Abstract
Objectives
To investigate the annual rate of NIHL in Israel, a modern economy with relatively low industrial hazardous noise exposure. To review international protocols of hearing surveillance. To recommend an effective, efficient, hearing screening frequency protocol.
Methods
A historical cohort study was conducted. Audiometric surveillance data from the Jerusalem occupational medicine registry of male employees in various industries from 2006 to 2017 were used. Mean individual annual threshold shifts simulating 1–8 checkup interval years were calculated. Joinpoint regression analysis was used to assess the interval in which the slope of the calculated ATS variability moderates significantly.
Results
A total of 263 noise-exposed workers and 93 workers in the comparison group produced 1913 audiograms for analysis. Among the noise-exposed workers, using the 1–4 kHz average, threshold shifts stabilized from 3 years onwards at around 1 dB per year in all age groups and 0.83 dB in the stratum younger than 50 years. No enhanced decline was detected in the first years of exposure.
Conclusion
Although most countries conduct annual hearing surveillance, hearing threshold shifts of noise-exposed workers become more accurate and show less variability when calculated at 3-year checkup intervals onwards than shorter intervals. Since margins of errors of the test method are much larger than the annual shift found, screening schedule that enables each subsequent test to identify a real deterioration in hearing is necessary. Triennial audiometric screening would be a better surveillance frequency for noise-exposed workers younger than 50 years of age in the category of 85–95 dBLAeq,8 h without other known risk factors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Epidemiology
Occupational noise-induced hearing loss (NIHL) is a significant cause of potentially avoidable morbidity and one of the most prevalent work-related health hazards internationally, accounting for 16% of hearing loss (HL) in adults (Chadambuka et al. 2013; Lie et al. 2016; Rabinowitz 2012; Themann and Masterson 2019; Tikka et al. 2017). Pre-COVID-19, hearing impairment accounted for 10% of all non-fatal occupational diseases, and was ranked the second most common occupational condition reported in the US (United States Department of Labor Bureau of Labor Statistics 2019). Approximately 14–20% of workers in the US, Europe, and Australia are exposed to hazardous noise in their occupational settings and 16% of the exposed develop significant hearing impairments (Rabinowitz et al. 2011; Themann and Masterson 2019). Hazardous noise can be defined as sound intensity level, frequency, and duration above a particular exposure limit, thereby potentially harmful to hearing (Themann and Masterson 2019). Many countries, including Israel, use 85 dBLAeq,8 h (A-weighted, equivalent continuous sound over an 8-h period) as a cut-off for hazardous occupational noise which requires hearing surveillance for the exposed workers (Arenas and Suter 2014; Israel Ministry of Economy and Industry Labour 1984). A noise level of 85 dBLAeq,8 h represents 8% of acceptable excess risk over a 40-year working lifetime (NIOSH 1998; Bruce et al. 2010; Siegel 2019).
In Israel, about 24% of workers reported being exposed to hazardous noise levels at some point during their work life (Israel Central Bureau of Statistics (ICBS) 2016). However, Israel, like Europe, USA and other developed countries, is undergoing labor market changes characterized by transforming conservative industry to high technology and service sectors (Hartmann et al. 2021). As a result, fewer workers are exposed to hazardous noise, and those who are exposed experience relatively lower intensity levels. Nevertheless, occupational NIHL is still the most commonly reported occupational disease in Israel, constituting about 46% of all such disorders recorded in the National Registry of Occupational Diseases (Meiman et al. 2019).
Pathophysiological progression
NIHL is characterized by more prominent reduction at 3–6 kHz “noise sensitive area” compared to the surrounding frequencies (i.e., 2 or 8 kHz), with a typical antecedent, 4 kHz notch (Lie et al. 2016; Liebenberg et al. 2021; Mirza et al. 2018). In the early phases, noise affects high frequencies which are indiscernible in daily communication (Liebenberg et al. 2021; Mirza et al. 2018; Tikka et al. 2017). Hence, periodic hearing screening is vital for detecting subclinical changes (EU-OSHA 2005; Lie et al. 2016; Silva et al. 2022; Verbeek et al. 2014). Previous studies have demonstrated accelerated hearing deterioration among noise-exposed workers aged 50 and above, due to additional factors such as presbycusis (age-related hearing loss; Lie et al. 2016; Liebenberg et al. 2021). In addition, there is evidence in the literature for accelerated occupational NIHL in first years of occupational noise exposure, ranging from the first 3 to 15 years of exposure (Cantley et al. 2019; Mirza et al. 2018). Individual susceptibility to the higher rates of hearing deterioration in the first years of exposure vary; however, the reasons for the variation are not clearly established (Cantley et al. 2019).
Hearing conservation policies
Annual hearing surveillance is a major component of occupational hearing conservation programs and it is the default protocol used in many western countries (Davies et al. 2008; EU-OSHA 2005; Hannah et al. 2016), as demonstrated in Table 1.
In Israel, annual hearing surveillance is mandatory, under the Safety at Work Ordinance (Occupational hygiene and health of workers exposed to noise 1984), and applied to all workers exposed to hazardous occupational noise. Unlike most countries, the surveillance is covered by the National Health Insurance and provided universally without co-payment from the employee or employer, within the larger framework of the national healthcare system by one of the four not-for-profit Health Maintenance Organizations (HMOs) covering the entire civilian population (Rinsky-halivni et al. 2020).
Threshold shifts
The literature demonstrated that the rate of annual hearing deterioration (“annual threshold shift”) among noise-exposed workers is approximately 1 dB/year at higher frequencies (Brickner and Carel 2005; Franks 2001; Hetu et al. 1990; Lie et al. 2016; Silva et al. 2022). However, there is measurement variability in audiometric tests as ± 5 dB steps are used to establish hearing thresholds. The margin of error can be notable especially in field conditions where there is lower control of conditions (Barlow et al. 2015). Therefore, the warning value of significant/standard threshold shift (STS) that requires further medical workup and application of control measures is higher than the random audiometric test variation (Dobie 2005; Tikka et al. 2017). Some of the common recommendations regarding the STS criterion, ranging between 10 and 15 dB, are shown in Table 1.
Study aims
The standard annual testing frequency may not reliably detect the annual threshold shift. This study aimed to investigate the annual rate of clinical deterioration of hearing of workers in Israel. Second, the study aimed to propose an effective, efficient, hearing screening frequency protocol for NIHL screening in noise-exposed workers in the context of modern labor markets based on empiric data.
Methods
Study population
Male workers, aged 18 years and above at first audiogram, from workstations certified to be hazardously noisy were eligible for inclusion in the noise-exposed group. Employees in noisy workstations with audiometric records of at least seven checkups and a 1-year gap between examinations were included in the exposed group. Participants met the eligibility criteria for the reference group if they were employed as crane operators, participating in mandatory occupational medical monitoring at a Jerusalem district HMO between 2006 and 2017, not concomitantly exposed to hazardous noise, and had at least four audiometric tests.
Crane operators were selected as a reference group as their workstations are verified to be non-exposed to occupational hazardous noise. Based on previous studies of tower and truck-mounted crane operators, it was assumed that the referent participants were exposed to an average of 76 dBLAeq,8 h (Sellappan and Janakiraman 2014). Their operation license requires them to be medically fit through medical monitoring, which includes, inter alia, hearing tests.
Women were excluded since more than 96% of the data available were from male workers. Workers with obvious cases of non-NIHL, e.g., documented chronic conductive HL or history of other causes of hearing impairment and those with profound degree of sensorineural HL at baseline audiogram were excluded. Based on previous studies, a ratio of exposed: non-exposed of approximately 3:1 and a standard deviation of 5 dB were used to estimate sample size for comparing mean threshold shifts between the groups (Lutman et al. 2008).
Data collection and study variables
Data on workers’ sociodemographic characteristics (age, gender, ethnicity, rural/urban residential area), occupational variables (industry, years in service hazardous noise-exposure history and duration, noise level of work environment, ototoxic concomitant occupational exposures), information on potential clinical factors known to be correlated with impaired hearing (diabetes, hypertension, smoking status, and medications) (Sliwinska-Kowalska 2020) and consecutive hearing monitoring results were obtained from the electronic medical records (EMRs) of the Jerusalem occupational medicine clinic between 2006 and 2017. Information on noise exposure levels of workstations in the plants where participants were employed was obtained from electronic files of the occupational medicine clinic derived from the Ministry of Labor factories' registry. A certified hygienist assessed noise level, as required by the Israeli law, according to international organization for standardization (ISO9612 standards) using personal monitoring approach sound level meters or noise dosimeters with personal monitoring approach. Mandatory workstation-based noise exposure measurements during the study period were used to assess exposure levels of the exposed group’s workplaces.
Baseline and consecutive screening hearing monitoring audiograms in the EMRs were conducted by trained nurses or audiologists, then analyzed by a certified occupational physician who decided on required investigation. Audiometry was performed following American National Standards Institute (ANSI standards) described in supplemental table S1, which includes additional operational definitions. The bilateral mean of 1–4 kHz and 0.5–2 kHz frequencies was used for analyses. Audiograms were omitted if unlikely threshold values with unusual patterns that suggest the presence of testing or patient recognition errors were noted. Confirmatory audiograms repeated within a 9-month period within the same year were averaged out. The North American Industry Classification System (NAICS) was used to classify all workstations into four major service industries, i.e., manufacturing, services, transport and warehousing, and construction industries. Chronic health conditions were recorded both if first diagnosed in the EMRs during follow-up and at baseline as diabetes are often not clinically diagnosed until a decade after onset (Baker et al. 2018; Ohishi 2018).
Data analysis
Data were analyzed with SPSS version 26 (IBM Corp., Armonk, NY). Bivariate analyses of associations between the characteristics of study subjects in the reference and noise-exposed group were evaluated using a Chi-square test. Two-sided tests of significance were used, and statistical significance was set at P < 0.05. Data were stratified by age (50 years and above, and below 50 years), given the unbalanced age of exposed and referent group and the association between age and HL. Presbycusis affecting the frequency range tested through occupational pure tone audiometry generally occurs around and after age 50, hence selection of 50 years as the cut-off (Arvin et al. 2013; Lie et al. 2016).
The mean noise exposure (2006–2017) of each of the plants where the noise-exposed participants worked was calculated by averaging the 8-h time-weighted average (TWA) noise doses of all measured workstation in the workplace. Noise exposure measurements from all workstations and factories were first converted to percentage dose as they could not be directly averaged in the logarithmic scale. A dose of 100% is equivalent to the permissible noise exposure (threshold limit value—TLV) of 85 dBLAeq,8 h and a 3 dB-exchange rate was used to calculate dose. Noise levels were presented in both noise doses scale and by conversion back to the logarithmic A-weighted scale in decibels.
Mean individual threshold shifts for each worker (1–4 kHz) in time periods of 1 year, 2 years, 3 years, up to 8 year intervals between checkups were calculated simulating different surveillance intervals of each study subject to maximize data usage (see Fig. 1 for schematic diagram). For each worker, pure tone average (PTA) thresholds of the latter year were subtracted from the former year according to desired time interval. For each time interval, all possibilities were then averaged to obtain the personal threshold shift mean. Afterward, the threshold shifts of each given time interval per person were summed together and divided by the number of study subjects and by the interval years to get a mean annual threshold shift (ATS) for each time interval. Standard deviations of the within-person means were calculated across all thresholds shifts of each time interval of every individual. Afterward, based on the within-person means, the between-person standard deviations were computed for the various time intervals. See equation S1 for calculation formulas and examples.
We stratified for years in service by assessing noise-exposed workers (with up to three years) and following them up to 12 years, giving a maximal range of 15 years, which is in accordance with the sparse evidence of accelerated occupational NIHL in the first 10–15 years employment (Kamal et al. 1989). Employees with 0–3 years in service at baseline were compared to those with longer years of exposure.
A Joinpoint regression analysis was used to assess timing of significant magnitude change in trends of mean ATS between increasing audiological checkups intervals, toward a zero slope. It indicates that mean ATS values are similar when calculated between consecutive time intervals, and therefore more accurate. Mean threshold shifts calculated for annual changes, from annual checkup interval up to 8 years, were used to compute the curves and Joinpoints utilizing Monte Carlo method set to 10,000 permutations and considering the existence of autocorrelation (Joinpoint Regression Program version 4.9.1.0, National Cancer Institute, Bethesda, Maryland). For each time interval, we calculated the coefficient of variation (standard deviation divided by the mean) to investigate the relationship between the variability of mean ATS values obtained from the exposed workers when calculated for different time intervals between checkups. A Joinpoint for trend change was then sought to determine the dispersion trend changes along the increasing time intervals for ATS calculations. A flat trend of the slope represents similarity in dispersion of ATS among the noise-exposed participants.
Ethics
This study was approved by the ethics committee of Clalit Health Services. A waiver of informed consent was granted by the committee due the use of anonymous and de-identified retrospective data without access to contact information of participants.
Results
Participant characteristics
A total of 1913 audiograms from 356 male participants (263 noise exposed and 93 reference group of crane operators) were included for analyses. An average of 8.4 and 8 audiograms were obtained per participant (noise exposed and crane operator, respectively) for the 12-year period covering the years 2006–2017.
As shown in Table 2, age distribution was significantly different given that the referent workers, i.e., the crane operators are older in all stratas than the noise exposed. In addition, the proportion of workers belonging to Israel's Arab minority comprised 28% of the noise-exposed group, comparable to the 28.9% share of Arabs among the male workers in Jerusalem district (Israel Central Bureau of Statistics 2011). However, only 17% of crane operators were Arabs. The distribution of enrollment time, smoking status, residential area, diabetes, and ototoxic exposures was similar between the two groups. Age and hypertension are highly associated, hence the likely explanation for the significant difference in the distribution of hypertension with the reference group (older) having higher incidence (Lie et al. 2016). Distribution of ototoxic drugs, parallel exposure to chemicals were assessed; however, the number of study subjects in the groups was too small for further analyses.
Table 3 shows hearing screening status at baseline, or on first computerized follow-up in 2006. Across all variables, the exposed group of workers showed a trend of higher percentages with hearing impairment compared to the crane operators, especially among oldest and longest serving subcategories. Hearing status distribution by ethnicity at baseline showed significant differences between Jews and Arabs, with Jews having higher HL percentages in both referent and exposed groups, explained by the relative older age of Jewish workers (P < 0.001, data not shown).
Noise level exposure during the research period
Noise-exposed participants worked in plants with a mean of 91.6 dBLAeq,8 h (459% dose), 5% trimmed mean of 90.3 dBLAeq,8 h (340%), median of 88.6 dBLAeq,8 h (230%) for the period relevant to the study (IQR 85.4–91.4 dBLAeq,8 h) (supplemental figure S1). In total, 9.4% of the factories had mean noise levels above 95 dBLAeq,8 h (1000% dose), while 12.5% were within the acceptable exposure limit of 85 dBLAeq,8 h (up to 100% dose).
Annual threshold shifts stratified by age
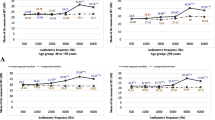
Given the significant differences in age distribution of exposed and referent groups, stratification by age was conducted (Table 4). Joinpoint among the younger than 50, exposed group (Fig. 2), located at mean ATS calculated in 4-year interval demonstrates significant changes in the slope (P = 0.01) that was moderated toward zero as checkup intervals increased. Among the reference group, an ATS trend change was evident when calculated at 3-year intervals onward. Mean ATS stabilized around 0.83 dB from 4-year test intervals among the exposed, slightly higher than the steady 0.65 dB in the reference group obtained from triennial interval and onward.
As opposed to the younger workers, a significant clear Joinpoint (homogenous hearing deterioration trend) was not obtained when ATS were calculated using consecutive multi-annual checkup intervals among noise-exposed workers aged 50 and above (Figure S2). Their annual hearing deterioration means oscillate around an ATS of about 1.15 dB (Table 4). In addition, the Joinpoint analysis in the older reference group demonstrated less stability in threshold shift trend along the sequential time intervals compared to younger crane operators. Therefore, further analyses were performed on the younger age group of below 50 years.
Figure 2 and Figure S2 demonstrate consistent pattern in the directions of the deviation from steady values in ATS obtained from higher test frequencies (annual and biennial): deviation toward higher average ATS in the exposed group and lower in the reference group.
Variability of annual change when calculating ATS in different hearing screening intervals
Figure 3 demonstrates that as the time interval between consecutive hearing checkups increased, the mean annual change (ATS) variability decreased, implying on improved accuracy. The moderation of the slope is seen from triennial interval onward. The mean coefficient of variation decreased from 5.39 (95% CI [4.82, 5.96]) for annual interval to 2.3 (95% CI [2.07–2.57])—a decrease in 58% for triennial interval. A Joinpoint located at 3-year interval with reduction in slope at lower test frequencies signifies the checkup frequency in which the variability decreases most substantially.
Joinpoint trend analyses of annual threshold shifts variability, represented by coefficient of variation (standard deviation divided by mean) according to sequential time intervals for calculating ATS among noise-exposed workers aged below 50 years at entry. As the time interval between consecutive hearing checkups increased, the mean annual change (ATS) variability decreased, implying improved accuracy
Annual threshold shifts stratified by duration of employment
To evaluate the noise-induced deterioration rate among newly exposed workers, further analysis of hearing threshold shift by years in service at entry was performed among noise-exposed workers below age 50 (Fig. 4). On average, the newly exposed group was 5 years younger relative to the more senior (33 versus 38, respectively). The comparison showed no significant differences at any time interval among participants with up to 3 years of exposure at baseline compared to the more senior workers and no accelerated NIHL among newer workers was demonstrated (P > 0.05 at all intervals between checkups, data not shown).
Mean annual threshold shifts calculated according to consecutive time intervals of hearing checkups in noise-exposed workers aged below 50 years at entry: newly exposed who had 0–3 years of service at baseline (N = 47), compared to senior workers who had more than 3 years of exposure at baseline (N = 127). Abbreviations: dB, decibel(s); ATS, annual threshold shifts. All T tests between newly exposed and veteran workers were non-significant (P > 0.05)
Discussion
According to our review, in Israel as well as in many other countries, it is customary to perform annual audiometric screening of noise-exposed workers and compare annual audiometry tests with the previous tests to calculate an ATS. Given the 5 dB margin of error when performing hearing tests and the slow rate of NIHL, threshold shift between annual audiometry tests might miss a real significant shift (STS) over a longer period or alternatively may produce an artifactual annual change leading to unnecessary medical investigations. This pioneering follow-up study, using Joinpoint of threshold shift means and variability of different intervals of hearing screening for the first time, assessed the accurate annual rate of occupational NIHL and the frequency of follow-up required to detect HL when comparing a test to its predecessor.
1–4 kHz rate of annual decline stratified by age and years in service
Our findings revealed that among the noise-exposed workers, using the 1–4 kHz average, the threshold shifts stabilized from 3 years onwards at around 1 dB per year in all age groups and 0.83 dB in the stratum younger than 50 years. The annual deterioration rate of 1 dB resembles previous studies (Brickner and Carel 2005; Hetu et al. 1990; Lie et al. 2016; Silva et al. 2022). For the reference group, age stratification demonstrated an annual hearing threshold shift at 3-year intervals onwards, stabilized at 0.65 dB among younger workers aged below 50. Nevertheless, we could not characterize a clear trend of stabilization of the ATS along the multi-annual test intervals within the older exposed and reference sub-groups aged 50 and above. The instability of the threshold shift averages is probably due to the strong non-linear age effect on HL. However, we were able to estimate the average annual HL value among the exposed workers at 1.15 dB.
Another critical element was to assess threshold shifts in the first years of exposure according to evidence in the literature, based on ISO 1999:1990 (International Organization for Standardization) nomograms or unprotected excessive noise exposure levels, for accelerated rate of HL, which might necessitate more frequent surveillance in the early post-exposure period (International Organization for Standardization 1990; Kamal et al. 1989; Keatinge and Laner 1958; Lie et al. 2016). In the UK and in some provinces of Canada, annual hearing tests are conducted in the first years of employment followed by a bi-/triennial surveillance (EU-OSHA 2005; Government of Alberta 2017; OHS Insider 2021). Our results, however, did not support an enhanced decline in the first years of service compared with those later years of exposure. An explanation for this difference could be that new workers are effectively using personal protective equipment, and are aware of the risk of hazardous noise and are younger.
Our findings corresponded with the evidence that the 10 years of exposure to a daily average of 85–90 dBLAeq,8 h results in an average threshold shift of 4–9 dB at 1–4 kHz and first 5 years with 3 dB (Lie et al. 2016; Silva et al. 2022).
Hearing loss in modern labor market settings
The study results revealed that annual hearing threshold shifts are higher in the noise-exposed group of workers as compared to the reference group despite mandatory use of hearing protection equipment, and improved engineering control measures in the last decades which led to relatively low (median of 88.6 dBLAeq,8 h) exposure levels in factories in the Jerusalem district. The findings suggest that the currently legislated hearing conservation practices and monitoring systems are imperfect in preventing NIHL, which remains the leading occupational disease reported to the registry in Israel. Consequently, further strategies are required to improve risk control among the numerous workers exposed to hazardously noisy occupational settings.
Surveillance frequency
The degree of change expected between tests annually is much smaller than the existing variability due to test conditions and hearing testing techniques of ± 5 dB steps, as reflected by the large coefficient of variation and weighted annual standard deviations in both exposed and reference groups. This is more pronounced among the noise-exposed workers, whose hearing testing is frequently conducted in the factory area, by different examiners and not always after the recommended noise-exposure avoidance time, that can result in the transient temporary threshold shift (TTS) (Codling and Fox 2013). As per our findings, threshold shifts calculated using testing intervals of 1 and 2 years are unreliable given the tendency for a positive error in exposed groups, and negative error in non-exposed groups. In effect, hearing threshold shifts calculated at intervals of at least 3 years reflect more accurately the exact annual decline rate of the employee. Reduced measurement error when calculating annual rate of deterioration over longer intervals between hearing tests might explain the stabilization in mean ATS values. Nevertheless, findings are less clear regarding older workers, strongly influenced by the non-linear rate of deterioration due to age. Researchers have not yet succeeded in finding an age correction mechanism for workers over the age of 60 to obtain the real rate of hearing deterioration due to noise exposure (Dobie and Wojcik 2015). In practice, the OSHA correction is only until age 60 (Dobie and Wojcik 2015).
An annual testing frequency is costly in terms of money, resources, and time of the health system, employees and employers, potentially reducing compliance (Windapo 2013). Therefore, there is a need to balance measurement accuracy with compliance and the risk of missing STS, signifying potential NIHL that needs to be adressed to protect workers’ health.
Given the issues highlighted in our study concerning annual screening, the triennial method whereby hearing tests are conducted at 3-year intervals is recommended unless workers are of older age, or a hearing problem or accelerated HL is detected. A similar protocol is currently adopted by the British HSE, though we were not able to discern the evidence base of this practice. However, our findings did not support frequent surveillance in the initial years of employment as the HSE protocol (Codling and Fox 2013). The average expected annual change of 0.8 dB, as we observed among noise-exposed workers younger than age 50, suggests that the intervals between each subsequent test should be considered so as to identify a significant and real deterioration in hearing. In this way, unnecessary medical investigations and unjustified displacement of employees from work to comply with legislation can be avoided. The South African regulations use the baseline audiogram obtained at the start of a worker’s work life as the reference to which all future periodic audiograms are evaluated (Grobler et al. 2020). Continuously referring to the baseline audiogram (which is periodically revised after a STS), together with spaced assessments, could improve accuracy and effectiveness of hearing assessments.
Other considerations such as risk factors for HL and primarily age of workers should be factored in (Codling and Fox 2013; Themann and Masterson 2019) and further studied in relation to desired screening frequency. However, for the average healthy worker, there is no additional benefit in conducting annual tests over triennial tests. Since frequent surveillance is recommended for highly exposed workers in some countries (e.g., safe work Australia for exposure greater than 100 dBLAeq,8 h), we recommend on lower surveillance frequency to be performed for those who are exposed to relatively lower noise levels (Franks 2001; Safe Work Australia 2018).
Strengths and limitations
To the best of our knowledge, no previous studies have examined the rate of occupational NIHL using different time intervals to establish an evidence-based hearing screening frequency protocol for different noise-exposed strata. Additionally, the computerized dataset enabled the use of comprehensive data which included a wide range of demographic, clinical, and occupational parameters compared to subjective questionnaires frequently used in occupational surveillance. The universal occupational medicine services in Israel (free of co-pay) allow research to include workers from all noise-exposed work sectors. Furthermore, the record-keeping practice enables inclusion in the dataset of many repeat investigations for each worker with the same instruments and test operators, enabling accurate calculations of average threshold shifts. Selection of workers with multiple checkups minimized the risk of attrition. In addition, the calculated simulation of different surveillance intervals allowed optimal use of the available data. Referral of all noise-exposed workers for hearing conservation surveillance is mandated by law and not subject the discretion of the workers or the employer, thereby minimizing bias. This is a “real life” cohort; therefore, practical recommendations can be drawn from the study.
Limitations include the lack of data regarding prior exposure to noise among crane workers who may have held other job titles in the construction industry before becoming crane operators; however, we screened all participants at baseline for severe-profound HL. In addition, exposure misclassification by employers (who may classify an unexposed worker as exposed and refer for hearing monitoring or a crane operator who works in parallel with exposure to noise, not referred for monitoring), cannot be ruled out. We were limited by a small sample size in the reference group since non-exposed workers are not regularly screened for HL. Moreover, less stringent measures on hearing screening frequency in the reference group of crane operators resulted in missing tests. The reference group although older, might introduce a “healthy worker effect” bias, including better hearing since it is a part of their fitness for duty requirements (Chowdhury et al. 2017). We, therefore, expected the workers in the reference group to be more incentivized to demonstrate better results of hearing tests. In contrast, noise-exposed workers might make lesser effort due to a possible secondary gain motive for work injury compensation. Nevertheless, average of threshold shifts along wider intervals may reduce effects of worker effort, and this may sharpen the difference in threshold shifts between the two groups. Moreover, it is possible that some exposed workers were not tested in ideal conditions (in the factory, sometimes exposed recently). In addition, we could not obtain the specific exposure status of each worker but rather used the factories mean to get a notion on the general noise exposure level of the workers in the cohort. Better characterization of the individual noise level would enable better tailoring surveillance recommendations. We excluded women from our study due to small numbers. Previous studies demonstrated higher susceptibility among males to noise-induced hearing shifts. However, our findings were comparable with studies where participants were of both sexes possibly due to most studies reporting higher proportions of male employees in the noisy industries (Lie et al. 2016). Further studies are needed to include occupationally noise-exposed women.
In conclusion, this study for the first time provides evidence for the accuracy of annual hearing threshold shifts of noise-exposed workers when calculated at 3-year interval onwards. The accurate ATS is at about 0.8 dB shift annually among workers below 50 years in the context of modern industry. Margins of errors of the test method are much larger than the ATS found, thus requiring a screening schedule that enables each subsequent test to identify a significant and real deterioration in hearing. Worse than that—missing a gradual deterioration that would not be revealed by annual testing, especially if the comparison is with the previous annual test. In practice, for the relatively low category of noise-exposed workers (85–92 dBLAeq,8 h) as in Jerusalem district in Israel, a triennial audiometric screening frequency method would be a clinically feasible surveillance method for workers without other known risk factors and enhance compliance.
Further studies are recommended to replicate the findings using a larger sample size and different strata of noise exposures investigating female and Arab minority workers as well as participants with additional risk factors for HL. As a first step, and pilot research, it is advisable to consider calculating 3-year intervals of each exposed worker attending the traditional annual hearing surveillance to enhance informed decision-making for screening. Moreover, it is worthwhile to add, to the screening policy, the use of long-term averages of threshold shifts for each worker not to miss STS, instead of using threshold shifts between adjacent checkups, as customary in Israel and other countries.
Data availability
The data that support the findings of this study are available from Clalit Health Services, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are, however, available from the authors upon reasonable request and with permission of Clalit Health Services.
Abbreviations
- ANSI:
-
American National Standards Institute
- dB:
-
Decibel(s)
- dBA:
-
Decibel(s), sound pressure level, A-weighted
- 85dBLAeq , 8 h :
-
85 Decibels, A-weighted, for 8-h time-equivalent continuous sound level
- HL:
-
Hearing loss
- Hr:
-
Hour(s)
- Hz:
-
Hertz
- kHz:
-
Kilohertz
- NIHL:
-
Noise-induced hearing loss
- NIOSH:
-
National Institute for Occupational Safety and Health
- OSHA:
-
Occupational Safety and Health Administration
- SNHL:
-
Sensorineural hearing loss
- STS:
-
Significant or standard threshold shift
- TWA:
-
Time-weighted average
References
Arenas J, Suter A (2014) Comparison of occupational noise legislation in the Americas: an overview and analysis. Noise Health 16(72):306–319. https://doi.org/10.4103/1463-1741.140511
Arvin B, Prepageran N, Raman R (2013) “High frequency presbycusis”—is there an earlier onset? Indian J Otolaryngol Head Neck Surg 65(3):480–484. https://doi.org/10.1007/s12070-011-0356-x
Baker R, Wilson A, Nockels K, Agarwal S, Modi P, Bankart J (2018) Levels of detection of hypertension in primary medical care and interventions to improve detection: a systematic review of the evidence since 2000. BMJ Open 8(3):e019965. https://doi.org/10.1136/bmjopen-2017-019965
Barlow C, Davison L, Ashmore M (2015) Variation in tone presentation by Pure Tone Audiometers: the potential for error in screening audiometry. In: Proceedings of Euronoise 2015, Maastricht, The Netherlands.
Brickner D, Carel R (2005) Annual rate of development of noise induced hearing loss in exposed workers. Harefuah (hebrew) 144(10):692–695
Bruce RD, Bommer AS, Hart NW, Riegel KA (2010) Safe lifetime occupational noise exposure – 1 LONE (lifetime occupational noise exposure). J Acoust Soc Am 127:1881–1881. https://doi.org/10.1121/1.3384670
Cantley LF, Galusha D, Slade MD (2019) Early hearing slope as a predictor of subsequent hearing trajectory in a noise-exposed occupational cohort. J Acoust Soc Am 146(5):4044–4050. https://doi.org/10.1121/1.5132542
Chadambuka A, Mususa F, Muteti S (2013) Prevalence of noise induced hearing loss among employees at a mining industry in Zimbabwe. Afr Health Sci 13(4):899–906. https://doi.org/10.4314/ahs.v13i4.6
Chowdhury R, Shah D, Payal AR (2017) Healthy worker effect phenomenon: revisited with emphasis on statistical methods— a review. Indian J Occup Environ Med 21(1):2–8. https://doi.org/10.4103/ijoem.IJOEM_53_16
Codling A, Fox D (2013) Current practice in health surveillance for noise HSE. https://www.hse.gov.uk/research/rrpdf/rr966.pdf. Accessed Aug 15 2022
Davies H, Marion S, Teschke K (2008) The impact of hearing conservation programs on incidence of noise-induced hearing loss in Canadian workers. Am J Ind Med 51(12):923–931. https://doi.org/10.1002/ajim.20634
Dobie RA (2005) Audiometric threshold shift definitions: simulations and suggestions. Ear Hear 26(1):62–77. https://doi.org/10.1097/00003446-200502000-00006
Dobie RA, Wojcik NC (2015) Age correction in monitoring audiometry: method to update OSHA age-correction tables to include older workers. BMJ Open 5(7):e007561. https://doi.org/10.1136/bmjopen-2014-007561
EU-OSHA (2005) European agency for safety and health at work: reducing the risks from occupational noise. Belgium, pp 1–88.
Franks JRW (2001) Hearing measurement. In: Goelzer B, Hansen CH, Sehrndt GA (eds) Occupational exposure to noise: evaluation, prevention and control. World Health Organization, Geneva, pp 183–232
Government of Alberta (2017) Audiometric testing: information for employers and workers. https://open.alberta.ca/dataset/3ee0e2ed-45b0-4f77-969d-33c554814374/resource/ebd22545-59e3-4334-8b74-25a76dff4fab/download/ohs-bulletin-hs005.pdf Accessed Aug 15 2021
Grobler LM, Swanepoel W, Strauss S, Becker P, Eloff Z (2020) Occupational noise and age: a longitudinal study of hearing sensitivity as a function of noise exposure and age in South African gold mine workers. S Afr J Commun Disord 67(2):e1–e7. https://doi.org/10.4102/sajcd.v67i2.687
Hannah L, Page W, Mclaren S (2016) A review of occupational noise in New Zealand. New Zealand Acoustics 29(1):4–26
Hartmann D, Zagato L, Gala P, Pinheiro FL (2021) Why did some countries catch-up, while others got stuck in the middle? Stages of productive sophistication and smart industrial policies. Struct Change Econ Dyn 58:1–13. https://doi.org/10.1016/j.strueco.2021.04.007
Hetu R, Quoc HT, Duguayf P (1990) The likelihood of detecting a significant threshold shift among noise-exposed workers subjected to annual audiometric testing. Ann Occup Hyg 34:361–370. https://doi.org/10.1093/annhyg/34.4.361
International Organization for Standardization (1990) Acoustics: determination of occupational noise exposure and estimation of noise-induced hearing impairment. In: International organization for standardization. https://www.iso.org/standard/45103.html Accessed Aug 15 2021
Israel Central Bureau of Statistics (ICBS) (2011) Labor force surveys 2010. Israel Central Bureau of Statistics Publishing
Israel Central Bureau of Statistics (ICBS) (2016) Israel central bureau of statistics (ICBS) social survey: quality of employment and working conditions. In: https://www.health.gov.il/publicationsfiles/occupationaldiseases2012_2013.pdf Accessed Aug 14 2020–2021.
Israel Ministry of Economy and Industry Labour (1984) Israel Workplace safety Regulations (Occupational hygiene and health of workers exposed to noise). 5739:7.
Kamal AAM, Mikael RA, Faris R (1989) Follow-up of hearing thresholds among forge hammering workers. Am J Ind Med 16(6):645–658. https://doi.org/10.1002/ajim.4700160604
Keatinge G, Laner S (1958) Some notes on the effects of excessive noise on the hearing of a group of workers. Brit J Indust Med 15(4):273. https://doi.org/10.1136/oem.15.4.273
Lie A, Skogstad M, Johannessen HA, Tynes T, Mehlum IS, Nordby KC, Engdahl B, Tambs K (2016) Occupational noise exposure and hearing: a systematic review. Int Arch Occup Environ Health 89(3):351–372. https://doi.org/10.1007/s00420-015-1083-5
Liebenberg A, Brichta AM, Nie VM, Ahmadi S, James CL (2021) Hearing threshold levels of Australian coal mine workers: a retrospective cross-sectional study of 64196 audiograms. Int J Audiol 60(10):808–819. https://doi.org/10.1080/14992027.2021.1884908
Lutman ME, Davis AC, Ferguson, MA (2008) Epidemiological evidence for the effectiveness of the noise at work regulations, RR669 (Research Report, RR669). Health and Safety Executive.
Meiman M, Klebanov M, Kabaha A, Bromberg M, Stark M (2019) 2017 Report for registry of occupational diseases in Israel. Ministry of Health 2019, Hebrew
Mirza R, Kirchner DB, Dobie RA, Crawford J (2018) Occupational noise-induced hearing Loss. J Occup Environ Med 60:e498–e501. https://doi.org/10.1097/jom.0000000000001423
NIOSH (1998) Criteria for a recommended standard: occupational exposure to noise. Revised criteria 1998. In: CDC-NIOSH Cincinnati. https://www.cdc.gov/niosh/docs/98-126/pdfs/98-126.pdf Accessed Aug 15 2022
Ohishi M (2018) Hypertension with diabetes mellitus: physiology and pathology. Hypertens Res 41(6):389–393. https://doi.org/10.1038/s41440-018-0034-4
OHS Insider (2021) Hearing Conservation–Know The Laws Around the Provinces. https://ohsinsider.com/hearing-conservation-know-the-laws-around-the-provinces/?print=print Accessed 15 August 2022
Rabinowitz PM (2012) The public health significance of noise-induced hearing loss. In: Le Prell CG, Henderson D, Fay RR, Popper AN (eds) Noise-induced hearing loss, vol 40. Springer, New York, pp 13–25
Rabinowitz PM, Galusha D, Kirsche SR, Cullen MR, Slade MD, Dixon-Ernst C (2011) Effect of daily noise exposure monitoring on annual rates of hearing loss in industrial workers. Occup Environ Med 68(6):414–418. https://doi.org/10.1136/oem.2010.055905
Rinsky-halivni L, Cohen C, Moshe S, Amster E (2020) Archives of environmental & occupational health socialized occupational medicine in Israel: past, present, and future. Arch Environ Occup Health 75(1):45–55. https://doi.org/10.1080/19338244.2019.1577211
Safe Work Australia (2018) Work Health and Safety Act 2011 (Managing Noise and Preventing Hearing Loss at Work) Code of Practice 2015. Australia, pp 1–59.
Sellappan E, Janakiraman K (2014) Environmental noise from construction site power systems and its mitigation. Noise Vib Worldw 45(3):14–20. https://doi.org/10.1260/0957-4565.45.3.14
Siegel MG (2019) The risk of noise-induced hearing loss performing knee replacement surgery. Noise Health 21(102):183–188. https://doi.org/10.4103/nah.NAH_22_19
Silva VAR, Guimarães AC, Lavinsky J, Pauna HF, Duarte AS, Castilho AM, Chone CT, Crespo AN (2022) Five-year longitudinal cohort study determines the critical intervals for periodic audiometric testing based on 5070 tests of metallurgical workers exposed and nonexposed to noise. Ear Hear 43(1):81–89. https://doi.org/10.1097/aud.0000000000001077
Sliwinska-Kowalska M (2020) New trends in the prevention of occupational noise-induced hearing loss. Int J Occup Med Environ Health 33(6):841–848. https://doi.org/10.13075/ijomeh.1896.01600
Themann CL, Masterson EA (2019) Occupational noise exposure: a review of its effects, epidemiology, and impact with recommendations for reducing its burden. J Acoust Soc Am 146(5):3879. https://doi.org/10.1121/1.5134465
Tikka C, Verbeek JH, Kateman E, Morata TC, Dreschler WA, Ferrite S (2017) Interventions to prevent occupational noise-induced hearing loss. Cochrane Database Syst Rev 7(7):Cd006396. https://doi.org/10.1002/14651858.cd006396.pub4
United States Department of Labor Bureau of Labor Statistics (2019) Nonfatal occupational illnesses by major industry sector and category of illness. https://www.bls.gov/iif/nonfatal-injuries-and-illnesses-tables/soii-summary-historical/supplemental-table-7-2019-national.xlsx Accessed Mar 15 2023
Verbeek JH, Kateman E, Morata TC, Dreschler WA, Mischke C (2014) Interventions to prevent occupational noise-induced hearing loss: a Cochrane systematic review. Int J Audiol 53(sup2):S84-96. https://doi.org/10.3109/14992027.2013.857436
Windapo AO (2013) Relationship between degree of risk, cost and level of compliance to occupational health and safety regulations in construction [Other Journal Article]. Aust J Construct Econ Build 13(2):67–82. https://doi.org/10.3316/informit.399940651100881
Acknowledgements
The authors would like to acknowledge Prof. Rafael Carel (of Blessed Memory), Prof. Yehuda Lerman from Clalit Health Services and Tel-Aviv University, and Dr. Ahser Pardo from the Israeli Institute for Occupational Safety and Hygiene (OSH) for methodological advice and assistance in evaluating noise exposure. We also gratefully thank Omer Halivni and Asher Rinsky for their help in data programming and visualization. This work was done as part of an MPH thesis at the Braun School of Public Health, Faculty of Medicine, Hadassah-Hebrew University of Jerusalem, Israel, and we would like to thank all the staff who provided technical and indirect assistance.
Author information
Authors and Affiliations
Contributions
NM, OP, MK, and LRH participated in the conception and design of the study. NM and LRH participated in the acquisition of data, performed the analyses and interpretation of data, and drafted the article. All authors contributed to the further interpretation of data, revising the manuscript critically for important intellectual content and final approval of the version to be submitted.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval and informed consent
The study was approved by the ethics committee of Clalit Health Services, Israel. A waiver of informed consent was granted by the committee due to the use of anonymous and de-identified retrospective data without access to the contact information of participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Makaruse, N., Paltiel, O., Klebanov, M. et al. The rate of occupational noise-induced hearing loss among male workers in Israel and implication on hearing surveillance frequency. Int Arch Occup Environ Health 96, 771–784 (2023). https://doi.org/10.1007/s00420-023-01975-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-023-01975-8