Abstract
Purpose
To assess incidence, risk factors, and treatment of retroprosthetic membrane (RPM) formation in eyes following Boston keratoprosthesis (Kpro) implantation and their correlation with glaucoma drainage device placement (GDD).
Methods
A retrospective review was performed on eyes that underwent Kpro type I or II implantation between 2005 and 2020 at a tertiary academic center. Multiple variables were collected including preoperative characteristics, presence of RPM, management of RPM, and outcomes including corrected visual acuity (VA). A Fischer’s exact test was used to evaluate the significance of risk factors of RPM formation and an odds ratio was calculated for each possible risk factor. A Mann–Whitney U test was used to evaluate comparisons between outcomes and qualitative analyses.
Results
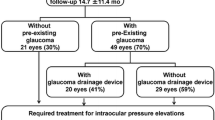
Of the 87 eyes identified, 37 (43%) developed an RPM within an average of 1.5 years (range, 31 days–7.5 years) following Kpro implantation. Mean follow-up duration was 4.3 years. Eyes that developed RPM had significantly worse preoperative VA compared to those that did not (logMAR 2.55 vs. 2.28, p = 0.022). The mean number of prior penetrating keratoplasty procedures trended higher in eyes that developed RPM (2.46 vs. 2.18, p = 0.44) but was not significant. GDD placement after Kpro implantation was associated with an increased risk of RPM formation (RR = 1.69 p = 0.026). Of the 37 eyes that developed an RPM following Kpro, 17 (47%) were treated with Nd:YAG laser, and four of those 17 (21%) also underwent pars plana vitrectomy (PPV). Seven of 37 eyes (19%) underwent PPV without Nd:YAG. Comparisons between RPM occurrence and final VA were not significant.
Conclusions
The incidence of RPM formation following Kpro implantation was 43%. Eyes that developed RPM had significantly worse preoperative VA. GDD placement after Kpro implantation increased the risk of developing RPM. Final VA and occurrence of RPM were not significantly different between the Nd:YAG and PPV treatment groups.

Similar content being viewed by others
References
Eye Bank Association of America (2019) 2019 eye banking statistical report. https://restoresight.org/wp-content/uploads/2020/04/2019-EBAA-Stat-Report-FINAL.pdf?fbclid=IwAR3AiMVzaDa7kg_mGhIdhDuQGgrJDynYZGesM1pC_9EP_Nt2qPtrQWPh-Uc Accessed 15 January 2023
Al Arfaj K (2015) Boston keratoprosthesis – clinical outcomes with wider geographic use and expanding indications – a systematic review. Saudi J Ophthalmol 29:212–221. https://doi.org/10.1016/j.sjopt.2015.02.001
Lee WB, Shtein RM, Kaufman SC, Deng SX, Rosenblatt MI (2015) Boston keratoprosthesis: outcomes and complications. Ophthalmology 122(7):1504–1511. https://doi.org/10.1016/j.ophtha.2015.03.025
Saeed HN, Shanbhag S, Chodosh J (2017) The Boston keratoprosthesis. Curr Opin Ophthalmol 28(4):390–396. https://doi.org/10.1097/icu.0000000000000373
Rudnisky CJ, Belin MW, Todani A, Al-Arfaj K, Ament JD, Zerbe BJ, Ciolino JB (2012) Risk factors for the development of retroprosthetic membranes with Boston keratoprosthesis type 1. Ophthalmology 119(5):951–955. https://doi.org/10.1016/j.ophtha.2011.11.030
Park J, Phrueksaudomchai P, Cortina MS (2020) Retroprosthetic membrane: a complication of keratoprosthesis with broad consequences. Ocul Surf. https://doi.org/10.1016/j.jtos.2020.09.004
Talati RK, Hallak JA, Karas FI, de la Cruz J, Cortina MS (2018) Retroprosthetic membrane formation in Boston keratoprosthesis. Cornea 37(2):145–150. https://doi.org/10.1097/ico.0000000000001462
Chak G, Aquavella JV (2010) A safe Nd:YAG retroprosthetic membrane removal technique for keratoprosthesis. Cornea 29(10):1169–1172. https://doi.org/10.1097/ico.0b013e3181cda001
Stacy RC (2011) Characterization of retrokeratoprosthetic membranes in the Boston type 1 keratoprosthesis. Arch Ophthalmol 129(3):310. https://doi.org/10.1001/archophthalmol.2011.26
Hou JH, Sivaraman KR, de la Cruz J, Lin AY, Cortina MS (2014) Histopathological and immunohistochemical analysis of melt-associated retroprosthetic membranes in the Boston type 1 keratoprosthesis. JAMA Ophthalmology 132(9):1133–1136. https://doi.org/10.1001/jamaophthalmol.2014.1959
The IONDT Research Group (1998) The ischemic optic neuropathy decompression trial (IONDT). Controlled Clinical Trials 19(3):276–296. https://doi.org/10.1016/s0197-2456(98)00003-8
Dohlman CH, Harissi-Dagher M, Khan BF, Sippel K, Aquavella JV, Graney J (2006) Introduction to the use of the Boston keratoprosthesis. Expert Rev Ophthalmol 1(1):41–48. https://doi.org/10.1586/17469899.1.1.41
Dohlman CH, Grosskreutz CL, Chen TC, Pasquale LR, Rubin PA, Kim EC, Durand M (2010) Shunts to divert aqueous humor to distant epithelialized cavities after keratoprosthesis surgery. J Glaucoma 19(2):111–115. https://doi.org/10.1097/IJG.0b013e3181a2fbeb
Engel LA, Muether PS, Fauser S, Hueber A (2014) The effect of previous surgery and topical eye drops for primary open-angle glaucoma on cytokine expression in aqueous humor. JAMA Ophthalmology 252(5):791–799. https://doi.org/10.1007/s00417-014-2607-5
Hu J, Goldstein DA, Leiderman YI, Malhotra V, Chau FY, Lin AY, Vajaranant TS (2013) Epithelial downgrowth after Ahmed implantation presenting as a peritubular fibrovascular membrane. J Glaucoma 22(6):e11–e13. https://doi.org/10.1097/ijg.0b013e318255d9ee
Dohlman CH, Colby KA, Belin MW, Todani A (2009) Titanium vs. PMMA backplates for boston keratoprosthesis: incidence of retroprosthetic membrane. Acta Neurochir 50(13):1505
Duan X, Xue P, Wang N, Dong Z, Lu Q, Yang F (2010) Proteomic analysis of aqueous humor from patients with primary open angle glaucoma. Mol Vis 16:2839–2846
Lenis TL, Chiu SY, Law SK, Yu F, Aldave AJ (2017) Safety of concurrent Boston type I keratoprosthesis and glaucoma drainage device implantation. Ophthalmology 124(1):12–19. https://doi.org/10.1016/j.ophtha.2016.08.003
Khair D, Daoud R, Harissi-Dagher M (2022) Retroprosthetic membrane formation in Boston keratoprosthesis type 1: incidence, predisposing factors, complications, and treatment. Cornea 41(6):751–756. https://doi.org/10.1097/ICO.0000000000002883
Lim JI, Machen L, Arteaga A, Karas FI, Hyde R, Cao D, Niec M, Vajaranant TS, Cortina MS (2018) Comparison of visual and anatomical outcomes of eyes undergoing type I Boston keratoprosthesis with combination pars plana vitrectomy with eyes without combination vitrectomy. Retina 38(Suppl 1):S125–S133. https://doi.org/10.1097/IAE.0000000000002036
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
All authors certify that they have no affiliations or any financial interest in any matters pertinent to the manuscript. Ethical approval was obtained from the Duke Institutional Review Board and was in accordance with the 1964 Helsinki declaration and its later amendments. Informed consent was exempted in this retrospective review. Authors have checked with their institutions to make sure they are complying with the specific requirements of their country for ethical considerations on this retrospective study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gabriel, B.S., Robbins, C.B., Wisely, C.E. et al. Incidence, risk factors, and treatment of retroprosthetic membranes following Boston keratoprosthesis eyes and the impact of glaucoma surgery. Graefes Arch Clin Exp Ophthalmol (2024). https://doi.org/10.1007/s00417-024-06445-6
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00417-024-06445-6