Abstract
Purpose
Self-report is an efficient and accepted means of assessing population characteristics, risk factors, and diseases. Little is known on the validity of self-reported work-related illness as an indicator of the presence of a work-related disease. This study reviews the evidence on (1) the validity of workers’ self-reported illness and (2) on the validity of workers’ self-assessed work relatedness of an illness.
Methods
A systematic literature search was conducted in four databases (Medline, Embase, PsycINFO and OSH-Update). Two reviewers independently performed the article selection and data extraction. The methodological quality of the studies was evaluated, levels of agreement and predictive values were rated against predefined criteria, and sources of heterogeneity were explored.
Results
In 32 studies, workers’ self-reports of health conditions were compared with the "reference standard" of expert opinion. We found that agreement was mainly low to moderate. Self-assessed work relatedness of a health condition was examined in only four studies, showing low-to-moderate agreement with expert assessment. The health condition, type of questionnaire, and the case definitions for both self-report and reference standards influence the results of validation studies.
Conclusions
Workers’ self-reported illness may provide valuable information on the presence of disease, although the generalizability of the findings is limited primarily to musculoskeletal and skin disorders. For case finding in a population at risk, e.g., an active workers’ health surveillance program, a sensitive symptom questionnaire with a follow-up by a medical examination may be the best choice. Evidence on the validity of self-assessed work relatedness of a health condition is scarce. Adding well-developed questions to a specific medical diagnosis exploring the relationship between symptoms and work may be a good strategy.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Self-report measures on work-related diseases including health complaints, disorders, injuries, and classical occupational diseases are widely used, especially in population surveys, such as the annual Labour Force Survey in the United Kingdom HSEa (2010). These measures are also used in more specific epidemiological studies, such as the Oslo Health Study (Mehlum et al. 2006). The purpose of these studies is to estimate or compare the prevalence rate of work-related diseases in certain groups but also case finding in workers’ health surveillance. In this review, the focus is on the self-report of work-related ill health or illness in which information is used to report about the presence of work-related diseases.
It is important to realize the difference between illness and disease. Although these terms are often used interchangeably (Kleinman et al. 1978), they are not the same. Physicians diagnose and treat diseases (i.e., abnormalities in the structure and function of bodily organs and systems), whereas patients suffer illnesses (i.e., experiences of disvalued changes in states of being and in social function: the human experience of sickness). In addition, illness and disease do not stand in a one-to-one relation. Illness may even occur in the absence of disease, and the course of a disease is distinct from the trajectory of the accompanying illness. In self-reported work-related illness, the respondent should therefore not only assess whether or not he or she is suffering from an illness (i.e., having symptoms or signs of illness or illnesses) but also assess the work relatedness of this illness. This is why self-reported work-related illness represents the collective individuals’ perception of the presence of an illness and the contribution that work made to the illness rather than a medical diagnosis and formal assessment of the work relatedness of the medical condition.
Although people’s opinions about work-related illnesses can be of interest in its own right, for epidemiological and surveillance purposes it is important to know how well self-reported work-related illnesses reflect work-related diseases as diagnosed by a physician. According to the International Labour Organization (ILO), work-related diseases are those diseases where work is one of several components contributing to the disease (ILO 2005). To estimate the incidence and prevalence of work-related diseases, the most robust way would be to undertake detailed etiological studies of exposed populations in which disease outcomes can be studied in relation to risk factors at work and other potential causative factors. However, this type of studies can rarely be performed on such a scale that the findings can serve as an estimate of the prevalence of several work-related diseases in larger populations. Thus, the common alternative approach is to rely on self-report by asking people whether they suffer from work-related illness using open, structured, or semi-structured interviews, or (self-administered) questionnaires.
Self-report measures are used to measure health conditions but also to obtain information on the demographic characteristics of respondents (e.g., age, work experience, education) and about the respondents’ occupational history of exposure, demands, and tasks. Sometimes self-report is the only way to gather this information because many health and exposure conditions cannot easily be observed directly; in those cases, it is not possible to know what a person is experiencing without asking them.
When using self-report measures, it is important to realize that they are potentially vulnerable to distortion due to a range of factors, including social desirability, dissimulation, and response style (Murphy and Davidshofer 1994; Lezak 1995).
For example, how people think about their illness is reflected in their illness perceptions (Leventhal et al. 1980). In general, these illness perceptions contain beliefs about the identity of the illness, the causes, the duration, the personal consequences of the illness, and the extent to which the illness can be controlled either personally or by treatment. As a result, people with the same symptoms or illness or injury can have widely different perceptions of their condition (Petrie and Weinman 2006). It is therefore clear that the validity of the information on self-reported disease relies heavily on the ability of participants to specifically self-report their medical condition.
From various studies, we know that the type of health condition may be a determinant for a valid self-report (Oksanen et al. 2010; Smith et al. 2008; Merkin et al. 2007). From comparing self-reported illness with information in medical records, these studies showed that diseases with clear diagnostic criteria (e.g., diabetes, hypertension, myocardial infarction) tended to have higher rates of agreement than those that were more complicated to diagnose by a physician or more difficult for the patient to understand (e.g., asthma, rheumatoid arthritis, heart failure).
The self-assessment of work relatedness can be considered a part of the perception of the causes of an illness. The attribution of an illness to work may be influenced by beliefs about disease etiology, the need to find an external explanation for symptoms, or the potential for economic compensation (Sensky 1997; Plomp 1993; Pransky et al. 1999). However, contextual factors can also influence the results of self-assessed work relatedness e.g., the way the information on study objectives is presented to the participants (Brauer and Mikkelsen 2003) or the news media attention to the subject (Fleisher and Kay 2006).
When evaluating self-reported work-related ill health, it is necessary to consider (1) the validation of the self-report of symptoms, signs, or illness, being the self-evaluation of health and (2) the self-assessment of work relatedness of the illness, being the self-evaluation of causality. To do this, we can consider self-report as a diagnostic test for the existence of a work-related disease and study the diagnostic accuracy. In addition, when synthesizing data from such “diagnostic accuracy studies”, it is important to explore the influence of sources of heterogeneity across studies, related to the health condition measured, the self-report measures used, the chosen reference standard, and the overall study quality.
Our primary objective was to assess the diagnostic accuracy of the self-report of work-related illness as an indicator for the presence of a work-related disease as assessed by an expert, usually a physician, using clinical examination with or without further testing (e.g., audiometry, spirometry, and blood tests) in working populations.
The research questions we wanted to answer were:
-
1.
What is the evidence on the validity of workers’ self-reported illness?
-
2.
What is the evidence on the validity of workers’ self-assessed work relatedness (of their illness)?
Methods
Search methods for identification of studies
An electronic search was performed on three databases as follows: Medline (through PubMed), Embase (through Ovid), and PsycINFO (through Ovid). To identify studies, a cutoff date of 01-01-1990 was imposed, and the review was limited to articles and reports published in English, German, French, Spanish, and Dutch. To answer the research questions, a search string was built after exploring the concepts of work-related ill health, self-report, measures, validity, and reliability (details Box 1). To identify additional studies, the reference lists of all relevant studies were checked.
Inclusion criteria
Types of studies
Eligible were studies in which a self-reported health condition was compared with an expert’s assessment, usually a physician’s diagnosis, based on clinical examination and/or the results of appropriate tests.
Participants
Studies had to include participants who were
-
working adults or adolescents (>16 year), or
-
workers presenting their work-related health problems in occupational health care (e.g., consulting an occupational health clinic or visiting an occupational physician or other health care worker specialized in occupational health), or
-
workers presenting their as such identified work-related health problems in general health care (e.g., visiting a general practitioner or medical specialist not specialized in occupational health).
Index tests and target conditions
Self-report methods or measures used had to assess any self-reported health condition (illness, disease, health symptoms or complaints, health rating) or assess the attribution of self-reported illness to work factors. We included self-administered questionnaires, single question questionnaires, telephone surveys using questionnaires, and interviews using questionnaires.
Reference standards
To establish work-related disease, the reference standard was an expert’s diagnosis. The included reference standards were defined as:
-
Clinical examination by a physician, physiotherapist, or registered nurse resulting in either a specific diagnosis or recorded clinical findings;
-
Physician’s diagnosis based on clinical examination combined with results from function(al) tests (e.g., in musculoskeletal disorders) or clinical tests (e.g., spirometry);
-
Results of function or clinical tests (e.g., audiometry, spirometry, blood tests, specific function tests).
Data collection and analysis
Selection of articles
In the first round, two reviewers (AL, IZ) independently reviewed all titles and abstracts of the identified publications and included all articles that seemed to meet all four inclusion criteria. In the second round, full text articles were retrieved and studies were selected if they fulfilled all four criteria. The references from each included article were checked to find additional relevant studies; if these articles were included, their references were checked as well (snowballing). To check for and improve agreement, a sample of 10 results was compared, and any disagreements were discussed and resolved in consensus meetings, if necessary, with a third reviewer (HM).
Data extraction
Data extraction was performed by one reviewer and checked by another. This extraction was performed using a checklist that included items on (a) the self-report measure; (b) the health condition that the instrument intended to measure; (c) the presence of an explicit question to assess the work relatedness of the health condition; (d) study type; (e) the reference standard (physician, test, or both) the self-report was compared with; (f) number and description of the population; (g) outcomes; (h) other considerations; (i) author and year; and (j) country. If an article described more than one study, the results for each individual study were extracted separately.
Assessment of method quality
The included articles were assessed for their quality by rating the following nine aspects against predefined criteria: aim of study, sampling, sample size, response rate, design, self-report before testing, interval between self-report and testing, blinding and outcome assessment (Table 1). The criteria were adapted from Hayden et al. (2006) and Palmer and Smedley (2007) to assess whether key study information was reported and the risk of bias was minimized. Articles were ranked higher if they were aimed at evaluation of self-report, well-powered, employed a representative sampling frame, achieved a highly effective response rate, were prospective or controlled, had a clear timeline with a short interval between self-report and examination, assessed outcome blinded to self-report, and had clear case definitions for self-report and outcome of examination/testing. Each of these qualities was rated individually and summarized to a final overall assessment per article translated into a quality score with a maximum of 23. We called a score high if it was 16 or higher: at least 14 points on aim of the study, sampling, sample size, response rate, design, interval, and outcome assessment combined and in addition positive scores for timeline and blinding of examiner. We called a score low if the summary score was 11 or lower. The moderate scores (12–15) are in between. The information regarding the characteristics of the studies, the quality and the results were synthesised into two additional tables (Tables 5, 6).
Data analysis and synthesis
Based on the self-report measures, participants were classified as positive or negative for self-report of (work-related) illness. Based on the reference standard, the participants were classified into two groups: those with a disease, clinical findings, or positive test results and those without a disease, clinical findings, or positive test results. From the 19 studies that contained sufficient data, two-by-two tables of true positives (TP), false positives (FP), false negatives (FN), and true negatives (TN) were constructed to calculate sensitivity (SE) and specificity (SP). We presented individual study results graphically by plotting the estimates of sensitivity and specificity (and their 95% confidence intervals) in a forest plot using Review Manager 5 (Fig. 3). From the studies that contained insufficient data, we presented the data on agreement (13) or sensitivity and specificity (8) in Tables 2 and 3. All data on self-assessment of work relatedness are summarized in Table 4.
The level of agreement and the predictive value of the self-report measures in relation to expert assessments were categorized as high, moderate, or low in accordance with the predefined criteria:
-
For studies reporting percentage of agreement, a percentage of >85% was considered high, 70–85% was considered moderate, <70% was considered low; (Altman 1991; Innes and Straker 1999a, b; Gouttebarge et al. 2004)
-
For studies that reported an assessment of concordance (e.g., kappa for categorical variables or Pearson correlation coefficients for continuous variables), the reported statistic was categorized according to the following criteria:
-
Kappa values >0.6 were considered high, results between 0.6 and 0.4 were considered moderate, and kappa values <0.4 were considered low (Landis and Koch 1977)
-
Pearson correlation coefficients >0.8 were considered high, results between 0.8 and 0.4 were considered moderate, and results <0.4 were considered low (Cohen and Cohen 1983; Chen and Popovich 2002; Younger 1979)
-
-
To assess sensitivity (SE), specificity (SP) independently for each measure, a value of >85% was considered high, 70–85% was considered moderate, and <70% was considered low.
Investigation of heterogeneity
Heterogeneity was investigated through analyzing the tables on level of agreement, sensitivity, and specificity and through visual examination of the forest plot of sensitivities and specificities. We also explored the effect of the overall methodological quality of the study, type of health condition, type of self-report measure, and case definition used in self-report and in the reference standard. For the construction of summary receiver operating characteristics (sROC) curves, we used a fixed effects model, mainly to explore the influence of covariates like health condition or type of self-report.
Results
Search results
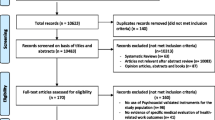
The electronic search identified 889 unique titles and abstracts, which were then screened by AL and IZ. The result was the retrieval of 50 potentially relevant articles. After assessment of the full text articles, 23 articles were included and 27 were discarded by consensus. The main reasons for exclusion being that they (1) did not address the research topic (i.e., the validity of self-reported illness among working adults), (2) did not compare self-report with expert assessment based on clinical examinations or tests, and (3) did not include an estimate of agreement between self-report and expert assessment or an estimate of the predictive value of self-report. Some articles were excluded for a combination of these reasons. (A list of excluded articles, with reasons for exclusion, is available on request.) Eight new articles were obtained by reference checking, so 31 articles in total were included in this review (Fig. 1). In the 31 articles, 32 studies were described since one article (Descatha et al. 2007) described two separate studies with different characteristics (the “Repetitive Task Survey” and the “Pays de Loire Survey”).
Methodological quality of included studies
The methodological quality was assessed for all 32 included studies, and the results are presented in Fig. 2. The range of the quality score was 10–20 (maximum 23) with a mean of 14.6 ± 2.6 and a median of 15. Of the studies, 11 had high quality (scores of 16 or higher), including 8 of 13 studies on musculoskeletal disorders; 15 had moderate quality (scores of 12–15), including 6 of 8 studies on skin disorders; and 6 had low quality (scores of 10 or 11).
Important reasons for lower study quality were a small sample size, low response rate, no control group, long interval between self-report and expert assessment, and lack of blinding to the outcomes of self-report while performing clinical examination or testing.
Characteristics of included studies
Additional Table 5 summarizes the main features of the 32 included studies, grouped according to the health condition measured: the measure/method for self-report, whether the participant was specifically asked questions on a possible relation between health impairment and work, the reference standard, the description and size of the study sample, and our quality assessment of the study.
Looking at the health conditions measured, 13 studies were aimed at musculoskeletal disorders, 8 at skin disorders, 4 at respiratory disorders, 2 at latex allergy, 2 at hearing problems, and 3 at miscellaneous problems (general health, neurological symptoms, and pesticide poisoning). In seven studies, (22%) participants were asked questions on their health as well as on their work. In four studies, participants were explicitly asked about the work relatedness of their illness or symptoms (Mehlum et al. 2009; Bolen et al. 2007; Lundström et al. 2008; Dasgupta et al. 2007). In 25 studies, the self-report was compared with the assessment by a medical expert (e.g., physician, registered nurse, or physiotherapist). In 7 studies, self-report was compared with the results of a clinical test (e.g., audiometry, pulmonary function tests, skin prick tests, blood tests).
Findings
In additional Table 6, an overview is presented of all 32 studies with the results of the comparison of self-reported work-related illness and expert assessment of work-related diseases.
Agreement between self-report and expert assessment
Thirteen studies presented results on the agreement between self-report and expert assessment (Table 2). The kappa values varied from <0.20 to 0.77, the percentages of agreement varied from 58 to 80%, and the correlation coefficients from <0.17 to 0.62. For two studies, only the significance of the correlation was reported, so the agreement level was not assessable. Overall, the agreement between self-reported illness and expert assessed disease was low to moderate.
Sensitivity and specificity of self-report
The results on sensitivity and specificity reflected the predictive value of self-reported illness to predict experts’ assessed disease. Nineteen studies (two studies by Descatha et al. 2007) contained enough data to combine in a forest plot (Fig. 3). The data were categorized according to the type of self-report: (1) questionnaires asking for symptoms, regardless of cutoff value (Symp Quest); (2) single-item questionnaires asking for self-diagnosis (Self Diag), and (3) scales rating severity of symptoms or illness (severity rate). Eight studies presented also data on sensitivity and specificity but did not contain enough data on true vs. false positives or negatives to include in the forest plot. These studies are summarized in Table 3.
Forest plot of 19 included studies, categorized by type of self-report measure. TP true positive, FP false positive, FN false negative, TN true negative. Between the brackets the 95% confidence intervals (CI) of sensitivity and specificity. The figure shows the estimated sensitivity and specificity of the study (black square) and its 95% CI (black horizontal line)
Both the sensitivity (0–100%) and the specificity (0.21–1.00) of self-report were found to be highly variable.
Assessment of work relatedness
In seven studies, work relatedness was assessed explicitly by a physician or established with a test. In four studies (Table 4), workers were explicitly asked to self-assess one-to-one the work relatedness of their self-reported illness (Mehlum et al. 2009) or symptoms (Bolen et al. 2007; Lundström et al. 2008; Dasgupta et al. 2007).
The study by Mehlum et al. (2009) was the only study that explicitly measured agreement between self-reported and expert-assessed work relatedness. Workers with neck, shoulder, or arm pain in the past month underwent an examination at the Norwegian Institute of Occupational Health. Prior to this health examination, they answered a questionnaire on work relatedness. The positive specific agreement (proportion of positive cases for which worker and physician agree) was 76–85%; the negative specific agreement (proportion of negative cases for which worker and physician agree) was 37–51%. Bolen et al. (2007) found that self-report of work-related exacerbation of asthma was poor in patients already diagnosed with asthma. Only one-third of the self-reported symptoms could be corroborated with serial peak expiratory flow findings. Lundström et al. (2008) found that just over half of all individuals vocationally exposed to hand--arm vibration at work were graded equally by self-reported symptoms and sensory loss testing. In addition, Dasgupta et al. (2007) tested whether self-reported symptoms of poisoning were useful as an indicator of acute or chronic pesticide poisoning in pesticide-exposed farmers. They found very low agreement between symptoms of pesticide poisoning and the results of blood tests measuring acetylcholinesterase enzyme activity.
In three studies, the outcomes were only compared on a group level (Nettis et al. 2003; Kujala et al. 1997; Livesley et al. 2002). In two studies on latex allergy in workers who used gloves during work the sensitivity and specificity of single symptoms/signs (e.g., contact urticaria, dyspnoea, conjunctivitis, and rhinitis) were mainly low to moderate, except for the very specific sign of localized contact urticaria (Nettis et al. 2003) and an aggregated measure combining the self-report of at least one skin symptom/sign with one mucosal symptom/sign (Kujala et al. 1997).
Investigation of heterogeneity
To explore the sources of heterogeneity across studies, the influence of the overall methodological quality of the study, the type of health condition measured, and the characteristics of the self-report measure were investigated using summary ROC (sROC) plots of those studies that contain enough data to include them in the forest plot.
In the sROC plot on overall quality of the studies, a comparison is made between 8 studies of high quality, 10 studies of moderate quality, and 2 studies of low quality. Again the results are highly variable, with a slight advantage for studies of moderate quality over studies with high or low quality (Fig. 4).
In the sROC plot on the type of health condition, a comparison is made between the results of 8 symptom questionnaires on musculoskeletal disorders (MSD), 8 on skin disorders, and 2 on hearing loss. Although the outcomes were highly variable, the combined sensitivity and specificity of symptom questionnaires on skin disorders was slightly better than for symptom questionnaires on musculoskeletal disorders and hearing loss. However, there were only a few self-report measures with a optimal balance between sensitivity and specificity.
In the sROC plot on type of self-report measure, a comparison is made between the results for 15 symptom questionnaires (i.e., questionnaires reporting symptoms of illness such as aches, pain, cough, dyspnoea, or itch), eight self-diagnostic questionnaires, (i.e., usually a single question asking whether the respondent suffered from a specified illness or symptom in a certain time frame), and two measures rating the severity of a health problem (i.e., how do you rate your hearing loss on a scale from 1 to 5). Although again the outcomes were highly variable, the combined sensitivity and specificity of symptom-based questionnaires was slightly better than for self-diagnosis or than for severity rating. In addition, symptom-based questionnaires tended to have better sensitivity, whereas self-diagnosis questionnaires tended to have better specificity.
Another source of heterogeneity may come from the variety in case definitions used in the studies for both self-report and reference standard. In the large cohorts of Descatha et al. (2007), the agreement differed substantially depending on the definition of a “positive” questionnaire result. If the definition was extensive (i.e., “at least one symptom in the past 12 months”), the agreement between the Nordic Musculoskeletal Questionnaire (NMQ) and clinical examination was low. With a more strict case definition (i.e., requiring the presence of symptoms at the time of the examination), the agreement with the outcomes of clinical examination was higher. Comparable results on the influence of case definition were reported by Perreault et al. (2008) and Vermeulen et al. (2000). Looking at the influence of heterogeneity in the reference standard, it showed that comparison of self-report with clinical examination seemed to result in mainly moderate agreement, whereas comparison of self-report with test results was low for exposure-related symptoms and tests (Lundström et al. 2008; Dasgupta et al. 2007) and moderate for hearing loss (Gomez et al. 2001) and self-rated pulmonary health change (Kauffmann et al. 1997).
Discussion
Summary of main results
Although the initial aim of the review was to come up with an overall judgment of the validity of self-reported work-related illness by workers, the number of studies that presented results on the validity of self-reported work-related illness as an integrated concept was low. That is why we chose to analyze both elements of the integrated concept separately i.e., the validity of self-reported illness as well as the validity of the self-assessed work relatedness. Workers’ self-report is compared with expert assessment based on clinical examination and clinical testing. We included 31 articles describing 32 studies in the review. The 32 studies did not comprise the full spectrum of health conditions. Musculoskeletal disorders (13), especially of the upper limbs, and hand eczema (8) were the health conditions most frequently studied, so the generalizability of the results of this review on self-reported illness is limited to these health conditions.
On the validity of self-reported illness, we considered the level of agreement between self-report and expert assessment in 13 studies. We found that agreement was mostly low to moderate. The best agreement was found between self-reported hearing loss and the results of pure tone audiometry. For musculoskeletal and skin disorders, however, the agreement was mainly moderate.
Looking at sensitivity and specificity in studies that used the self-reporting of symptoms to predict the result of expert assessment, we often found a moderate-to-high sensitivity, but a moderate-to-low specificity. In studies that used a “single question” for self-reported health problems, the opposite was often found a high specificity combined with a low sensitivity. The sensitivity and specificity for reporting of individual symptoms was variable, but mainly low to moderate, except for symptoms that were typical for a certain disease (e.g., localized urticaria in latex allergy and breathlessness in chronic obstructive lung disease).
Seven studies also considered the work relatedness of the health condition. In five studies, workers were asked about the work-relatedness of their symptoms; in the other two studies, only the expert considered work relatedness. Surprisingly, only one (Mehlum et al. 2009) studied the agreement between self-reported work relatedness and expert assessed work relatedness. They found that workers and occupational physicians agreed more on work-related cases than on non-work-related cases. Overall, the self-assessment of work relatedness by workers was rather poor when compared with expert judgement and testing.
Limitations of the review
This review has some limitations from a methodological point of view. We considered it unlikely that important high-quality studies were overlooked because we searched several databases using a broad selection of terms referring to self-report and work relatedness and checked the references of selected studies. However, our search did not, for example, encompass the “non-peer review” (gray) literature and publications in languages other than English, French, German, Spanish, and Dutch. In addition, we only included studies published after 1-1-1990 because we chose to focus on new evidence. But we trust that our "snowballing” approach would have found the most relevant studies published before that date. We did not approach authors who are currently active in the field.
As a number of the retrieved studies did not contain enough information on true and false positives and negatives, we did not include their data in the forest plot on sensitivity and specificity. After an exploration of several potentially important sources of heterogeneity, such as the overall methodological quality of the study, the health condition measured, the type of self-report measure, and the case definitions for both self-report and reference standard, we decided that a formal meta-analysis synthesizing all data was not possible as the studies were too heterogeneous.
An important methodological consideration is that the reference standard of expert assessment may not be completely independent of the worker’s self-report. The patient’s history taken by a physician or other medical expert in the consultation room along with the clinical examination and/or tests will overlap the symptoms, signs, and illness reported by the worker during self-report. This may lead to bias often referred to as common method variance, also called mono-method bias or same source bias (Spector 2006): Correlations between variables measured with the same method might be inflated. Besides from the fact that in the studies of this review information on self-report and reference standard are only partly stemming from the same source, opinions also differ about the likely effects and on what can be done to remedy potential problems. Spector and Brannick (2010) concluded that “certainty can only be approached as a variety of methods and analyses are brought to bear on a question, hopefully all converging on the same conclusion.” This was in line with the methodological remarks on diagnostic accuracy testing in the absence of a gold standard (Bossuyt et al. 2003; Rutjes et al. 2007; Reitsma et al. 2009). Since we studied self-reported work-related illness as a form of a “diagnostic test”, the evaluation would be determining its diagnostic accuracy: the ability to discriminate between suffering or not from a health condition. Usually, a test is compared with the outcomes of a gold standard that ideally provides an error-free classification of the presence or absence of the target health condition. For most health conditions, however, a gold standard without error or uncertainty is not available (Rutjes et al. 2007). In these circumstances, researchers use the best available practicable method to determine the presence or absence of the target condition, a method referred to as “reference standard” rather than gold standard (Bossuyt et al. 2003). If even an acceptable reference standard does not exist, clinical validation is an alternative approach (Reitsma et al. 2009). In a validation study, the index test results are compared with other pieces of information, none of which are necessarily a priori supposed to identify the target condition without error. These pieces of information can come from the patient’s history, clinical examination, imaging, laboratory or function tests, severity scores, and events during follow-up. This makes validation a gradual process to assess the degree of confidence that can be placed on the results of the index test results. Since the most often used reference standard for the diagnostic accuracy of self-reported illness in the included studies is “a physician’s diagnosis”, our results may contribute to the validation of self-reported work-related illness rather than prove its validity.
Our results compared with other reports
Although there are many reviews on self-report, to our knowledge there have been neither reviews evaluating self-reported illness in the occupational health field nor reviews evaluating self-assessed work relatedness. However, there have been several validation studies on self-report as a measure of prevalence of a disease in middle-aged and elderly populations, supporting the accuracy of self-report for the lifetime prevalence of chronic diseases. For example, good accuracy for diabetes and hypertension and moderate accuracy for cardiovascular diseases and rheumatoid arthritis have been reported (Haapanen et al. 1997; Beckett et al. 2000; Merkin et al. 2007; Oksanen et al. 2010). In addition, self-reported illness was compared with electronic medical records by Smith et al. (2008) in a large military cohort; a predominantly healthy, young, working population. For most of the 38 studied conditions, prevalence was found to be consistently lower in the electronic medical records than by self-report. Since the negative agreement was much higher than the positive agreement, self-report may be sufficient for ruling out a history of a particular condition rather than suitable for prevalence studies.
Oksanen et al. (2010) studied self-report as an indicator of both prevalence and incidence of disease. Their findings on incidence showed a considerable degree of misclassification. Although the specificity of self-reports was equally high for the prevalence and incidence of diseases (93–99%), the sensitivity of self-report was considerably lower for the incident (55–63%) than the prevalent diseases (78–96%). They proposed that participants may have misunderstood or forgotten the diagnosis reported by the physician, may have lacked awareness that a given condition was a definite disease, or may have been unwilling to report it. Reluctance to report was also found when screening flour-exposed workers with screening questionnaires (Gordon et al. 1997). They found with the use of self-report questionnaires a considerable underestimation of the prevalence of bakers’ asthma. One of the reasons was that 4% of the participants admitted falsifying their self-report when denying asthmatic symptoms because they wanted to avoid a medical investigation that would lead to a change of job.
Implications for practice
Self-report measures of a work-related illness are used to estimate the prevalence of a work-related disease and the differences in prevalence between populations, such as different occupational groups representing different exposures. From this review, we know that prevalence estimated with symptom questionnaires was mainly higher than prevalence estimated with the reference standards, except for hand eczema and respiratory disorders. If prevalence was estimated with self-diagnosis questionnaires, questionnaires that use a combined score of health symptoms, or for instance use pictures to identify skin diseases, they tended to agree more with the prevalence based on the reference standard.
The choice for a certain type of questionnaire depends also on the expected prevalence of the health condition in the target population. If the expected prevalence in the target population is high enough (e.g., over 20%), a self-report measure with high specificity (>0.90) and acceptable sensitivity (0.70–0.90) may be the best choice. It will reflect the “true” prevalence because it will find many true cases with a limited number of false negatives. But if the expected prevalence is low (e.g., under 2%), the same self-report measure will overestimate the “true” prevalence considerably; it will successfully identify most of the non-cases but at the expense of a large number of false positives. This holds equally true if self-report is used for case finding in a workers’ health surveillance program. Therefore, when choosing a self-report questionnaire for this purpose, one should also take into account other aspects of the target condition, including the severity of the condition and treatment possibilities. If in workers’ health surveillance it is important to find as many cases as possible, the use a sensitive symptom-based self-report questionnaire (e.g., the NMQ for musculoskeletal disorders or a symptom-based questionnaire for skin problems) is recommended, under the condition of a follow-up including a medical examination or a clinical test able to filter out the large number of false positives (stepwise diagnostic procedure).
Although the agreement between self-assessed work relatedness and expert assessed work relatedness was rather low on an individual basis, workers and physicians seemed to agree better on work relatedness compared with the non-work relatedness of a health condition. Adding well-developed questions to a specific medical diagnosis exploring the relationship between symptoms and work may be a good strategy.
Implications for research
In the validation of patients’ and workers’ self-report of symptoms, signs, or illness, it is necessary to find out more about the way sources of heterogeneity like health condition, type of self-report, and type of reference standard influence the diagnostic accuracy of self-report. To improve the quality of field testing, we recommend the use of self-report measures with proven validity, although we realize these evidence-based questionnaires might not be available for many health conditions.
To gain more insight into the processes involved in workers’ inference of illness from work, more research is needed. One way to study the possible enhancement of workers’ self-assessment is by developing and validating a specific module with a variety of validated questions on the issue of work relatedness as experienced by the worker. Such a "work-relatedness questionnaire"(generic or disease specific) may explore (1) the temporal relationship between exposure and the start or deterioration of symptoms, (2) the dose–response relationship reflected in the improvement of symptoms away from work and/or deterioration of symptoms if the worker carries out specific tasks or works in exposure areas, and (3) whether there are colleagues affected by the same symptoms related to the same exposure (Bradford Hill 1965; Lax et al. 1998; Agius 2000; Cegolon et al. 2010). The exploration of issues such as reactions on high non-occupational exposure and the issue of susceptibility may be added as well. After studying the validity and reliability of such a specific module, it could be combined into a new instrument with a reliable and valid questionnaire on self-reported (ill) health.
References
Agius R (2000) Taking an occupational history. Health environment & work 2000 (http://www.agius.com/hew/resource/occhist.htm) (updated in April 2010; accessed on 28 December 2010)
Åkesson I, Johnsson B, Rylander L, Moritz U, Skerfving S (1999) Musculoskeletal disorders among female dental personnel–clinical examination and a 5-year follow-up study of symptoms. Int Arch Occup Environ Health 72(6):395–403
Altman DG (1991) Practical statistics for medical research. Chapman & Hall, Boca Raton
Beckett M, Weinstein M, Goldman N, Yu-Hsuan L (2000) Do health interview surveys yield reliable data on chronic illness among older respondents? Am J Epidemiol 151(3):315–323
Bjorksten MG, Boquist B, Talback M, Edling C (1999) The validity of reported musculoskeletal problems. A study of questionnaire answers in relation to diagnosed disorders and perception of pain. Appl Ergon 30(4):325–330
Bolen AR, Henneberger PK, Liang X, Sama SR, Preusse PA, Rosiello RA et al (2007) The validation of work-related self-reported asthma exacerbation. Occup Environ Med 64(5):343–348
Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP, Irwig LM et al (2003) The STARD statement for reporting studies of diagnostic accuracy: explanation and elaboration. Ann Int Med 138:W1–W12
Brauer C, Mikkelsen S (2003) The context of a study influences the reporting of symptoms. Int Arch Occup Environ Health 76(8):621–624
Cegolon et al (2010) The primary care practitioner and the diagnosis of occupational diseases. BMC Public Health 10:405
Chen PY, Popovich PM (2002) Correlation: parametric and nonparametric measures. Thousand Oaks, CA: Sage Publications
Choi SW, Peek-Asa C, Zwerling C, Sprince NL, Rautiainen RH, Whitten PS et al (2005) A comparison of self-reported hearing and pure tone threshold average in the Iowa farm family health and hazard survey. J Agromed 10(3):31–39
Cohen J, Cohen P (1983) Applied multiple regression/correlation analysis for the behavioral sciences, 2nd edn. NJ Lawrence Erlbaum Associates, Hillsdale
Cvetkovski RS, Jensen H, Olsen J, Johansen JD, Agner T (2005) Relation between patients’ and physicians’ severity assessment of occupational hand eczema. Br J Dermatol 153(3):596–600
Dasgupta S, Meisner C, Wheeler D, Xuyen K, Thi LN (2007) Pesticide poisoning of farm workers-implications of blood test results from Vietnam. Int J Hyg Environ Health 210(2):121–132
de Joode BW, Vermeulen R, Heederik D, van GK, Kromhout H (2007) Evaluation of 2 self-administered questionnaires to ascertain dermatitis among metal workers and its relation with exposure to metalworking fluids. Contact Dermat 56(6):311–317
Demers RY, Fischetti LR, Neale AV (1990) Incongruence between self-reported symptoms and objective evidence of respiratory disease among construction workers. Soc Sci Med 30(7):805–810
Descatha A, Roquelaure Y, Chastang JF, Evanoff B, Melchior M, Mariot C et al (2007) Validity of Nordic-style questionnaires in the surveillance of upper-limb work-related musculoskeletal disorders. Scand J Work Environ Health 33(1):58–65
Eskelinen L, Kohvakka A, Merisalo T, Hurri H, Wagar G (1991) Relationship between the self-assessment and clinical assessment of health status and work ability. Scand J Work Environ Health 17(Suppl 1):40–47
Fleisher JM, Kay D (2006) Risk perception bias, self-reporting of illness, and the validity of reported results in an epidemiologic study of recreational water associated illnesses. Mar Pollut Bull 52(3):264–268
Gomez MI, Hwang SA, Sobotova L, Stark AD, May JJ (2001) A comparison of self-reported hearing loss and audiometry in a cohort of New York farmers. J Speech Lang Hear Res 44(6):1201–1208
Gordon SB, Curran AD, Murphy J, Sillitoe C, Lee G, Wiley K, Morice AH (1997) Screening questionnaires for bakers’ asthma—are they worth the effort? Occup Med (Lond) 47(6):361–366
Gouttebarge V, Wind H, Kuijer PP, Frings-Dresen MH (2004) Reliability and validity of functional capacity evaluation methods: a systematic review with reference to Blankenship system, Ergos work simulator, Ergo-Kit and Isernhagen work system. Int Arch Occup Environ Health 77(8):527–537
Haapanen N et al (1997) Agreement between questionnaire data and medical records of chronic diseases in middle-aged and elderly Finnish men and women. Am J Epidemiol 145(8):762–769
Hayden JA et al (2006) Evaluation of the quality of prognosis studies in systematic reviews. Ann Int Med 144(6):427–437
Hill AB (1965) The environment and disease: association or causation? Proc R Soc Med 58:295–300
HSEa (2010) Self-reported work-related illness and workplace injuries in 2008/09: results from the Labour Force Survey. HSE. 10-3-2010
ILO (2005) World day for safety and health at work: a background paper. International Labour Office, Geneva
Innes E, Straker L (1999a) Reliability of work-related assessments. Work 13:107–124
Innes E, Straker L (1999b) Validity of work-related assessments. Work 13:125–152
Johnson NE, Browning SR, Westneat SM, Prince TS, Dignan MB (2009) Respiratory symptom reporting error in occupational surveillance of older farmers. J Occup Environ Med 51(4):472–479
Juul-Kristensen B, Kadefors R, Hansen K, Bystrom P, Sandsjo L, Sjogaard G. (2006) C96linical signs and physical function in neck and upper extremities among elderly female computer users: the NEW study. Eur J Appl Physiol (96):136–45
Kaergaard A, Andersen JH, Rasmussen K, Mikkelsen S (2000) Identification of neck-shoulder disorders in a 1 year follow-up study. Validation Of a questionnaire-based method. Pain 86(3):305–310
Kauffmann F, Annesi I, Chwalow J (1997) Validity of subjective assessment of changes in respiratory health status: a 30 year epidemiological study of workers in Paris. Eur Respir J 10(11):2508–2514
Kleinman A, Eisenberg L, Good B (1978) Culture, illness, and care: clinical lessons from anthropologic and cross-cultural research. Ann Int Med 88(2):251–258
Kujala VM, Karvonen J, Laara E, Kanerva L, Estlander T, Reijula KE (1997) Postal questionnaire study of disability associated with latex allergy among health care workers in Finland. Am J Ind Med 32(3):197–204
Landis J, Koch G (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Lax MB, Grant WD, Manetti FA, Klein R (1998) Recognizing occupational disease—taking an effective occupational history. American Academy of Family Physicians 1998 (http://www.aafp.org/afp/980915ap/lax.html). Accessed on 28 Dec 2010
Leventhal H, Meyer D, Nerenz DR (1980) The common sense representation of illness danger. In: Rachman S (ed) Contributions to medical psychology. Pergamon Press, New York, pp 17–30
Lezak MD (1995) Neuropsychological assessment. Oxford University Press, Oxford
Livesley EJ, Rushton L, English JS, Williams HC (2002) Clinical examinations to validate self-completion questionnaires: dermatitis in the UK printing industry. Contact Dermat 47(1):7–13
Lundström R, Nilsson T, Hagberg M, Burstrom L (2008) Grading of sensorineural disturbances according to a modified Stockholm workshop scale using self-reports and QST. Int Arch Occup Environ Health 81(5):553–557
Meding B, Barregard L (2001) Validity of self-reports of hand eczema. Contact Dermat 45(2):99–103
Mehlum IS et al (2006) Self-reported work-related health problems from the Oslo health study. Occup Med (Lond) 56(6):371–379
Mehlum IS, Veiersted KB, Waersted M, Wergeland E, Kjuus H (2009) Self-reported versus expert-assessed work-relatedness of pain in the neck, shoulder, arm. Scand J Work Environ Health 35(3):222–232
Merkin SS, Cavanaugh K, Longenecker JC, Fink NE, Levey AS, Powe NR (2007) Agreement of self-reported comorbid conditions with medical and physician reports varied by disease among end-stage renal disease patients. J Clin Epidemiol 60:634–642
Murphy KR, Davidshofer CO (1994) Psychological testing: principles and applications, 3rd edn. Prentice-Hall International, London
Nettis E, Dambra P, Soccio AL, Ferrannini A, Tursi A (2003) Latex hypersensitivity: relationship with positive prick test and patch test responses among hairdressers. Allergy 58(1):57–61
Ohlsson K, Attewell RG, Johnsson B, Ahlm A, Skerfving S (1994) An assessment of neck and upper extremity disorders by questionnaire and clinical examination. Ergonomics 37(5):891–897
Oksanen T et al (2010) Self-report as an indicator of incident disease. Ann Epidemiol 20(7):547–554
Palmer KT, Smedley J (2007) Work-relatedness of chronic neck pain with physical findings—a systematic review. Scand J Work Environ Health 33(3):165–191
Perreault N, Brisson C, Dionne CE, Montreuil S, Punnett L (2008) Agreement between a self-administered questionnaire on musculoskeletal disorders of the neck-shoulder region and a physical examination. BMC Musculoskelet Disord 9:34
Petrie KJ, Weinman J (2006) Why illness perceptions matter. Clin Med 6(6):536–539
Plomp HN (1993) Employees’ and occupational physicians’ different perceptions of the work-relatedness of health problems: a critical point in an effective consultation process. Occup Med (Lond) 43(Suppl 1):S18–S22
Pransky G, Snyder T, Dembe A, Himmelstein J (1999) Under-reporting of work-related disorders in the workplace: a case study and review of the literature. Ergonomics 42(1):171–182
Reitsma JB, Rutjes AW, Khan KS, Coomarasamy A, Bossuyt PM (2009) A review of solutions for diagnostic accuracy studies with an imperfect or missing reference standard. J Clin Epidemiol 62:797–806
Rutjes AW, Reitsma JB, Coomarasamy A, Khan KS, Bossuyt PM (2007) Evaluation of diagnostic tests when there is no gold standard. A review of methods. Health Technol Assess 11:50
Sensky T (1997) Causal attributions in physical illness. J Psychosom Res 43(6):565–573
Silverstein BA, Stetson DS, Keyserling WM, Fine LJ (1997) Work-related musculoskeletal disorders: comparison of data sources for surveillance. Am J Ind Med 31(5):600–608
Smit HA, Coenraads PJ, Lavrijsen AP, Nater JP (1992) Evaluation of a self-administered questionnaire on hand dermatitis. Contact Dermat 26(1):11–16
Smith B et al (2008) Challenges of self-reported medical conditions and electronic medical records among members of a large military cohort. BMC Med Res Methodol 8:37
Spector PE (2006) Method variance in organizational research. Truth or urban legend? Org Res Methods 9(2):221–232
Spector PE, Brannick MT (2010) Common method issues: an introduction to the feature topic in organizational research methods. Org Res Methods 13:403
Stål M, Moritz U, Johnsson B, Pinzke S (1997) The Natural course of musculoskeletal symptoms and clinical findings in upper extremities of female milkers. Int J Occup Environ Health 3(3):190–197
Susitaival P, Husman L, Hollmen A, Horsmanheimo M (1995) Dermatoses determined in a population of farmers in a questionnaire-based clinical study including methodology validation. Scand J Work Environ Health 21(1):30–35
Svensson A, Lindberg M, Meding B, Sundberg K, Stenberg B (2002) Self-reported hand eczema: symptom-based reports do not increase the validity of diagnosis. Br J Dermatol 147(2):281–284
Toomingas A, Nemeth G, Alfredsson L (1995) Self-administered examination versus conventional medical examination of the musculoskeletal system in the neck, shoulders, and upper limbs. The Stockholm MUSIC I Study Group. J Clin Epidemiol 48(12):1473–1483
Vermeulen R, Kromhout H, Bruynzeel DP, de Boer EM (2000) Ascertainment of hand dermatitis using a symptom-based questionnaire; applicability in an industrial population. Contact Dermat 42(4):202–206
Younger MS (1979) Handbook for linear regression. Duxbury Press, North Scituate
Zetterberg C, Forsberg A, Hansson E, Johansson H, Nielsen P, Danielsson B et al (1997) Neck and upper extremity problems in car assembly workers. A comparison of subjective complaints, work satisfaction, physical examination and gender. Int J Ind Ergon 19(4):277–289
Acknowledgments
The Health and Safety Executive (HSE), United Kingdom, is thanked for funding this research. The funders approved the study design but had no role in the data collection, analysis, the decision to publish or the preparation of the manuscript.
Conflict of interest
All authors declare not having any competing interests.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Lenderink, A.F., Zoer, I., van der Molen, H.F. et al. Review on the validity of self-report to assess work-related diseases. Int Arch Occup Environ Health 85, 229–251 (2012). https://doi.org/10.1007/s00420-011-0662-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-011-0662-3