Abstract
Introduction
Astigmatism correction after small-incision lenticule extraction (SMILE) surgery is affected by several factors, including ocular residual astigmatism (ORA), which accounts for the vector difference between refractive and corneal astigmatism. Previous studies revealed the relationship between ORA and astigmatism correction after laser-assisted in situ keratomileusis (LASIK). However, in SMILE surgery, no comprehensive study exploring the link between these two variables has been performed. We have therefore assessed the association between ORA and astigmatism correction after SMILE.
Methods
This was a retrospective, single-centered study. Patients with myopia or myopic astigmatism who underwent SMILE surgery using the 500-kHz Visumax laser platform and were followed up for at least 3 months were included. Patients’ demographic and clinical characteristics, such as visual acuity, refractive status and corneal tomography, were recorded. ORA was calculated using Alpins Statistical System for Ophthalmic Refractive Surgery Techniques (ASSORT) Ocular Residual Astigmatism calculator.
Results
A total of 888 eyes (408 eyes from males and 480 eyes from females) from 444 patients (mean age [standard deviation] 32.4 ± 7.1 years) were included in our study. Mean (± SD) preoperative sphere and cylinder were − 5.45 ± 1.98 (range − 10.00–0.00) diopter (D) and − 0.89 ± 0.70 (range − 4.00–0.00) D, respectively. Calculated mean ORA was 0.68 ± 0.35 (range 0.07–3.53) D. Postoperative logMAR uncorrected visual acuity was 0.03 ± 0.31. Mean postoperative sphere and cylinder were − 0.10 ± 0.56 (range − 1.5 to 1.0) D and − 0.51 ± 0.37 (− 1.5 to 0.0) D, respectively. The Pearson correlation test revealed preoperative sphere, steep keratometry (steep-K) and ORA were statistically correlated with the amplitude of astigmatism correction (P < 0.001), and the generalized estimating equations analysis showed that ORA was negatively correlated with the amplitude of astigmatism correction (P < 0.001).
Conclusion
The results of our study suggest that preoperative higher ORA may be associated with a lower magnitude of astigmatism correction after SMILE surgery in patients with all levels of astigmatism preoperative.
Trial Registration
ClinicalTrials.gov: NCT05604872. Registered 3 November 2022—Retrospectively registered. https://clinicaltrials.gov/ct2/show/NCT05604872.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Previous studies have shown that ocular residual astigmatism (ORA) could affect astigmatism outcome after small-incision lenticule extraction (SMILE) surgery, but the participants in these studies were limited to patients with low to moderate refractive astigmatism or to sampling a single eye from one patient. |
The aim of our study was to provide a more comprehensive analysis of the relationship between ORA and the amplitude of astigmatism correction in patients who undergo SMILE. |
Our null hypothesis is that ocular residual astigmatism is not associated with refractive astigmatism correction. |
What was learned from the study? |
The results of the study showed that a higher preoperative ORA was associated with a lower magnitude of astigmatism correction after SMILE in patients with low to severe astigmatism. |
Our study showed that the astigmatism outcomes after SMILE refractive surgery not only relied on manifest refractive astigmatism itself, but that physicians should also consider the difference between manifest refractive astigmatism and corneal astigmatism. |
Introduction
Uncorrected refractive error was one of the leading causes of moderate to severe vision impairment around the world in 2015 [1]. The prevalence of myopia in the global population is 28.3%, and it is even higher in East and Southeast Asia [2]. The prevalence of astigmatism worldwide ranges from 8% to 62% and is higher among elderly individuals [3].
Small incision lenticule extraction (SMILE) is an effective refractive surgery for correcting myopia or myopic astigmatism [4, 5]. In 2020, the US Food and Drug Administration (FDA) approved a treatment for astigmatism with cylinder range of within − 3.00 diopters (D) [6]; the Taiwan FDA approved cylinder treatment up to − 5.00 D. However, several studies have shown that SMILE results in a higher risk of postoperative residual astigmatism than laser in situ keratomileusis (LASIK) [7,8,9], such that retreatment may be needed [10]. A recent review reported on factors that could impact the efficacy of SMILE for correcting astigmatism, including cyclotorsion, center or optic zone, angle kappa, patient positioning, incision location, types of astigmatism (with-the-rule or against-the-rule) and ocular residual astigmatism [11].
Ocular residual astigmatism (ORA) is defined as the vector difference between refractive and corneal astigmatism, and it has been reported that patients with high ORA are negatively affected by postoperative residual astigmatism or induced astigmatism if they undergo LASIK [12]. In normal astigmatic eyes, the ORA can range from 0.01 to 1.87 D [13]. The importance of ORA in astigmatism correction has been reported in previous studies, in which a higher ORA or higher ORA ratio was observed to be associated with a lower risk of postoperative astigmatism correction after SMILE [14, 15]. Recent studies reported that patients without preoperative astigmatism who underwent refractive correction with SMILE experienced postoperative astigmatism [16] and that using the vector analysis method to correct astigmatism in patients with high ORA could yield acceptable refractive outcomes [17]. However, the patient populations of these studies were limited to patients with low to moderate refractive astigmatism or to sampling a single eye from one patient. The aim of our study was to provide a more comprehensive analysis of the relationship between ORA and the amplitude of astigmatism correction in patients who undergo SMILE.
Methods
This study was retrospectively conducted from 2020 to 2021 at the Taipei Nobel Eye Clinic and was approved by the Ethics Committee of National Changhua University of Education (Changhua, Taiwan). It was registered on ClinicalTrials.gov (identifier NCT05604872, date of approval: November 3, 2022). All procedures performed were conducted in accordance with the tenets of the Declaration of Helsinki and its later amendments. Informed consent was not needed in the study.
The inclusion criteria for this study were: age between 20 and 50 years; corrected distance visual acuity (CDVA) of both eyes reaching 0.1 logarithm of the minimum angle of resolution (logMAR); and stable refractive errors of myopia (− 0.50 to − 10.00 D) and astigmatism (0.00 to − 5.00 D). The exclusion criteria were: cataract; corneal opacities or irregularities; dry eye (Schirmer’s test I ≤ 5 mm); amblyopia; coexisting ocular pathologies; glaucoma; nondilating pupil; history of intraocular surgery, laser therapy or retinopathy; optic nerve or macular diseases; estimated postoperative cornea residual stromal thickness < 250 μm; pregnancy or current lactation; uncontrolled diabetic mellitus or systemic immune disease; and refusal or inability to maintain follow-up.
Ophthalmic Examinations
The patients were examined preoperatively as well as at 1 day, 1 week, 1 month and 3 months after surgery as scheduled. At each visit, a thorough ophthalmologic examination was performed that included tests for uncorrected visual acuity (UCVA) and CDVA, in addition to manifest refraction, biomicroscopy and pneumotonometry. Fundus examination, cycloplegic refraction and corneal tomography were performed before surgery. Cycloplegic refraction was applied after instilling 1 drop of 1% Mydrin P (tropicamide 0.5%, phenylephrine HCl 0.5%) 3 times at 5-min intervals. Autorefraction data were collected before and after cycloplegia with Topcon KR-8900 (Topcon, Tokyo, Japan). Corneal astigmatism values were exported from the Pentacam (Pentacam HR; Oculus GmbH, Wetzlar, Germany) machine as measured by the Scheimpflug keratometry system. The magnitude of astigmatism correction was defined as the postoperative cycloplegic subjective astigmatism minus the preoperative cycloplegic manifest astigmatism.
Surgery
The triple centration technique marking under slit-lamp at 3, 6 and 9 o’clock was used for all patients on the same day before surgery to prevent cyclotorsion. To achieve proper alignment, the operator could rotate the applanation cone clockwise or counterclockwise after suction fixation was applied and before femtosecond laser scanning started. A 500-kHz Visumax (Carl Zeiss Meditec AG, Jena, Germany) femtosecond laser was used with cap thicknesses ranging from 100 to 130 μm and cap diameters ranging from 7.3 to 7.9 mm. The lenticule was dissected with a blunt spatula through a 30- to 60-degree incision at the 10 o’clock position and removed using forceps afterward. Treatment targets of both eyes were set to emmetropia, and the refraction corrections were based on manifest refractions. Levofloxacin and prednisolone acetate eyedrops were prescribed 4 times daily after surgery for 1 week.
Statistical Analysis
The preoperative demographics and postoperative outcome variables were collected according to our chart review. The sample size needed for the study was assessed by the software PS Power and Sample Size Calculations Version 3.0 [18]. Prior data indicate that the standard deviation (SD) of ORA is 0.4 and that for the regression errors is 0.7. The slope of the line obtained by regressing the change in astigmatism against ORA is − 0.25. Taking all factors into account, it was determined that 842 eyes should be included in the study in order to be able to reject the null hypothesis that this slope equals zero with a probability (power) of 0.8 under a type I error rate < 0.001 [18]. To analyze the primary outcome measure, statistical significance was set at P < 0.001. Correlations between variables were tested using Pearson’s correlation analysis. A generalized estimating equation (GEE) approach was used to adjust the clustering effect between the left and right eyes from the same patient [19]. Stata Version 13.0 was used for data analysis (StataCorp, College Station, TX, USA). Vector analysis included the targeted induced astigmatism vector [20], surgically induced astigmatism vector (SIA), difference vector (DV) (remaining refractive astigmatism after surgery) and correction index (CI) (the ideal CI = 1, whereas CI > 1 indicates overcorrection, and CI < 1 indicates undercorrection) were calculated using AstigMATIC software Version 2.0 [21]. The ORA was calculated by Alpins Statistical System for Ophthalmic Refractive Surgery Techniques (ASSORT) Ocular Residual Astigmatism calculator (https://assort.com/assort-vector-calculator) after calculating the vector difference between the manifest refractive astigmatism and corneal astigmatism values [20].
Results
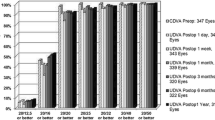
A total of 888 eyes (408 eyes from males and 480 eyes from females) from 444 patients (mean age ± standard deviation [SD] 32.4 ± 7.1 years) were included in our study. Table 1 presents the patients’ demographic and clinical characteristics, including preoperative visual acuity, refractive status, corneal keratometry data, postoperative visual acuity, UDVA, CDVA and spherical equivalent. The mean (± SD) preoperative spectacle plane sphere and cylinder were − 5.45 ± 1.98 D and − 0.89 ± 0.70 D, respectively. The mean ORA was 0.68 ± 0.35 D. All surgical procedures were conducted smoothly. The postoperative mean sphere was − 0.10 ± 0.56 D, and the mean cylinder was − 0.51 ± 0.37 D. Figure 1 presents the vector analysis results for target induced astigmatism (TIA, the astigmatic change that the operator intended to induce), SIA, DV and CI; the mean DV was 0.47 D with a CI of 1.01, indicating acceptable surgical outcomes.
Single-angle polar plots for the target-induced astigmatism vector [20], surgically induced astigmatism vector, difference vector and the correction index at 3 months after small-incision lenticule extraction (SMILE) surgery. Ax Axis, cyl cylinder, D diopter, SD standard deviation
The analysis of the relationship between the amplitude of astigmatic correction and patient demographics is summarized in Table 2. Steep keratometry (steep-K) was found to be positively correlated with the amplitude of astigmatic correction, whereas ORA and sphere were negatively correlated with the amount of correction. These results revealed that higher preoperative ORA and sphere may be related to a weaker efficacy of astigmatic correction.
Table 3 shows the GEE analysis of independent variables of the amplitude of astigmatism correction. Age and sex were not related to astigmatism correction, and the results of this analysis reconfirmed that with increasing ORA, the amount of astigmatism correction could be negatively decreased. Figure 2 shows that after adjusting for age, the ORA was negatively related to the amplitude of astigmatism correction and that the trend was consistent within the low, moderate and high astigmatism groups for both male and female patients.
Discussion
This study is the first large-scale, comprehensive study covering various degrees of preoperative astigmatism, and the results showed that ORA was associated with a lower magnitude of astigmatism correction after SMILE. Other factors that may affect astigmatism correction have been described in previous studies. Regarding types of astigmatism, undercorrection may be noted in with-the-rule astigmatism and overcorrection in against-the-rule astigmatism [11], although overcorrection with-the-rule astigmatism was noted in a previous study [22]. Cap thickness, cap diameter, incision width and incision position were not found to be associated with astigmatism outcomes [23, 24]. Large-angle kappa and decentration from the pupil center and kappa intercept are associated with increased higher-order aberration and compromised visual outcomes; nevertheless, their association with astigmatism correction has not been elucidated [25, 26]. Cyclotorsion during docking and femtosecond laser scanning procedures would partially offset the effect of astigmatism correction, which can be checked by the marking position using the triple centration technique marking and manually repositioned by a rotating applanation interface cone after suction fixation is applied; however, the accuracy of this approach is still not comparable to that of the image-guided system [27].
The concordance of refractive astigmatism and corneal astigmatism has been deciphered, and a linear regression line can be plotted in a coordinate system using keratometric astigmatism as the abscissa and refractive astigmatism as the ordinate [28]. Nonetheless, the measurement of refractive astigmatism might be influenced by patients’ perceptual preference for objects or by behaviors of the optometrist [29]. Intra- or interobserver variability can also yield different refractive astigmatism measurement outcomes. In a previous study measuring 40 eyes for cylinder power and axis, the repeatability of cycloplegic subjective power measurement accounted for only 92.5% of the variability within 0.25 D; furthermore, the repeatability of cycloplegic subjective axis measurement accounted for up to 62.5% of variability, with a shift of the axis of > than 5° [30]. For astigmatism correction in refractive surgery, Alpins advocated considering both refractive and corneal astigmatism, and the term “ocular residual astigmatism” was coined to describe the vector difference between these two kinds of astigmatism [31].
Higher ORA could offset astigmatism correction after SMILE, as noted by the authors of previous studies, although it was noted that it was confined to eyes with low to moderate astigmatism. In Qian’s series, 122 right eyes of 122 patients were included, with the correction range of sphere being − 3.5 to − 10.75 D and that of the cylinder being 0.25–3.00 D; the cutoff point of ORA was set at 1.00 D, whereas the mean postoperative manifest astigmatism was higher in patients within the high ORA group [14]. Chan et al. compared patients (134 eyes of 134 patients) with a higher ORA ratio (defined value of ORA as the nominator and preoperative refractive astigmatism as the denominator), which tended to result in a lower index of success in vector analysis compared with the lower ORA ratio group [15]. In a clinical trial including 114 eyes of 114 patients with mild to moderate astigmatism (< 2.50 D), in which the high ORA group was designated as ORA > 0.75 D, the high ORA eyes were randomized into the manifest planning group (astigmatism corrected 100% by refractive astigmatism) and vector planning group (astigmatism corrected 60% by refractive astigmatism and 40% by corneal astigmatism), respectively [17]. The vector planning group yielded better postoperative refractive outcomes [17]. Our study further broadened the scope from previous studies in that we included a larger sample size, examined both eyes of each patient and observed a continuous, consistent trend of ORA outcomes from low to high preoperative refractive astigmatism rather than a binary trend.
Our study has a number of limitations. First, the study had a retrospective design; therefore, we could only determine the association between variables. Additionally, the large sample size and statistical methods applied to decrease the effect of selection bias led to some patients being lost to follow-up, probably due to unsatisfactory results. Second, there was no adjustment for other confounding factors that may affect the refractive outcomes, such as cyclotorsion or decentration from the pupil center and kappa intercept. Third, this was a single-center, single-surgeon study, and the results of our study may not be generalizable to other patient populations and centers.
Conclusions
Our study showed that a higher preoperative ORA was associated with a lower magnitude of astigmatism correction after SMILE in patients with astigmatism ranging from low to severe. Further prospective, multicenter studies may need to be conducted to reconfirm this trend.
References
Flaxman SR, Bourne RRA, Resnikoff S, et al. Global causes of blindness and distance vision impairment 1990-2020: a systematic review and meta-analysis. Lancet Glob Health. 2017;5(12):e1221–e34.
Baird PN, Saw SM, Lanca C, et al. Myopia. Nat Rev Dis Primers. 2020;6(1):99.
Zhang J, Wu Y, Sharma B, Gupta R, Jawla S, Bullimore MA. Epidemiology and burden of astigmatism: a systematic literature review. Optom Vis Sci. 2023;100(3):218–31.
Hjortdal J, Vestergaard AH, Ivarsen A, Ragunathan S, Asp S. Predictors for the outcome of small-incision lenticule extraction for Myopia. J Refract Surg. 2012;28(12):865–71.
Chansue E, Tanehsakdi M, Swasdibutra S, McAlinden C. Efficacy, predictability and safety of small incision lenticule extraction (SMILE). Eye Vis (Lond). 2015;2:14.
Dishler JG, Slade S, Seifert S, Schallhorn SC. Small-incision lenticule extraction (SMILE) for the correction of myopia with astigmatism: outcomes of the United States food and drug administration premarket approval clinical trial. Ophthalmology. 2020;127(8):1020–34.
Chen X, Wang Y, Zhang J, Yang SN, Li X, Zhang L. Comparison of ocular higher-order aberrations after SMILE and Wavefront-guided Femtosecond LASIK for myopia. BMC Ophthalmol. 2017;17(1):42.
Khalifa MA, Ghoneim A, Shafik Shaheen M, Aly MG, Pinero DP. Comparative analysis of the clinical outcomes of SMILE and wavefront-guided LASIK in low and moderate Myopia. J Refract Surg. 2017;33(5):298–304.
Chiang B, Valerio GS, Manche EE. Prospective, randomized contralateral eye comparison of wavefront-guided laser in situ keratomileusis and small incision lenticule extraction refractive surgeries. Am J Ophthalmol. 2022;237:211–20.
Moshirfar M, Shah TJ, Masud M, Linn SH, Ronquillo Y, Hoopes PC, Sr. Surgical options for retreatment after small-incision lenticule extraction: advantages and disadvantages. J Cataract Refract Surg. 2018;44(11):1384–9.
Chow SSW, Chow LLW, Lee CZ, Chan TCY. Astigmatism Correction Using SMILE. Asia Pac J Ophthalmol (Phila). 2019;8(5):391–6.
Qian YS, Huang J, Liu R, et al. Influence of internal optical astigmatism on the correction of myopic astigmatism by LASIK. J Refract Surg. 2011;27(12):863–8.
Lin J. The contribution of ocular residual astigmatism to anterior corneal astigmatism in refractive astigmatism eyes. Sci Rep. 2021;11(1):1018.
Qian Y, Huang J, Chu R, et al. Influence of intraocular astigmatism on the correction of myopic astigmatism by femtosecond laser small-incision lenticule extraction. J Cataract Refract Surg. 2015;41(5):1057–64.
Chan TCY, Wan KH, Zhang L, Wang Y. Impact of ocular residual astigmatism on predictability of myopic astigmatism correction after small-incision lenticule extraction. J Cataract Refract Surg. 2019;45(4):525–6.
Gyldenkerne A, Hjortdal J, Ivarsen A. Astigmatism prediction in small-incision lenticule extraction. J Cataract Refract Surg. 2020;46(4):524–33.
Jun I, Kang DSY, Arba-Mosquera S, et al. Comparison of clinical outcomes between vector planning and manifest refraction planning in SMILE for myopic astigmatism. J Cataract Refract Surg. 2020;46(8):1149–58.
Dupont WD, Plummer WD, Jr. Power and sample size calculations for studies involving linear regression. Control Clin Trials. 1998;19(6):589–601.
Zeger SL, Liang KY, Albert PS. Models for longitudinal data: a generalized estimating equation approach. Biometrics. 1988;44(4):1049–60.
Alpins N. Astigmatism analysis by the Alpins method. J Cataract Refract Surg. 2001;27(1):31–49.
Gauvin M, Wallerstein A. AstigMATIC: an automatic tool for standard astigmatism vector analysis. BMC Ophthalmol. 2018;18(1):255.
Yang X, Liu Q, Lin H, Xie Y, Feng Q. Long-term vector outcomes of SMILE in correcting moderate to high with-the-rule astigmatism under astigmatism axis marked condition. J Refract Surg. 2020;36(9):585–91.
Chan TC, Ng AL, Cheng GP, Wang Z, Woo VC, Jhanji V. Effect of location of opening incision on astigmatic correction after small-incision lenticule extraction. Sci Rep. 2016;6:35881.
Ivarsen A, Gyldenkerne A, Hjortdal J. Correction of astigmatism with small-incision lenticule extraction: Impact of against-the-rule and with-the-rule astigmatism. J Cataract Refract Surg. 2018;44(9):1066–72.
Shao T, Wang Y, Ng ALK, et al. The The effect of intraoperative angle kappa adjustment on higher-order aberrations before and after small incision lenticule extraction. Cornea. 2020;39(5):609–14.
Wong JX, Wong EP, Htoon HM, Mehta JS. Intraoperative centration during small incision lenticule extraction (SMILE). Medicine (Baltimore). 2017;96(16):e6076.
Kose B. Detection of and compensation for static cyclotorsion with an image-guided system in SMILE. J Refract Surg. 2020;36(3):142–9.
Grosvenor T, Quintero S, Perrigin DM. Predicting refractive astigmatism: a suggested simplification of Javal’s rule. Am J Optom Physiol Opt. 1988;65(4):292–7.
Goggin M. Internal astigmatism and ocular residual astigmatism. J Cataract Refract Surg. 2012;38(2):381–2.
Walline JJ, Kinney KA, Zadnik K, Mutti DO. Repeatability and validity of astigmatism measurements. J Refract Surg. 1999;15(1):23–31.
Alpins NA. New method of targeting vectors to treat astigmatism. J Cataract Refract Surg. 1997;23(1):65–75.
Acknowledgements
Funding
This research received no external funding. The journal’s Rapid Service fee was provided by Chao-Kai Chang.
Medical Writing and Editorial Assistance
Medical writing and editorial assistance were provided by Springer Nature Author Services, funded by the authors.
Author Contributions
Conceptualization: Chao-Kai Chang and Chen-Cheng Chao. Methodology: Chen-Cheng Chao. Software: Meng-Yin Lin and Chen-Cheng Chao. Formal analysis: Meng-Yin Lin. Investigation: Meng-Yin Lin. Data curation: Chao-Kai Chang and Chen-Cheng Chao. Writing—original draft preparation: Chao-Kai Chang and Chen-Cheng Chao. Writing—review and editing: Chao-Kai Chang. Visualization: Meng-Yin Lin and Chao-Kai Chang. All authors have read and agreed to the published version of the manuscript.
Compliance with Ethics Guidelines
This study was retrospectively conducted from 2020 to 2021 at the Taipei Nobel Eye Clinic and was approved by the Ethics Committee of National Changhua University of Education (Changhua, Taiwan). It was registered on ClinicalTrials.gov (identifier NCT05604872, date of approval: November 3, 2022). All procedures performed were conducted in accordance with the tenets of the Declaration of Helsinki and its later amendments. Informed consent was not needed in the study.
Disclosures
All named authors confirm that they have no conflicts of interest to declare.
Data Availability
The data are available upon reasonable request to the corresponding author.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Chao, CC., Lin, MY. & Chang, CK. The Association Between Ocular Residual Astigmatism and the Efficacy of Astigmatism Correction Via Small Incision Lenticule Extraction (SMILE). Ophthalmol Ther 12, 2631–2640 (2023). https://doi.org/10.1007/s40123-023-00766-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-023-00766-1