfunction (Russo et al. 2019; Foster et al. 2020b). In the study by Gostimorovic et al. concerning heat stress on human cardiovascular functions, a vigorous, long-term impairment of physiological parameters did lead to several health issues such as heart attacks, malignant cardiac arrhythmias, thromboembolic diseases and heat-induced sepsis like shock. (Gostimirovic et al. 2020).
As climate change progresses, the frequency of hot days with uncomfortable indoor temperatures is expected to increase. This situation can lead to heat strain events when the core body temperature exceeds its normal level, resulting from a total heat load exceeding the capacity for heat dissipation. This may cause long-term health and productivity risks with devastating economic consequences (Russo et al. 2019).
Finally, the feasibility of using Cosinuss° Two in-ear sensor® to observe the physiological response which is attributable as heat stress was investigated. While some studies described the advantages of this device (Burgos et al. 2020; Ellebrecht et al. 2022), some evaluated the inaccuracy of using this wearable, particularly in measuring core body temperature (Roossien et al. 2020, 2021). Consequently, we used the terminology of IET instead of core body temperature. Nevertheless, the IET is a good proxy of the core body temperature. Since the goal of our study is observing the physiological responses of HCW under different experimental conditions, this device is suitable as a monitoring tool for effects caused by thermal stress. Furthermore, the potential measurement error due to wind factor was likely minimized due to controlled experimental environment in the climate chamber.
Strength and limitations
To our knowledge, this is the first experimental study concerning the heat stress measurement by conducting simulations of the HCW-related activities in a controlled climatic environment. Besides supporting existing knowledge, this study provides valuable information about planning heat stress experiments using realistic but controlled conditions. Furthermore, the feasibility of using wearables to assess heat stress was demonstrated. A limiting factor is the temperature measurement in the ear, which is a proxy of the core body temperature. However, we considered this more feasible and non-invasive compared to other methods for the determination of the core body temperature. Furthermore, data quality of the ear sensors was impaired in cases when the sensor was not correctly placed in the ear or slipped out. This happened more frequently when the participants had to take off FFP2 masks. In this case, the experiment was stopped for a brief moment and a member of the study team reinserted the sensor. At last, the temperature and humidity in the climate chamber were not as stable as intended. However, the temperature difference between the settings was significantly higher than its variance. For relative humidity, the variance likely did not have an influence on the results.
Conclusions
In summary, our results suggest that the combination of internal heat stress triggered by high physical activity as well as external heat stress induced by increased environmental heat appears to be related to health and productivity losses of workers engaged in the healthcare sector. This situation can be worsened by wearing additional PPE, which was required in particular working conditions. This fact was supported by both participants’ perceptions and physiological measurements. All nations, particularly during a worldwide pandemic such as COVID-19, are dependent on HCW. Subsequently, their health and welfare are of paramount importance for sustained health stability. Unfortunately, HCW are likely at high risk of the health burden due to excessive occupational heat exposure. Lack of ventilation or non-air-conditioning building, as it is common in Germany, can aggravate this situation. As a consequence, adequate cooling provisions or other mitigation strategies should be implemented in order to reduce potential heat strain in HCW (Foster et al. 2020a; Lou et al. 2021; Bongers et al. 2022). Further research concerning the current and future risks of occupational heat exposure is crucial to develop comprehensive evidence-based policies for protecting HCW from the adversities of heat stress. We hope that the results of this study will help policymakers establishing appropriate interventions based on HCW’s work-related health hazards due to heat stress.
Availability of data and material
The data can be made available upon reasonable request.
References
an der Heiden M, Muthers S, Niemann H, et al (2019) Estimation of heat-related deaths in Germany between 2001 and 2015. Bundesgesundheitsblatt - Gesundheitsforsch - Gesundheitsschutz. https://doi.org/10.1007/s00103-019-02932-y
Arbury S, Jacklitsch B, Farquah O et al (2014) Heat illness and death among workers - United States, 2012–2013. MMWR Morb Mortal Wkly Rep 63:661–665
Bisolli P, Deutschländer T, Imbery F, et al (2019) Hitzewelle Juli 2019 in Westeuropa - neuer nationaler Rekord in Deutschland. https://www.dwd.de/DE/leistungen/besondereereignisse/temperatur/20190703_bericht_juni2019.pdf?__blob=publicationFile&v=2. Accessed 12 Feb 2022
BMAS (Bundesministerium für Arbeit und Soziales (German Federal Ministry of Labour and Social Affairs)) (2022) Technische Regeln für Arbeitsstätten (ASR): A3.5: Raumtemperatur. https://www.baua.de/DE/Angebote/Regelwerk/ASR/pdf/ASR-A3-5.pdf?__blob=publicationFile&v=5
Bolton S, Cave N, Cogger N, Colborne GR (2021) Use of a Collar-Mounted Triaxial Accelerometer to Predict Speed and Gait in Dogs. Anim an Open Access J from MDPI. https://doi.org/10.3390/ani11051262
Bonato P (2010) Wearable sensors and systems. From enabling technology to clinical applications. IEEE Eng Med Biol Mag Q Mag Eng Med Biol Soc 29:25–36. https://doi.org/10.1109/MEMB.2010.936554
Bongers CCWG, de Korte JQ, Zwartkruis M, Levels K, Kingma BRM, Eijsvogels TMH (2022) Heat Strain and Use of Heat Mitigation Strategies among COVID-19 Healthcare Workers Wearing Personal Protective Equipment-A Retrospective Study. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph19031905
Burgos CP, Gärtner L, Ballester MAG et al (2020) In-Ear Accelerometer-Based Sensor for Gait Classification. IEEE Sens J 20:12895–12902. https://doi.org/10.1109/JSEN.2020.3002589
DGAUM (2012) Deutsche Gesellschaft für Arbeitsmedizin und Umweltmedizin e.V. (DGAUM) Leitlinie Arbeit unter klimatischer Belastung: Hitze. 1–22
Dorman LE, Havenith G (2009) The effects of protective clothing on energy consumption during different activities. Eur J Appl Physiol 105:463–470. https://doi.org/10.1007/s00421-008-0924-2
Ebi KL, Hasegawa T, Hayes K, et al (2018) Health risks of warming of 1.5 °c, 2 °c, and higher, above pre-industrial temperatures. Environ Res Lett. https://doi.org/10.1088/1748-9326/aac4bd
Eggenberger P, MacRae BA, Kemp S et al (2018) Prediction of Core Body Temperature Based on Skin Temperature, Heat Flux, and Heart Rate Under Different Exercise and Clothing Conditions in the Heat in Young Adult Males. Front Physiol 9:1–11. https://doi.org/10.3389/fphys.2018.01780
Ellebrecht DB, Gola D, Kaschwich M (2022) Evaluation of a Wearable in-Ear Sensor for Temperature and Heart Rate Monitoring: A Pilot Study. J Med Syst. https://doi.org/10.1007/s10916-022-01872-6
Foster J, Hodder SG, Goodwin J, Havenith G (2020a) Occupational Heat Stress and Practical Cooling Solutions for Healthcare and Industry Workers During the COVID-19 Pandemic. Ann Work Expo Heal 64:915–922. https://doi.org/10.1093/annweh/wxaa082
Foster J, Hodder SG, Lloyd AB, Havenith G (2020b) Individual Responses to Heat Stress: Implications for Hyperthermia and Physical Work Capacity. Front Physiol. https://doi.org/10.3389/fphys.2020.541483
Goel N, Basner M, Rao H, Dinges DF (2013) Circadian rhythms, sleep deprivation, and human performance. Prog Mol Biol Transl Sci 119:155–190. https://doi.org/10.1016/B978-0-12-396971-2.00007-5
Gostimirovic M, Novakovic R, Rajkovic J et al (2020) The influence of climate change on human cardiovascular function. Arch Environ Occup Health 75:406–414. https://doi.org/10.1080/19338244.2020.1742079
Haapalainen E, Laurinen P, Röning J, Kinnunen H (2008) Estimation of exercise energy expenditure using a wrist-worn accelerometer: A linear mixed model approach with fixed-effect variable selection. Proc-7th Int Conf Mach Learn Appl ICMLA 2008. https://doi.org/10.1109/ICMLA.2008.131
IPCC (2019) Climate Change and Land: an IPCC special report. Clim Chang L an IPCC Spec Rep Clim Chang Desertif L Degrad Sustain L Manag food Secur Greenh gas fluxes Terr Ecosyst 1–864
Krishnamurthy M, Ramalingam P, Perumal K et al (2017) Occupational Heat Stress Impacts on Health and Productivity in a Steel Industry in Southern India. Saf Health Work 8:99–104. https://doi.org/10.1016/j.shaw.2016.08.005
Lenzer B, Drozdek M, Sosa AV et al (2020) Hitzestress Im Krankenhaus Der Klin 49:14–21
Lou L, Chen K, Fan J (2021) Advanced materials for personal thermal and moisture management of health care workers wearing PPE. Mater Sci Eng R Rep 146:100639. https://doi.org/10.1016/j.mser.2021.100639
Mazlomi A, Golbabaei F, Farhang Dehghan S et al (2017) The influence of occupational heat exposure on cognitive performance and blood level of stress hormones: a field study report. Int J Occup Saf Ergon 23:431–439. https://doi.org/10.1080/10803548.2016.1251137
McMorris T, Swain J, Smith M et al (2006) Heat stress, plasma concentrations of adrenaline, noradrenaline, 5-hydroxytryptamine and cortisol, mood state and cognitive performance. Int J Psychophysiol off J Int Organ Psychophysiol 61:204–215. https://doi.org/10.1016/j.ijpsycho.2005.10.002
Notley SR, Flouris AD, Kenny GP (2018) On the use of wearable physiological monitors to assess heat strain during occupational heat stress. Appl Physiol Nutr Metab Physiol Appl Nutr Metab 43:869–881. https://doi.org/10.1139/apnm-2018-0173
Papalexiou SM, AghaKouchak A, Trenberth KE, Foufoula-Georgiou E (2018) Global, Regional, and Megacity Trends in the Highest Temperature of the Year: Diagnostics and Evidence for Accelerating Trends. Earth’s Futur 6:71–79. https://doi.org/10.1002/2017EF000709
Patel S, Park H, Bonato P et al (2012) A review of wearable sensors and systems with application in rehabilitation. J Neuroengineering Rehabil 9:1–17
Pfeiffer KA, Dowda M, McIver KL, Pate RR (2009) Factors related to objectively measured physical activity in preschool children. Pediatr Exerc Sci 21:196–208. https://doi.org/10.1123/pes.21.2.196
Ravindra K, Rattan P, Mor S, Aggarwal AN (2019) Generalized additive models: Building evidence of air pollution, climate change and human health. Environ Int 132:104987. https://doi.org/10.1016/j.envint.2019.104987
Roossien CC, Heus R, Reneman MF, Verkerke GJ (2020) Monitoring core temperature of firefighters to validate a wearable non-invasive core thermometer in different types of protective clothing: Concurrent in-vivo validation. Appl Ergon 83:103001. https://doi.org/10.1016/j.apergo.2019.103001
Roossien CC, Hodselmans AP, Heus R, Reneman MF, Verkerke GJ (2021) Evaluation of a Wearable Non-Invasive Thermometer for Monitoring Ear Canal Temperature during Physically Demanding (Outdoor) Work. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph18094896
Rowell LB (1974) Human cardiovascular adjustments to exercise and thermal stress. Physiol Rev 54:75–159. https://doi.org/10.1152/physrev.1974.54.1.75
Russo S, Sillmann J, Sippel S et al (2019) Half a degree and rapid socioeconomic development matter for heatwave risk. Nat Commun 10:1–9. https://doi.org/10.1038/s41467-018-08070-4
Schoierer J, Mertes H, Wershofen B, Böse-O’Reilly S (2019) Training modules on climate change, heat, and health for medical assistants and nurses in outpatient care. Bundesgesundheitsblatt - Gesundheitsforsch - Gesundheitsschutz 62:620–628. https://doi.org/10.1007/s00103-019-02942-w
Simister J, Cooper C (2005) Thermal stress in the U.S.A.: Effects on violence and on employee behaviour. Stress Heal 21:3–15. https://doi.org/10.1002/smi.1029
Steul K, Schade M, Heudorf U (2018) Mortality during heatwaves 2003–2015 in Frankfurt-Main – the 2003 heatwave and its implications. Int J Hyg Environ Health 221:81–86. https://doi.org/10.1016/j.ijheh.2017.10.005
Teng XF, Poon CCY, Zhang YT, Bonato P (2008) Wearable Medical Systems for p-Health. IEEE Rev Biomed Eng 1:62–74. https://doi.org/10.1109/RBME.2008.2008248
Trenberth KE (2018) Climate change caused by human activities is happening and it already has major consequences. J Energy Nat Resour Law 36:463–481. https://doi.org/10.1080/02646811.2018.1450895
UNEP (2021) Climate Change | United Nations. United Nations Environ. Program (UNEP).
Van Dongen HPA, Olofsen E, Dinges DF, Maislin G (2004) Mixed-Model Regression Analysis and Dealing with Interindividual Differences. In: Numerical Computer Methods, Part E. Academic Press, pp 139–171
van Rüth P, Schönthaler K, von Andrian-Werburg S, Buth M (2019) Monitoringbericht zur Deutschen Anpassungsstrategie an den Klimawandel. 276. https://www.umweltbundesamt.de/sites/default/files/medien/1410/publikationen/das_monitoringbericht_2019_barrierefrei.pdf. Accessed 21 Nov 2021
Vicedo-Cabrera AM, Scovronick N, Sera F et al (2021) The burden of heat-related mortality attributable to recent human-induced climate change. Nat Clim Chang 11:492–500. https://doi.org/10.1038/s41558-021-01058-x
Acknowledgements
The authors thank Mrs. Christina Feldmaier from the State Vocational School for Nursing at the University Hospital of the LMU Munich (Staatliche Berufsfachschule für Krankenpflegehilfe am Klinikum der Universität München) for advising and providing the appropriate healthcare activity scenarios in the climate chamber.
Funding
Open Access funding enabled and organized by Projekt DEAL. This study was funded by the Berufsgenossenschaft für Gesundheitsdienst und Wohlfahrtspflege–BGW (project number FF_1486).
Author information
Authors and Affiliations
Contributions
Conceptualization: SB-O’R, SR; methodology: RW, VD, DK, HD, SR; formal analysis and investigation: RW, VD, DK, SR; writing—original draft preparation: RW. writing—review and editing: RW, CQ, DK, HD, DN, SB-O-R, SR; resources: SR; supervision: DN, SBo-O-R, SR.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethical approval
The study was carried out in accordance with the Code of Ethics of the Declaration of Helsinki for experiments involving human subjects and was reviewed and approved by the ethics committee of the Ludwig Maximilians University of Munich (#21-0197).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This work is part of a doctoral thesis.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wibowo, R., Do, V., Quartucci, C. et al. Effects of heat and personal protective equipment on thermal strain in healthcare workers: part B—application of wearable sensors to observe heat strain among healthcare workers under controlled conditions. Int Arch Occup Environ Health 97, 35–43 (2024). https://doi.org/10.1007/s00420-023-02022-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-023-02022-2