Abstract
Background
To find out the incidence and risk factors of opaque bubble layer (OBL) in eyes with myopia and myopic astigmatism following femtosecond laser–assisted in situ keratomileusis (FS-LASIK) and small incision lenticule extraction (SMILE).
Methods
A total of 1076 eyes from 569 patients who had FS-LASIK or SMILE were included in the retrospective research. For each kind of surgery, eyes were separated into two groups: "OBL" groups and "no OBL" groups. In the FS-LASIK group, eyes that developed OBL were split into "hard OBL" and "soft OBL" groups. The incidence and size of OBL were analyzed after watching the surgical procedure videotaped during the operation and taking screenshots. Surgical parameters, including sphere, cylinder, keratometry, corneal thickness, flap thickness, cap thickness, lenticule thickness, and visual acuity, were compared.
Results
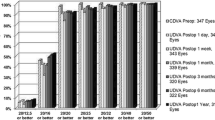
In the FS-LASIK surgery, the incidence of OBL was 63.2% (347 eyes). A thicker central corneal thickness (CCT) was the only independent risk factor affecting the OBL area (β = 0.126, P = 0.019). One hundred and thirty of these eyes had hard OBL, and the flap thickness of these eyes was thinner than that of those with soft OBL (P = 0.027). In the SMILE group, 26.6% (140 eyes) developed OBL. A higher flat keratometry (K) and a thicker residual stromal thickness (RST) were risk factors affecting the OBL area (β = 0.195, P = 0.024; β = 0.281, P = 0.001).
Conclusion
The incidence of OBL differs between the FS-LASIK surgery and the SMILE surgery. There are differences in the factors influencing OBL between the two surgeries.

Similar content being viewed by others
References
Wu J, Wu J, Wu S, Zhu D, Miao Y, Huang C, Akiti S, Vinciguerra R, Zhang X, Zhang P, Zheng X, Wang J, Wang Q, Chen S, Li Y, Ye Y, Bao F, Elsheikh A (2022) Regional Changes in Posterior Corneal Surface During a 6-Month Follow-up Period After tPRK, FS-LASIK, and SMILE. J Refract Surg 38:708–715. https://doi.org/10.3928/1081597X-20221005-02
Ang M, Farook M, Htoon HM, Mehta JS (2020) Randomized Clinical Trial Comparing Femtosecond LASIK and Small-Incision Lenticule Extraction. Ophthalmology 127:724–730. https://doi.org/10.1016/j.ophtha.2019.09.006
Lau YT, Shih KC, Tse RH, Chan TC, Jhanji V (2019) Comparison of Visual, Refractive and Ocular Surface Outcomes Between Small Incision Lenticule Extraction and Laser-Assisted In Situ Keratomileusis for Myopia and Myopic Astigmatism. Ophthalmol Ther 8:373–386. https://doi.org/10.1007/s40123-019-0202-x
Huang G, Melki S (2021) Small Incision Lenticule Extraction (SMILE): Myths and Realities. Semin Ophthalmol 36:140–148. https://doi.org/10.1080/08820538.2021.1887897
Kasetsuwan N, Satitpitakul V, Puangsricharern V, Reinprayoon U, Pariyakanok L (2016) Comparison of performances of femtosecond laser and microkeratome for thin-flap laser in situ keratomileusis. Lasers Surg Med 48:596–601. https://doi.org/10.1002/lsm.22511
Lim DH, Keum JE, Ju WK, Lee JH, Chung TY, Chung ES (2013) Prospective contralateral eye study to compare 80- and 120-μm flap LASIK using the VisuMax femtosecond laser. J Refract Surg 29:462–468. https://doi.org/10.3928/1081597X-20130617-04
Randleman JB (2020) Small Incision Lenticule Extraction (SMILE): What Now? What Next. Ophthalmology 127:1035–1036. https://doi.org/10.1016/j.ophtha.2020.03.013
Dowdle TS, Jenkins JC, Bertolio M, Monson BK (2021) Monson small-incision lenticule extraction fixation device. J Cataract Refract Surg 47:e29–e30. https://doi.org/10.1097/j.jcrs.0000000000000554
Titiyal JS, Kaur M, Shaikh F, Gagrani M, Brar AS, Rathi A (2018) Small incision lenticule extraction (SMILE) techniques: patient selection and perspectives. Clin Ophthalmol 12:1685–1699. https://doi.org/10.2147/OPTH.S157172
Asif MI, Bafna RK, Mehta JS, Reddy J, Titiyal JS, Maharana PK, Sharma N (2020) Complications of small incision lenticule extraction. Indian J Ophthalmol 68:2711–2722. https://doi.org/10.4103/ijo.IJO_3258_20
Marino GK, Santhiago MR, Wilson SE (2017) OCT Study of the Femtosecond Laser Opaque Bubble Layer. J Refract Surg 33:18–22. https://doi.org/10.3928/1081597X-20161027-01
Hurmeric V, Yoo SH, Fishler J, Chang VS, Wang J, Culbertson WW (2010) In vivo structural characteristics of the femtosecond LASIK-induced opaque bubble layers with ultrahigh-resolution SD-OCT. Ophthalmic Surg Lasers Imaging 41(Suppl):S109-113. https://doi.org/10.3928/15428877-20101031-08
Lifshitz T, Levy J, Klemperer I, Levinger S (2005) Anterior chamber gas bubbles after corneal flap creation with a femtosecond laser. J Cataract Refract Surg 31:2227–2229. https://doi.org/10.1016/j.jcrs.2004.12.069
Li L, Schallhorn JM, Ma J, Zhang L, Dou R, Wang Y (2017) Risk Factors for Opaque Bubble Layer in Small Incision Lenticule Extraction (SMILE). J Refract Surg 33:759–764. https://doi.org/10.3928/1081597X-20170821-02
Kanclerz P, Khoramnia R (2021) Flap Thickness and the Risk of Complications in Mechanical Microkeratome and Femtosecond Laser In Situ Keratomileusis: A Literature Review and Statistical Analysis. Diagnostics (Basel) 11:1588. https://doi.org/10.3390/diagnostics11091588
Lin HY, Fang YT, Chuang YJ, Yu HC, Pu C, Chou YJ, Chien CY, Lin PJ, Schallhorn SC, Sun CC (2017) Influences of Flap Shape and Hinge Angle on Opaque Bubble Layer Formation in Femtosecond Laser-Assisted LASIK Surgery. J Refract Surg 33:178–182. https://doi.org/10.3928/1081597X-20161219-02
Jung HG, Kim J, Lim TH (2015) Possible risk factors and clinical effects of an opaque bubble layer created with femtosecond laser-assisted laser in situ keratomileusis. J Cataract Refract Surg 41:1393–1399. https://doi.org/10.1016/j.jcrs.2014.10.039
Courtin R, Saad A, Guilbert E, Grise-Dulac A, Gatinel D (2015) Opaque Bubble Layer Risk Factors in Femtosecond Laser-assisted LASIK. J Refract Surg 31:608–612. https://doi.org/10.3928/1081597X-20150820-06
Kaiserman I, Maresky HS, Bahar I, Rootman DS (2008) Incidence, possible risk factors, and potential effects of an opaque bubble layer created by a femtosecond laser. J Cataract Refract Surg 34:417–423. https://doi.org/10.1016/j.jcrs.2007.10.026
Lim DH, Hyun J, Shin E, Ko BW, Chung ES, Chung TY (2019) Incidence and Risk Factors of Opaque Bubble Layer Formation According to Flap Thickness During 500-kHz FS-LASIK. J Refract Surg 35:583–589. https://doi.org/10.3928/1081597X-20190814-01
Mastropasqua L, Calienno R, Lanzini M, Salgari N, De Vecchi S, Mastropasqua R, Nubile M (2017) Opaque bubble layer incidence in Femtosecond laser-assisted LASIK: comparison among different flap design parameters. Int Ophthalmol 37:635–641. https://doi.org/10.1007/s10792-016-0323-3
Wang Y, Ma J, Zhang J, Dou R, Zhang H, Li L, Zhao W, Wei P (2017) Incidence and management of intraoperative complications during small-incision lenticule extraction in 3004 cases. J Cataract Refract Surg 43:796–802. https://doi.org/10.1016/j.jcrs.2017.03.039
Ma J, Wang Y, Li L, Zhang J (2018) Corneal thickness, residual stromal thickness, and its effect on opaque bubble layer in small-incision lenticule extraction. Int Ophthalmol 38:2013–2020. https://doi.org/10.1007/s10792-017-0692-2
Son G, Lee J, Jang C, Choi KY, Cho BJ, Lim TH (2017) Possible Risk Factors and Clinical Effects of Opaque Bubble Layer in Small Incision Lenticule Extraction (SMILE). J Refract Surg 33:24–29. https://doi.org/10.3928/1081597X-20161006-06
Wang Z, Cheng X, Lou X, Chen H, Lu Z, Chen H, Yu Y (2022) VisuMax Flap 2.0: a flap plus technique to reduce incidence of an opaque bubble layer in femtosecond laser-assisted LASIK. Graefes Arch Clin Exp Ophthalmol 261:1187–1194. https://doi.org/10.1007/s00417-022-05894-1
Liu CH, Sun CC, Hui-Kang Ma D, Chien-Chieh Huang J, Liu CF, Chen HF, Hsiao CH (2014) Opaque bubble layer: incidence, risk factors, and clinical relevance. J Cataract Refract Surg 40:435–440. https://doi.org/10.1016/j.jcrs.2013.08.055
Kanellopoulos AJ, Asimellis G (2013) Essential opaque bubble layer elimination with novel LASIK flap settings in the FS200 Femtosecond Laser. Clin Ophthalmol 7:765–770. https://doi.org/10.2147/OPTH.S43723
Liu T, Yu T, Liu L, Chen K, Bai J (2018) Corneal Cap Thickness and Its Effect on Visual Acuity and Corneal Biomechanics in Eyes Undergoing Small Incision Lenticule Extraction. J Ophthalmol 2018:6040873. https://doi.org/10.1155/2018/6040873
Morishige N, Petroll WM, Nishida T, Kenney MC, Jester JV (2006) Noninvasive corneal stromal collagen imaging using two-photon-generated second-harmonic signals. J Cataract Refract Surg 32:1784–1791. https://doi.org/10.1016/j.jcrs.2006.08.027
Morishige N, Wahlert AJ, Kenney MC, Brown DJ, Kawamoto K, Chikama T, Nishida T, Jester JV (2007) Second-harmonic imaging microscopy of normal human and keratoconus cornea. Invest Ophthalmol Vis Sci 48:1087–1094. https://doi.org/10.1167/iovs.06-1177
Jun I, Kang D, Roberts CJ, Lee H, Jean SK, Kim EK, Seo KY, Kim TI (2021) Comparison of Clinical and Biomechanical Outcomes of Small Incision Lenticule Extraction With 120- and 140-µm Cap Thickness. Transl Vis Sci Technol 10:15. https://doi.org/10.1167/tvst.10.8.15
Wei CH, Dai QY, Mei LX, Ge Y, Zhang PF, Song E (2019) Paired eye-control study of unilateral opaque bubble layer in femtosecond laser assisted laser in situ keratomileusis. Int J Ophthalmol 12:654–659. https://doi.org/10.18240/ijo.2019.04.21
Wu N, Christenbury JG, Dishler JG, Bozkurt TK, Duel D, Zhang L, Hamilton DR (2017) A Technique to Reduce Incidence of Opaque Bubble Layer Formation During LASIK Flap Creation Using the VisuMax Femtosecond Laser. J Refract Surg 33:584–590. https://doi.org/10.3928/1081597X-20170621-06
Acknowledgements
We would like to thank Nantong Science and Technology Project MSZ2022024 and the Science and Technology Development Plan of Jiangsu Provincial Administration of Traditional Chinese Medicine MS2022091 for financial support. The authors thank Ms. Guojuan Jin and Ms. Jing Zhang for skillful technique assistance.
Funding
This project has been funded in part by grants from Nantong Science and Technology Project MSZ2022024 and the Science and Technology Development Plan of Jiangsu Provincial Administration of Traditional Chinese Medicine MS2022091.
Author information
Authors and Affiliations
Contributions
Conceptualization: Hui Chen, Ying Yu; Methodology: Mingrui Li, Haixia Ji; Formal analysis and investigation: Xinliang Cheng, Jun Li; Writing—original draft preparation: Zichen Wang; Writing—review and editing: Ying Yu; Supervision: Aimin Sang.
Corresponding author
Ethics declarations
Ethics approval
This retrospective comparative study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Human Investigation Committee (IRB) of Affiliated Hospital of Nantong University approved this study.
Conflicts of interest
All authors have no conflicts of interest in this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, Z., Li, M., Ji, H. et al. Comparison of risk factors for OBL in FS-LASIK and SMILE correction for myopia and myopia astigmatism. Graefes Arch Clin Exp Ophthalmol 262, 1925–1931 (2024). https://doi.org/10.1007/s00417-023-06336-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-023-06336-2