Abstract
Objective
Workers from various industries use personal protective equipment (PPE) including masks, respirators, and hearing protection to reduce their exposures to workplace hazards. Many studies have evaluated the physiological impacts of PPE use, but few have assessed the psychological impacts. The aim of the present study was to carry out a scoping review to compile existing evidence and determine the extent of knowledge on workplace mask, respirator or hearing protection use as a psychosocial hazard (stressor) that could result in a stress response and potentially lead to psychological injury.
Methods
The scoping review followed recognized methods and was conducted using Ovid Emcare, PubMed, Sage Journals, ScienceDirect, Scopus, SpringerLink, Google Scholar and preprint databases (OSF Preprints and medRxiv). Articles on the stressors associated with the use of masks, respirators, and hearing protection were included. The extracted data included author(s) name, year of publication, title of article, study design, population data, stressors assessed, and key findings.
Results
We retrieved 650 articles after removal of duplicates, of which 26 were deemed eligible for inclusion for review. Identified factors associated with PPE use that could potentially create a stress response were identified: communication impacts, physical impacts, psychological illness symptoms, cognitive impacts, and perceived PPE-related impacts. Evidence for respirators suggest that there may be psychological injury associated with their use. However, hearing protection appears to have a protective effect in reducing psychological symptoms such as anxiety, depression, and aggression.
Conclusions
Mask or respirator use may lead to an increase in work-related stress. Whereas hearing protection may have protective effects against psychological symptoms and improves speech intelligibility. More research is needed to better understand potential psychosocial impacts of mask, respirator and/or hearing protection use.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Personal protective equipment (PPE) is used by workers in a wide range of industries to reduce exposures to health and safety hazards (Balkhyour et al. 2019). Yet the use of PPE is recognized as the last step in the hierarchy of control to mitigate occupational hazards and is the least effective measure of controlling the risk (Olaru et al. 2021). The hierarchy progresses from elimination of the hazard, through substitution, engineering, administrative measures, and down to PPE usage. Although PPE has its limitations, its use is still considered an important protective barrier when other higher order control methods have been considered and exposure to the hazard cannot be adequately reduced by other means or in emergency response scenarios.
While the intention behind the use of PPE is to protect the worker from potential workplace hazards that could lead to physical harm, there are various physiological effects associated with PPE use that could impact upon a worker’s physical wellbeing. For instance, PPE used on the face or head, specifically hearing protection, surgical masks, and respirators, are accompanied by various mild physical and physiological impacts including pressure-related skin lesions and dermatitis (Battista et al. 2021), perceived heat stress (Scarano et al. 2020), and increased heart rate, respiratory rate, and blood pressure (Lässing et al. 2020).
PPE used on the face (masks and respirators) has been shown to impact on social interaction by creating difficulties in the recognition of faces (Freud et al. 2020) and emotions (Carbon, 2020; Grundmann et al. 2021). The use of this type of PPE can cause fatigue (Wu and McGoogan 2020), which has been shown to negatively impact performance and cognitive function (Möckel et al. 2015; Slimani et al. 2018). It can also impact on communication through reduced speech intelligibility (Randazzo, Koenig, and Priefer), which perceivably could lead to miscommunication within the workplace. Miscommunication can not only interrupt workflow and lower work efficiency but can also lead to misunderstandings and workplace conflicts. Studies have also reported on the impact of mask use, psychological impact, and communication issues in individuals with normal hearing. Malzanni et al. (2021), for instance, reported an overall decrease in quality of life for those who used face masks; specifically, impacting on individuals’ ability to perform in some physical activities and interfering with normal social activities. It was also reported that face masks were the main contributors towards communication difficulties due to sound attenuation and impairment of facial expression recognition. These effects on social interaction and cognition are psychosocial hazards that may impact on occupational stress, which could lead to psychological injury.
Psychological symptoms, such as anxiety and depression, have a bidirectional relationship with stress whereby the symptoms can be both a cause and effect of stress (Daviu et al. 2019; Kinser and Lyon 2014). Normally, the brain regulates how the body responds to stressors to maintain homeostasis of neurotransmission, endocrine levels, and immune function, alongside sympathetic and parasympathetic activity. A balance in these bodily functions contribute towards maintenance of allostasis or psychological and physical balance (Kinser and Lyon 2014; McEwen and Lasley 2003). Short term exposures to stressors can trigger regulatory functions that can enhance an individual’s response to stress and manage negative physiological effects (Epel 2009). However, problems begin to arise when one experiences long-term exposure to stressors unabated which can result in the impairment of neuronal function and regulatory systems (Kinser and Lyon 2014). Chronic exposure to stressors can eventually cause psychological injury and other comorbidities when one’s ability to cope cannot keep up with the repeated episodic stressors (McEwen and Lasley 2003).
Within the workplace, workers are exposed to a wide range of psychosocial hazards which can lead to occupational stress. Stress has both a physical (objective) and psychological (subjective) component (Mariotti 2015). Occupational stress or work-related stress occurs when the resources of an individual are not sufficient enough to cope with the demands of the situation (Basu et al. 2017). How individuals respond to stress largely results from how they anticipate and control a certain stressor (Koolhaas et al. 2011). Studies have linked adverse health and occupational outcomes with stress. Acute exposure to stress can result in gastrointestinal upset, fatigue and disturbance in sleep (Beswick et al. 2006; O’Connor et al. 2021); and those who experience chronic stress exposure are at a higher risk of developing hypertension, cardiovascular disease, psychological injury, and musculoskeletal illness (Basu et al. 2017).
Figure 1 highlights the relationship between workplace psychosocial hazards such as PPE use, stress response and psychological injury. PPE-related psychosocial hazards/stressors include communication, cognitive, physiological, and physical effects. These PPE-related stressors can then elicit a stress response, to which an individual can overcome the episode or experience psychological distress. If one does not have the resources to cope with repeated stressful episodes, they are at an increased risk of developing psychological injury or illness, physical injury or illness, and poor health behaviors.
The recent coronavirus disease 2019 (COVID-19) pandemic has resulted in an increase in the use of PPE for both the public and in various workplace settings. This has resulted in surgical mask wearing becoming a common occurrence throughout the world. Literature on the various impacts of COVID-19 continues to proliferate with many reporting the influence of mask wearing on psychological health, primarily among health care workers and the public (Amin et al. 2020; Choi et al. 2020). Outside of COVID-19 related research, most research on PPE use, to date, has tended to focus on the physiological impacts and not so much on psychological impacts.
Masks and respirators are used in other industries outside of healthcare and it is anticipated that similar psychological impacts from mask or respirator use may be experienced in these other industries. There is potential for any PPE used on the face or head that may impact on social interaction and cognition (e.g., hearing protection) to act as a psychosocial hazard or stressor. Hence, the purpose of this scoping review is to compile existing evidence on this emerging issue of workplace PPE-related psychological impacts. For the purposes of this review, PPE that will be examined will include those that occlude parts of the face (i.e., nose and mouth) and those that affect the sense of hearing. Specifically, respiratory protection (surgical face masks, and various types of respirators) and hearing protection (earmuffs and earplugs). While there are other forms of PPE that may also create a stress response in the wearer and impact on their psychosocial health (e.g., gloves, gowns, visors, and head protection), this review will focus on PPE that would most likely be used broadly in a wide range of industries.
Methods
Study design
A scoping review aims to compile an overview of existing evidence in an area of interest and provide an opportunity to identify key concepts, gaps in the research, and types and sources of evidence to inform practice, policymaking, and guide further research (Arksey and O’Malley 2005; Munn et al. 2018; Pham et al. 2014) Due to the broad nature of personal protective equipment available, the various situations in which they are used, and the lack of any published comprehensive reviews on the topic of PPE use creating a psychosocial hazard, a scoping review was deemed most appropriate for this study. The scoping review was conducted and findings were presented in accordance with the framework outlined by Arksey and O’Malley (2005). The five stages of the framework described were (1) the identification of a clear research question, (2) identification of relevant studies, (3) selection of studies, (4) charting of data, and (5) to collate, summarize, and report the results. The primary research question guiding this review is “what is the extent and scope of research on workplace use of masks, respirators or hearing protection acting as a psychosocial hazard?”.
Literature search strategies
Relevant peer-reviewed articles were searched using electronic databases and search engines including PubMed, Scopus, Ovid Emcare, SAGE Journals, ScienceDirect, and SpringerLink. These were chosen because during initial searches, the team noticed that some articles were not indexed or available in some databases or search engines. To find further relevant studies that may not have been identified through the databases, we hand searched preprint servers (OSF Preprints and medRxiv), Google Scholar and review articles. The research team limited the search to the past fifteen years [2006 to 2021]. This time period was chosen as it was believed that there would be limited research on this topic outside of healthcare and the extended time period could aid in identifying relevant research. The search strategy involved the use of the Boolean operators “AND” and “OR” when searching keywords. Furthermore, depending on the database being used, Medical Subject Headings (MeSH) were used. The keywords used were terms relating to PPE used on the face and ears (e.g., mask, hearing protection device) and psychological health (e.g., psychological distress, depression, anxiety). The keywords used were searched in the titles, abstract, and text of relevant articles. The keywords used in each search from the chosen databases and search results can be found in Supplementary Table 1. The search was conducted between 5th July and 4th of August, 2021.
Eligibility criteria
The scoping review included both qualitative and quantitative studies that had assessed the psychological health impact of PPE worn on the face and ears in the workplace, and documents that contained at least one keyword from both search groups (PPE and mental health). There were no exclusions for the PPE to any specific types (e.g., surgical face mask, respirator, earmuff, earplug). The exclusion criteria consisted of studies that investigated protective behaviors and psychological health impact as a result of an epidemic or pandemic (e.g., COVID-19, SARS), or those that have investigated the impact of an epidemic or pandemic in the workplace or in general, and editorials, commentaries, reviews, and articles that were not accessible by the primary researcher, or were published in languages other than English. While reviews were not included for assessment, they were examined to identify additional primary studies that may be eligible for inclusion.
Identification and selection of studies
The primary author searched through the databases and screened the titles for relevant articles to include for review. A second screening was conducted by two other reviewers (K.R.J. and M.M.C.) whereby the titles and abstracts were assessed against the eligibility criteria. The literature was then compared, and duplicate articles were removed. The primary author then screened the full texts of the remaining articles and summarized them into a separate document for discussion with the team. Article relevance was then discussed between the authors (R.L., K.R.J., and M.M.C.) before data was extracted and charted.
Data extraction and charting
After relevant articles were identified, data was extracted and charted in an Excel spreadsheet. The data that were extracted and recorded included the title of the article, date of publication, name of journal, study population, PPE assessed, data collection tools, risks assessed, and key findings.
Summarizing the findings
The findings were then summarized into the following research domains: psychological health impact of respiratory PPE and psychological health impact of hearing protection PPE.
Results
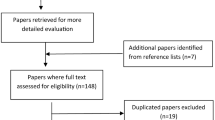
A total of 871 articles for mask/respirator-type PPE and hearing protection were retrieved from the selected six databases (Fig. 2 review schematic), plus an additional two (2) articles relevant to hearing protection, which were subsequently retrieved from Google Scholar, two (2) from preprint servers, and one (1) from a review article giving 876 papers. Two hundred and twenty-six (226) duplicate articles were then excluded. Of the remaining 650 articles, 514 articles were excluded for not meeting the inclusion criteria. The remaining 136 articles were then screened by the authors for eligibility for inclusion, of which 110 articles were removed after being deemed not relevant towards the aim of the review, i.e., were primarily focused on pandemic and mask wearing behaviors, the devices being assessed were not PPE (e.g., anesthesia mask, in-ear hearing device), and were articles investigating the general public and not workplaces. The remaining twenty-six (26) articles were deemed relevant and were included for review. From the included articles, twenty-two (22) articles were related to mask and respirator-type PPE, and four articles (4) were relevant for hearing protection. Of the 26 articles, nine (9) were cross-sectional studies, fifteen (15) experimental studies, and two (2) cohort studies (Table 1).
Although there was some variation in the industries and populations represented in the included literature, the healthcare industry was prominent, with fewer from other industries (Table 2). The studies were from a wide range of countries, with the majority from the United States of America (USA) (7 articles, 27%), followed by Iran (4 articles, 15%). Further details of article origin can be found in Table 1 and relevant findings can be found in Supplementary Table 2.
Impact of PPE
Most studies evaluated more than one psychosocial hazard or stressor associated with the use of PPE. Of the stressors assessed, over half of the articles assessed the impact of PPE on communication (16 articles, 62%) (Bandaru et al. 2020; Bani et al. 2021; Benítez et al. 2020; Bottalico et al. 2020; Brown et al. 2021; Cheok et al. 2021; Dastpaak et al. 2019; Hayirli et al. 2021; Karami et al. 2020; Kratzke et al. 2021; Nguyen et al. 2021; Radonovich Jr et al. 2009; Schlögl et al. 2021; Singh et al. 2021; Thomas et al. 2011; Yi et al. 2021). Most of these articles assessed the impact on speech intelligibility, facial and emotion recognition, and listening effort when PPE is worn. Studies also evaluated the impact on psychological health factors, such as stress, fatigue, and emotional state (5 articles, 19%) (Hoedl et al. 2020; Kratzke et al. 2021; Sakuma and Ikeda 2021; Thiagarajan et al. 2021; Wong et al. 2013). Two articles investigated the effect of PPE use on psychological illness symptoms, specifically anxiety and depression (2 articles, 8%) (Emanuel et al. 2017; Tavakolizadeh et al. 2019). A small number of articles addressed the potential cognitive impact on those who use PPE, including concentration, reaction time and decision-making (3 articles, 6%) (Benítez et al. 2020; İpek et al. 2021; Tornero-Aguilera and Clemente-Suárez, 2021). The remaining studies assessed psychosocial stressors generally, including physical symptoms and other perceived subjective impacts related to PPE which we have grouped together as ‘perceived PPE-related impacts’ (7 articles, 27%) (Benítez et al. 2020; Cheok et al. 2021; Choudhury et al. 2020; İpek et al. 2021; Rebmann et al. 2013; Singh et al. 2021; Thiagarajan et al. 2021).
Psychological impact of masks and respirators
There were fifteen articles related to communication impacts associated with respiratory PPE use (Bandaru et al. 2020; Bani et al. 2021; Benítez et al. 2020; Bottalico et al. 2020; Cheok et al. 2021; Hayirli et al. 2021; Kratzke et al. 2021; Nguyen et al. 2021; Radonovich Jr et al. 2009; Ruba and Pollak, 2020; Schlögl et al. 2021; Singh et al. 2021; Thibodeau et al. 2021; Thomas et al. 2011; Yi et al. 2021). These studies specifically investigated communication in general, emotion and facial recognition, listening effort, sentence recall, and speech intelligibility. Most articles reported that there was a negative impact on communication between individuals when facial PPE was worn (10 articles, 67% of 15 articles). Like the previously discussed hearing protection related studies, impacts on speech intelligibility become more apparent in high levels of background noise, while in low background noise, masks had little to no effect on speech intelligibility (Thomas et al. 2011). Furthermore, research that tested the effect of transparent masks reported comparable findings (Kratzke et al. 2021). Transparent masks were reported to alleviate communication impacts, especially in those with hearing impairments.
There were seven articles that reported individuals’ perceived PPE impacts (Benítez et al. 2020; Cheok et al. 2021; Choudhury et al. 2020; İpek et al. 2021; Rebmann et al. 2013; Singh et al. 2021; Thiagarajan et al. 2021). These articles reported on the physical and subjective symptoms associated with wearing PPE. Additionally, there were three articles that assessed the cognitive impact associated with facial PPE with two studies finding that participants experienced a negative effect on their decision-making and felt greater attention deficit and difficulty concentrating (Benítez et al. 2020; İpek et al. 2021). However, research by Tornero-Aguilera and Clemente-Suárez (2021) did not report an impact on cognition, specifically mental fatigue and reaction time. Though this may be due to the different cohorts being studied with the previous two articles evaluating those in healthcare compared to the latter investigating university students.
Of the twenty-two articles related to mask and/or respirator-type PPE, only one study assessed the effect of PPE use on psychological illness symptoms of those who interacted with those wearing PPE (Emanuel et al. 2017). This study reported that those who interacted with those who wore PPE experienced negative impacts on their psychological health, with increasing levels of anxiety. Additionally, four articles assessed for psychological factors and described similar findings (Kratzke et al. 2021; Sakuma and Ikeda 2021; Thiagarajan et al. 2021; Wong et al. 2013). PPE that occluded a part of the face resulted in negative psychological impacts, specifically increasing stress, fatigue, and perceiving someone who wore PPE in a more negative light. Of note, Hoedl et al. (2020) reported no significant association between stress and PPE use in nurses, but nurses who wore masks for more than eight hours had significantly higher levels of stress than those who used masks for shorter periods (p = 0.000).
Psychological impact of hearing protection
Two of the four hearing protection studies investigated impacts on communication, specifically on how hearing protection effected speech intelligibility (Dastpaak et al. 2019; Karami et al. 2020). Both articles reported that the higher the background noise the more it affected speech intelligibility regardless of whether hearing protection devices were worn or not. Furthermore, both papers reported that the use of some hearing protectors was effective in improving speech intelligibility in the presence of background noise.
Two of the articles discussed potential psychological impacts on stone workers who wore hearing protection. One study (Tavakolizadeh et al. 2019) used an intervention to investigate the effects of hearing protection use on anxiety and depression. The study found that anxiety significantly decreased after using hearing protection devices (HPD), with earplugs reducing symptoms of anxiety more than earmuffs. Earplug use was also associated with a significant decrease in depression (p < 0.01). But earmuff use was associated with a significant increase in depression (p < 0.01). The other article evaluated the effect of earmuffs and earplugs use on aggression in stone workers (Kianmehr et al. 2017). The findings of this study revealed that earplugs have a protective effect, having a significantly higher contribution to reducing aggression, specifically physical aggression, verbal aggression, anger, and hostility, than earmuffs (p < 0.05).
Six (6) articles also assessed physiological impacts. However, as this review is primarily focused on the psychological impact of PPE use, the physiological impact will not be further discussed as it is not within the scope of this review.
Discussion
To our knowledge, this is the first scoping review to focus on and collate PPE-related impacts on the psychological health of those who either wear it or are interacting with someone who has donned PPE, specifically mask and respirator-type PPE and hearing protectors. The findings of this review suggest that the use of masks, respirators or hearing protection can act as a psychosocial hazard leading to a stress response and negative psychological health consequences.
Mask and respirator use
Impact on psychological health
Findings for mask and respirator-type PPE suggest that there is a potential negative impact on psychological health and therefore the use of this PPE is a psychosocial hazard. Studies reviewed, alongside other similar studies that were excluded from assessment, reported that there were negative impacts on psychological health for both the wearer and for those who interacted with the wearer with increased levels of anxiety, depression, and psychological distress (Biermann et al. 2021; Emanuel et al. 2017; Homans and Vroegop 2021; Saunders et al. 2021; Wu et al. 2011). The study by Emanuel et al. (2017) assessing the effect of dental clinicians wearing masks and visors on special care patients, found that the style of face protection had an effect on the patients’ level of anxiety. These findings suggest that the more occluded a face becomes, the more anxious other people in close proximity become. Findings from several studies investigating the effect of masked and unmasked conditions or different types of masks, including transparent masks, have reported comparable results (Kratzke et al. 2021; Marini et al. 2021; Wong et al. 2013). These studies all demonstrated that facial occlusion of the lower face resulted in more negative psychological implications, in terms of feelings of trust and empathy towards the person wearing PPE, when compared to unmasked conditions or when transparent masks were used.
Though it should be mentioned that studies have observed cultural differences regarding protective behaviors, such as the use of PPE. A study by Wang et al. (2020) found cultural differences between Chinese and Polish citizens between physical, mental health, and mask use during COVID-19. Their study reported that Chinese were more accepting of face masks compared to Poles due to cultural differences. The same applied to respirators used to protect those who work in the industries that require them, such as mining. These cultural differences may also carry over to the workplace which may influence workers’ acceptance of PPE and subsequently their ability to cope with PPE-related stressors.
Impact on subjective and physical symptoms
Subjective and physical symptoms associated with PPE use, such as discomfort could possibly be a psychosocial stressor. A large proportion of the studies investigated reported subjective and physical impacts to individuals, including headaches, breathing difficulties, fatigue, and discomfort (Benítez et al. 2020; Cheok et al. 2021; Choudhury et al. 2020; İpek et al. 2021; Karagkouni, 2021; Rebmann et al. 2013; Ribeiro et al. 2020; Singh et al. 2021; Thiagarajan et al. 2021). Findings from a study by Thiagarajan et al. (2021) investigating PPE use and comfort levels among surgeons during the COVID-19 pandemic, found that N95 masks and eye protection contributed most to surgeon discomfort, specifically headache, dryness of mouth, breathing difficulty and fogging of eye protection, which were related to reported increased stress and fatigue. This raises concerns because symptoms such as headaches could have a negative effect on concentration and work performance (Hajjij et al. 2020).
Impact on cognition
Of the studies reviewed, three articles assessed cognitive impacts on those who wore masks or respirators (Benítez et al. 2020; İpek et al. 2021; Tornero-Aguilera and Clemente-Suárez 2021). Two articles reported that there was an impact to those in the healthcare profession (i.e., surgeons, nurses), specifically respondents reported they felt that PPE had an influence on their decision-making process (Benítez et al. 2020) and felt significantly greater attention deficit and difficulty concentrating (İpek et al. 2021). It is possible that subjective and physical responses (e.g., headache, discomfort, etc.) associated with mask or respirator use could potentially lead to an increase in occupational stress, which in turn has an impact on one’s cognition. Stress has been documented to have a negative effect on working memory, attention, response inhibition and cognitive flexibility (Girotti et al. 2018). In the workplace, this translates to an impairment in an individual’s ability to concentrate, remember, plan, and control their impulses. Consequently, this could lead to further stressful situations that, if not managed, could increase one’s risk of psychological illness or other injuries.
Hearing protection use
Impact on psychological health
While there seems to be evidence of potential negative impacts on an individual’s psychological health when using masks or respirators, the same could not be said for hearing protection. Our retrieval of hearing protection studies related to psychological health only yielded two articles (Kianmehr et al. 2017; Tavakolizadeh et al. 2019). Both articles assessed the impact on psychological symptoms such as anxiety and depression. Psychological symptoms, such as anxiety and depression, are often characterized by impaired social behaviors including excessive aggression, anger, and violence (Barrett et al. 2013; Chung et al. 2019; Meyrueix et al. 2015; Neumann et al. 2010). Findings revealed that the use of earplugs had a protective effect on these symptoms in stone workers (Kianmehr et al. 2017; Tavakolizadeh et al. 2019). Earmuffs were also found to reduce anxiety and aggression in stone workers, though were not as effective when compared to earplugs. However, depression was found to increase in those who wore earmuffs (Tavakolizadeh et al. 2019). Possible explanations for the difference include that earmuffs are large, cumbersome, unsuitable in warmer environments and in this study had higher attenuation than earplugs, which could block out more background noise (environmental noises and voices).
Communication impacts from mask, respirator or hearing protection use
An impairment in communication can lead to miscommunication between peers and supervisors that could have an influence on stress and negative emotions. Such issues, if left unresolved, could lead to conflicts or worsen a situation. Studies have found that within work environments unsolved conflicts can be detrimental to all parties involved by increasing risk of stress, fatigue and emotional exhaustion (Bültmann et al. 2002; Danielsson et al. 2015; Grandey et al. 2007). Facial occlusion may also have an impact on verbal and nonverbal communication. The majority of evidence from the studies reviewed reported negative impacts on communication, specifically emotion and facial recognition (Bani et al. 2021; Ruba and Pollak 2020), speech intelligibility (Bottalico et al. 2020; Nguyen et al. 2021; Radonovich Jr et al. 2009; Thomas et al. 2011), speech perception and listening effort (Bandaru et al. 2020), and communication in general (Benítez et al. 2020; Cheok et al. 2021; Hayirli et al. 2021; Kratzke et al. 2021; Schlögl et al. 2021; Singh et al. 2021). In situations where the use of masks or respirators are needed there may be an increased risk of stress due to partial facial occlusion and impaired communication with others. Of the few studies that investigated speech intelligibility, a study by Thomas et al. (2011) found that in low to no noise environments, masks had little to no effect on speech intelligibility. However, like hearing protection studies, background noise was found to have a significant impact on speech intelligibility regardless of the presence of PPE. Though that is not to say that PPE has no or less impact on communication, but background noise may have a synergistic effect with PPE attenuation that impairs communication, depending on the equipment used. For example, the results from a study by Toscano and Toscano (2021) revealed that in high background noise differences between masks become more apparent. Similarly, findings from Thomas et al. (2011) revealed that from within a loud environment (helicopter cockpit while the engine is operational) only some of the masks tested maintained higher accuracy of recited words.
In our scoping review we included two articles assessing impacts on communication when wearing hearing protectors, which specifically measured speech intelligibility (Dastpaak et al. 2019; Karami et al. 2020). Similar findings were reported between both articles which demonstrated that the higher the background noise the more it impacted speech intelligibility regardless of whether hearing protection was worn or not. Furthermore, the articles reported that the use of hearing protection, while in the presence of background noise, was effective in improving speech intelligibility (Dastpaak et al. 2019; Karami et al. 2020). In comparison, findings from Rocha et al. (2021) did not observe such effects with hearing protection. While they too found evidence of speech intelligibility decreasing when wearing HPDs in high levels of noise, their study did not report an improvement in speech intelligibility. Moreover, in their study, the greatest negative impact of hearing protectors had affected individuals with normal hearing, who were not normally exposed to occupational noise, suggesting that hearing protectors do not always improve speech intelligibility. In addition, evidence suggested that an increase in the attenuation of the hearing protectors led to an increase in speech interference (Karami et al. 2020). Together, these findings demonstrate the importance of matching the hearing protection to the work environment to maximize speech intelligibility. While the use of hearing protection with a high noise reduction rating (NRR) may protect the user from noise exposure, this overprotection can result in workers being exposed to other workplace stressors like impaired communication.
This review has identified possible evidence of PPE use acting as a psychosocial hazard or stressor that could have a negative impact on an individual’s psychological health. The most studied industry in relation to this topic was healthcare. Understandably, this is an important industry to evaluate as patients’ lives are in the hands of healthcare professionals and the quality of the healthcare workers’ psychological health is critical. However, in light of the current COVID-19 pandemic, the use of PPE has increased and become stricter in certain workplaces. This sudden change to everyone’s daily lifestyle and workplace behaviors has shed light on the potential stressors associated with the use of PPE that has yet to be fully explored. Hence, future research should investigate the use of PPE and its impact on occupational stress and psychological health in other industries outside of healthcare. In addition, studies that were included for review were either cross-sectional or experimental and could not evaluate long-term effects on psychological health. Future research should consider longitudinal study designs to investigate effects of long-term use of PPE.
Limitations
This scoping review employed a systematic search strategy of the scientific literature to identify studies on psychological health impacts due to PPE usage. Preliminary research into the topic revealed that this was a topic that has yet to be fully explored. Therefore, the selection criteria used were quite broad with the aim of retrieving as many relevant studies as possible. However, we acknowledge that the articles retrieved may underrepresent the research. Our review only included studies in English and may have missed findings reported in other languages. The included studies were conducted in multiple countries, in various industries and populations, and at different times before and during COVID-19, which may have influenced reported findings. A difference in cultures has been found to influence perceptions and behaviors surrounding PPE and protective behaviors (Wang et al. 2020). Finally, hearing protection related articles included for review were limited in number and the conclusions drawn may not be entirely accurate.
Conclusion
PPE is commonly used in workplaces to protect workers from physical, chemical, and biological hazards. However, the use of PPE could pose hidden risks for users, with this review identifying possible negative impacts on worker’s psychological health. The findings suggest that the use of masks and respirators may lead to an increase in occupational stress and risk of psychological symptom development. In comparison, in two studies hearing protection was found to have protective effects in reducing psychological symptoms and increasing speech intelligibility. These findings demonstrate the importance of considering the psychosocial hazards that may be created by using masks or respirators in the workplace as part of designing occupational health hazard control strategies.
References
Amin F, Sharif S, Saeed R, Durrani N, Jilani D (2020) COVID-19 pandemic-knowledge, perception, anxiety and depression among frontline doctors of Pakistan. BMC Psychiatry 20(1):1–9
Arksey H, O’Malley L (2005) Scoping studies: towards a methodological framework. Int J Soc Res Methodol 8(1):19–32. https://doi.org/10.1080/1364557032000119616
Balkhyour MA, Ahmad I and Rehan M (2019) Assessment of personal protective equipment use and occupational exposures in small industries in Jeddah: Health implications for workers. Saudi J Biol Sci 26(4):653–659. Retrieved from https://pubmed.ncbi.nlm.nih.gov/31048988. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6486506/. https://doi.org/10.1016/j.sjbs.2018.06.011
Bandaru SV, Augustine AM, Lepcha A, Sebastian S, Gowri M, Philip A, Mammen MD (2020) The effects of N95 mask and face shield on speech perception among healthcare workers in the coronavirus disease 2019 pandemic scenario. J Laryngol Otol 134(10):895–898. https://doi.org/10.1017/S0022215120002108
Bani M, Russo S, Ardenghi S, Rampoldi G, Wickline V, Nowicki S, Strepparava MG (2021) Behind the mask: emotion recognition in healthcare students. Medical Sci Educ. https://doi.org/10.1007/s40670-021-01317-8
Barrett EL, Mills KL, Teesson M (2013) Mental health correlates of anger in the general population: findings from the 2007 National Survey of Mental Health and Wellbeing. Aust N Z J Psychiatry 47(5):470–476. https://doi.org/10.1177/0004867413476752
Basu S, Qayyum H, Mason S (2017) Occupational stress in the ED: a systematic literature review. Emerg Med J 34(7):441–447
Battista RA, Ferraro M, Piccioni LO, Malzanni GE, Bussi M (2021) Personal Protective Equipment (PPE) in COVID 19 pandemic: related symptoms and adverse reactions in healthcare workers and general population. J Occup Environ Med 63(2):e80. https://doi.org/10.1097/JOM.0000000000002100
Benítez CY, Güemes A, Aranda J, Ribeiro M, Ottolino P, Di Saverio S et al (2020) Impact of personal protective equipment on surgical performance during the COVID-19 pandemic. World J Surg 44(9):2842–2847. https://doi.org/10.1007/s00268-020-05648-2
Beswick J, Gore J and Palerman D (2006) Bullying at work: a review of the literature WPS/06/04. Health Safety Laboratory, 14
Biermann M, Schulze A, Unterseher F, Atanasova K, Watermann P, Krause-Utz A et al (2021) Trustworthiness appraisals of faces wearing a surgical mask during the COVID-19 pandemic in Germany: an experimental study. PLoS One 16(5):e0251393. https://doi.org/10.1371/journal.pone.0251393
Bottalico P, Murgia S, Puglisi GE, Astolfi A, Kirk KI (2020) Effect of masks on speech intelligibility in auralized classrooms. J Acoust Soc Am 148(5):2878–2884. https://doi.org/10.1121/10.0002450
Brown VA, Van Engen KJ, Peelle JE (2021) Face mask type affects audiovisual speech intelligibility and subjective listening effort in young and older adults. Cogn Res 6(1):49. https://doi.org/10.1186/s41235-021-00314-0
Bültmann U, Kant IJ, Van Den Brandt PA, Kasl SV (2002) Psychosocial work characteristics as risk factors for the onset of fatigue and psychological distress: prospective results from the Maastricht Cohort Study. Psychol Med 32(2):333–345. https://doi.org/10.1017/S0033291701005098
Carbon C-C (2020) Wearing face masks strongly confuses counterparts in reading emotions. Front Psychol 11:2526. https://doi.org/10.3389/fpsyg.2020.566886
Cheok GJW, Gatot C, Sim CHS, Ng YH, Tay KXK, Howe TS, Koh JSB (2021) Appropriate attitude promotes mask wearing in spite of a significant experience of varying discomfort. Infect Dis Health 26(2):145–151. https://doi.org/10.1016/j.idh.2021.01.002
Choi EPH, Hui BPH, Wan EYF (2020) Depression and anxiety in Hong Kong during COVID-19. Int J Environ Res Public Health 17(10):3740
Choudhury A, Singh M, Khurana DK, Mustafi SM, Ganapathy U, Kumar A, Sharma S (2020) Physiological effects of N95 FFP and PPE in healthcare workers in COVID intensive care unit: a prospective cohort study. Indian J Crit Care Med 24(12):1169. https://doi.org/10.5005/jp-journals-10071-23671
Chung JE, Song G, Kim K, Yee J, Kim JH, Lee KE, Gwak HS (2019) Association between anxiety and aggression in adolescents: a cross-sectional study. BMC Pediatr 19(1):115. https://doi.org/10.1186/s12887-019-1479-6
Danielsson CB, Bodin L, Wulff C, Theorell T (2015) The relation between office type and workplace conflict: a gender and noise perspective. J Environ Psychol 42:161–171. https://doi.org/10.1016/j.jenvp.2015.04.004
Dastpaak H, Alimohammadi I, Jalal Sameni S, Abolghasemi J, Vosoughi S (2019) Effects of earplug hearing protectors on the intelligibility of Persian words in noisy environments. Appl Acoust 148:19–22. https://doi.org/10.1016/j.apacoust.2018.11.017
Daviu N, Bruchas MR, Moghaddam B, Sandi C and Beyeler A (2019) Neurobiological links between stress and anxiety. Neurobiol Stress 11:100191. Retrieved from https://www.sciencedirect.com/science/article/pii/S2352289519300438. https://doi.org/10.1016/j.ynstr.2019.100191
Emanuel R, Corcoran R, Cass H (2017) A study of special care dental patient preference toward choice of mask and visor use by dental clinicians. Spec Care Dentist 37(4):164–167. https://doi.org/10.1111/scd.12226
Epel ES (2009) Psychological and metabolic stress: a recipe for accelerated cellular aging? Hormones (athens) 8(1):7–22. https://doi.org/10.14310/horm.2002.1217
Freud E, Stajduhar A, Rosenbaum RS, Avidan G, Ganel T (2020) The COVID-19 pandemic masks the way people perceive faces. Sci Rep 10(1):1–8. https://doi.org/10.1038/s41598-020-78986-9
Girotti M, Adler SM, Bulin SE, Fucich EA, Paredes D, Morilak DA (2018) Prefrontal cortex executive processes affected by stress in health and disease. Prog Neuropsychopharmacol Biol Psychiatry 85:161–179. https://doi.org/10.1016/j.pnpbp.2017.07.004
Grandey AA, Kern JH, Frone MR (2007) Verbal abuse from outsiders versus insiders: comparing frequency, impact on emotional exhaustion, and the role of emotional labor. J Occup Health Psychol 12(1):63–79. https://doi.org/10.1037/1076-8998.12.1.63
Grundmann F, Epstude K, Scheibe S (2021) Face masks reduce emotion-recognition accuracy and perceived closeness. PLoS ONE 16(4):e0249792. https://doi.org/10.1371/journal.pone.0249792
Hajjij A, Aasfara J, Khalis M, Ouhabi H, Benariba F Jr, El Kettani C (2020) Personal protective equipment and headaches: cross-sectional study among moroccan healthcare workers during COVID-19 pandemic. Cureus 12(12):e12047. https://doi.org/10.7759/cureus.12047
Hayirli TC, Stark N, Bhanja A, Hardy J, Peabody CR, Kerrissey MJ (2021) Masked and distanced: a qualitative study of how personal protective equipment and distancing affect teamwork in emergency care. Int J Qual Health Care 33(2):mzab069. https://doi.org/10.1093/intqhc/mzab069
Hoedl M, Eglseer D, Bauer S (2020) Associations between personal protective equipment and nursing staff stress during the COVID-19 pandemic. medRxiv 105(4):103567
Homans NC, Vroegop JL (2021) Impact of face masks in public spaces during COVID-19 pandemic on daily life communication of cochlear implant users. Laryngoscope Investig Otolaryngol. https://doi.org/10.1002/lio2.578
İpek S, Yurttutan S, Güllü UU, Dalkıran T, Acıpayam C, Doğaner A (2021) Is N95 face mask linked to dizziness and headache? Int Arch Occup Environ Health. https://doi.org/10.1007/s00420-021-01665-3
Karagkouni O (2021) The effects of the use of protective face mask on the voice and its relation to self-perceived voice changes. J Voice. https://doi.org/10.1016/j.jvoice.2021.04.014
Karami M, Aliabadi M, Golmohammadi R, Nahrani MH (2020) The effect of hearing protection devices on speech intelligibility of Persian employees. BMC Res Notes 13(1):1–6. https://doi.org/10.1186/s13104-020-05374-x
Kianmehr M, Tavakolizadeh J, Tamaddon-Yalmeh J, Bahalgardi B (2017) Comparison of the effect of earmuffs and hocks on aggression of stone workers. Bali Med J 6(1):164–168. https://doi.org/10.15562/bmj.v6i1.388
Kinser PA, Lyon DE (2014) A conceptual framework of stress vulnerability, depression, and health outcomes in women: potential uses in research on complementary therapies for depression. Brain Behav 4(5):665–674. https://doi.org/10.1002/brb3.249
Koolhaas JM, Bartolomucci A, Buwalda B, de Boer SF, Flügge G, Korte SM et al (2011) Stress revisited: a critical evaluation of the stress concept. Neurosci Biobehav Rev 35(5):1291–1301. https://doi.org/10.1016/j.neubiorev.2011.02.003
Kratzke IM, Rosenbaum ME, Cox C, Ollila DW, Kapadia MR (2021) Effect of clear vs standard covered masks on communication with patients during surgical clinic encounters: a randomized clinical trial. JAMA Surg 156(4):372–378. https://doi.org/10.1001/jamasurg.2021.0836
Lässing J, Falz R, Pökel C, Fikenzer S, Laufs U, Schulze A et al (2020) Effects of surgical face masks on cardiopulmonary parameters during steady state exercise. Sci Rep 10(1):22363. https://doi.org/10.1038/s41598-020-78643-1
Malzanni GE, Canova C, Battista RA, Malerba P, Lerda C, Angelone SM et al (2021) Restrictive measures during COVID-19 pandemic: the impact of face masks and social distancing on communication, physical and mental health of normal hearing subjects. Hear Balance Commun 19(3):144–150. https://doi.org/10.1080/21695717.2021.1943788
Marini M, Ansani A, Paglieri F, Caruana F, Viola M (2021) The impact of facemasks on emotion recognition, trust attribution and re-identification. Sci Rep 11(1):1–14. https://doi.org/10.1038/s41598-021-84806-5
Mariotti A (2015) The effects of chronic stress on health: new insights into the molecular mechanisms of brain-body communication. Future Sci OA 1(3):FSO23–FSO23. Retrieved from https://pubmed.ncbi.nlm.nih.gov/28031896. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5137920/. https://doi.org/10.4155/fso.15.21
McEwen B, Lasley EN (2003) Allostatic load: when protection gives way to damage. Adv Mind Body Med 19(1):28–33
Meyrueix L, Durham G, Miller J, Smalley KB, Warren JC (2015) Association between depression and aggression in rural women. J Health Dispar Res Pract 8(4):136–144
Möckel T, Beste C, Wascher E (2015) The effects of time on task in response selection—an ERP study of mental fatigue. Sci Rep 5:10113. https://doi.org/10.1038/srep10113
Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E (2018) Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol 18(1):143. https://doi.org/10.1186/s12874-018-0611-x
Neumann ID, Veenema AH, Beiderbeck DI (2010) Aggression and anxiety: social context and neurobiological links. Front Behav Neurosci 4:12. https://doi.org/10.3389/fnbeh.2010.00012
Nguyen DL, Kay-Rivest E, Tewfik MA, Hier M, Lehmann A (2021) Association of in-ear device use with communication quality among individuals wearing personal protective equipment in a simulated operating room. JAMA Netw Open 4(4):e216857–e216857. https://doi.org/10.1001/jamanetworkopen.2021.6857
O’Connor DB, Thayer JF, Vedhara K (2021) Stress and health: a review of psychobiological processes. Annu Rev Psychol 72:663–688
Olaru ID, Ferrand RA, Magwenzi MT, Robertson V, Musenyereki V, Kranzer K (2021) Risk assessment for rationalizing the use of personal protective equipment for SARS-CoV2 in healthcare settings with special focus on low- and middle-income settings. Clin Microbiol Infect 27(2):169–171. https://doi.org/10.1016/j.cmi.2020.10.015
Pham MT, Rajić A, Greig JD, Sargeant JM, Papadopoulos A and McEwen SA (2014) A scoping review of scoping reviews: advancing the approach and enhancing the consistency. Res Synth Methods 5(4):371–385. Retrieved from https://pubmed.ncbi.nlm.nih.gov/26052958. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4491356/. https://doi.org/10.1002/jrsm.1123
Radonovich LJ Jr, Yanke R, Cheng J, Bender B (2009) Diminished speech intelligibility associated with certain types of respirators worn by healthcare workers. J Occup Environ Hyg 7(1):63–70. https://doi.org/10.1080/15459620903404803
Randazzo M, Koenig LL and Priefer R (2020) The effect of face masks on the intelligibility of unpredictable sentences. J Acoust Soc Am, 42: 032001. https://doi.org/10.1121/2.0001374
Rebmann T, Carrico R, Wang J (2013) Physiologic and other effects and compliance with long-term respirator use among medical intensive care unit nurses. Am J Infect Control 41(12):1218–1223. https://doi.org/10.1016/j.ajic.2013.02.017
Ribeiro VV, Dassie-Leite AP, Pereira EC, Santos ADN, Martins P, de Alencar Irineu R (2020) Effect of wearing a face mask on vocal self-perception during a pandemic. J Voice. https://doi.org/10.1016/j.jvoice.2020.09.006
Rocha CH, Lisboa G, Padilha FY, Rabelo CM, Samelli AG (2021) Effects of hearing protector devices on speech intelligibility: the importance of individualized assessment. Int J Occup Saf Ergon. https://doi.org/10.1080/10803548.2021.1880763
Ruba AL, Pollak SD (2020) Children’s emotion inferences from masked faces: Implications for social interactions during COVID-19. PLoS One 15(12):e0243708. https://doi.org/10.1371/journal.pone.0243708
Sakuma N, Ikeda K (2021) Effects of modulated emotion and facial masking encounter on personal distance. Percept Mot Skills 128(1):178–190. https://doi.org/10.1177/0031512520973515
Saunders GH, Jackson IR, Visram AS (2021) Impacts of face coverings on communication: an indirect impact of COVID-19. Int J Audiol 60(7):495–506. https://doi.org/10.1080/14992027.2020.1851401
Scarano A, Inchingolo F, Lorusso F (2020) Facial skin temperature and discomfort when wearing protective face masks: thermal infrared imaging evaluation and hands moving the mask. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph17134624
Schlögl M, Singler K, Martinez-Velilla N, Jan S, Bischoff-Ferrari HA, Roller-Wirnsberger RE et al (2021) Communication during the COVID-19 pandemic: evaluation study on self-perceived competences and views of health care professionals. Eur Geriatr Med. https://doi.org/10.1007/s41999-021-00532-1
Singh P, Bhandoria G, Maheshwari A (2021) Pharmacological prophylaxis and personal protective equipment (PPE) practices in gynecological cancer surgery during COVID-19 pandemic. Indian J Gynecol Oncol 19(1):1–7. https://doi.org/10.1007/s40944-021-00500-4
Slimani, M., Znazen, H., Bragazzi, N. L., Zguira, M. S., & Tod, D. (2018). The Effect of Mental Fatigue on Cognitive and Aerobic Performance in Adolescent Active Endurance Athletes: Insights from a Randomized Counterbalanced, Cross-Over Trial. Journal of clinical medicine, 7(12), 510. Retrieved from https://pubmed.ncbi.nlm.nih.gov/30513903. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6306934/. https://doi.org/10.3390/jcm7120510
Tavakolizadeh J, Kianmehr M, Tamaddon-Yalmeh J, Bahalgardi B, Beheshti MH (2019) Effect of hearing protection devices on anxiety and depression of stone workers. J Res Med Dental Sci 7(3):21–25
Thiagarajan S, Shetty P, Gulia A, Prakash G, Pramesh CS, Puri A (2021) A Survey of Personnel Protective equipment’s (PPE) use and comfort levels among surgeons during routine cancer surgery in the COVID-19 pandemic. Indian J Surg Oncol. https://doi.org/10.1007/s13193-021-01316-6
Thibodeau LM, Thibodeau-Nielsen RB, Tran CMQ, de Souza Jacob RT (2021) Communicating during COVID-19: the effect of transparent masks for speech recognition in noise. Ear Hear 42(4):772–781. https://doi.org/10.1097/AUD.0000000000001065
Thomas F, Allen C, Butts W, Rhoades C, Brandon C, Handrahan DL (2011) Does wearing a surgical facemask or N95-respirator impair radio communication? Air Med J 30(2):97–102. https://doi.org/10.1016/j.amj.2010.12.007
Tornero-Aguilera JF, Clemente-Suárez VJ (2021) Cognitive and psychophysiological impact of surgical mask use during university lessons. Physiol Behav 234:113342. https://doi.org/10.1016/j.physbeh.2021.113342
Toscano JC, Toscano CM (2021) Effects of face masks on speech recognition in multi-talker babble noise. PLoS One 16(2):e0246842. https://doi.org/10.1371/journal.pone.0246842
Wang C, Chudzicka-Czupała A, Grabowski D, Pan R, Adamus K, Wan X et al (2020) The association between physical and mental health and face mask use during the COVID-19 pandemic: a comparison of two countries with different views and practices. Front Psychiatry 11:901. https://doi.org/10.3389/fpsyt.2020.569981
Wong CKM, Yip BHK, Mercer S, Griffiths S, Kung K, Wong MC-S et al (2013) Effect of facemasks on empathy and relational continuity: a randomised controlled trial in primary care. BMC Fam Pract 14(1):1–7. https://doi.org/10.1186/1471-2296-14-200
Wu Z, McGoogan JM (2020) Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention. JAMA 323(13):1239–1242. https://doi.org/10.1001/jama.2020.2648
Wu S, Harber P, Yun D, Bansal S, Li Y, Santiago S (2011) Anxiety during respirator use: comparison of two respirator types. J Occup Environ Hyg 8(3):123–128. https://doi.org/10.1080/15459624.2011.549780
Yi H, Pingsterhaus A and Song W (2021) Effects of wearing face masks while using different speaking styles in noise on speech intelligibility during the COVID-19 pandemic. Front Psychol 12:682677–682677. Retrieved from https://pubmed.ncbi.nlm.nih.gov/34295288; https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8292133/. https://doi.org/10.3389/fpsyg.2021.682677
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. The first author is a recipient of the University of Queensland’s Research Training Program (RTP) scholarship. This research did not receive funding by any agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
RL, KRJ and MMC were responsible for designing the study. RL was responsible for searching the databases and initial screening for articles for inclusion. KRJ and MMC conducted the second screening stage of reviewing the titles and abstracts against the eligibility criteria. RL, KRJ and MMC were responsible for identifying potential articles for inclusion and evaluating their relevancy. RL, KRJ, MMC and MFC were involved in the drafting process of the article, critical revision for important intellectual content, and approved the submitted manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no known conflicting financial interests or non-financial interests that could have influenced the findings reported in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visithttp://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Leung, R., Cook, M.M., Capra, M.F. et al. The contribution of respiratory and hearing protection use to psychological distress in the workplace: a scoping review. Int Arch Occup Environ Health 95, 1647–1659 (2022). https://doi.org/10.1007/s00420-022-01863-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-022-01863-7