Abstract
Purpose
Anti-retinal autoantibodies are assumed to be associated with age-related macular degeneration (AMD). To our knowledge, this is the first evaluation of autoantibodies in human sera of participants with different stages of AMD in a large population-based, observational cohort study in Germany.
Methods
The Gutenberg Health Study (GHS) is a population-based, observational cohort study in Germany, including 15,010 participants aged between 35 and 74. Amongst others, non-mydriatic fundus photography (Visucam PRO NM™, Carl Zeiss Meditec AG, Jena, Germany) was performed. Fundus images of the first 5000 participants were graded based on the Rotterdam Eye Study classification. Sera of participants with AMD (n=541) and sera of age-matched participants without AMD (n=490) were analyzed by antigen-microarrays. Besides descriptive statistics, autoantibody-levels were compared by Mann-Whitney-U test and the associations of level of autoantibodies with AMD were calculated by logistic regression analysis. Likewise, possible associations of the autoantibodies and both clinical and laboratory parameters on AMD subjects were analyzed.
Results
Autoantibodies against transferrin (p<0.001) were significantly downregulated in participants with early AMD and soft, distinct drusen (≥63 μm) or pigmentary abnormalities only compared to Controls. Mitogen-activated protein kinase 3 (p=0.041), glutathione peroxidase 4 (p=0.048), clusterin (p=0.045), lysozyme (p=0.19), protein kinase C substrate 80K-H (p=0.02), heat shock 70 kDa protein 1A (p=0.04) and insulin (p=0.018) show a trend between Control and participants with early AMD and soft, distinct drusen (≥63 μm) or pigmentary abnormalities only.
Conclusions
This study contributes to a growing knowledge of autoantibodies in association with different AMD stages compared to controls in the context of a large population-based study in Germany. Especially autoantibodies against inflammatory proteins were downregulated in participants with early AMD and soft, distinct drusen (≥63 μm) or pigmentary abnormalities only.

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Age-related macular degeneration (AMD) is one of the major causes of irreversible visual impairment in industrialized countries [1].
In a previous study the prevalence of AMD in the Gutenberg Health Study (GHS) cohort was determined on the basis of fundus photographs from 4,340 participants [2]. Aging is the greatest risk factor for AMD, accordingly, in a previous study the prevalence of AMD in the cohort increased with age; however, although AMD is usually defined to occur after age 50, signs of early AMD were found in 3.8 % of individuals in the youngest age group (younger than 45 years) [2]. Additionally, several studies during the last years reported the involvement of anti-retinal autoantibodies in ocular disorders, such as retinal vasculitis [3], retinopathy [4, 5], retinitis pigmentosa [6] and also AMD [7,8,9,10,11,12]. These studies support the growing evidence of an immunological involvement in the pathogenesis of AMD. Accordingly, in a previous study we could demonstrate a difference in Immunoglobulin G (IgG) antibody patterns against retinal antigens between patients with wet AMD and healthy volunteers [13]. Until now the relevance and the role of autoantibodies in the pathogenesis of AMD is unknown and it is unclear if antibodies play a causative role during the pathogenesis of AMD or might appear as secondary effects during the disease’s progression. Autoantibody evaluation in serum may provide a minimally invasive procedure with impact for prediction of disease activity, prognosis and especially response to treatment in the future.
The aim of this study is to provide different serological autoantibody biomarkers in relation to different stages of AMD in comparison to healthy control subjects.
We therefore evaluated the presence of different serologic autoantibody levels in study participants with AMD in the population-based Gutenberg Health Study (GHS).
Materials and methods
Study population
The Gutenberg Health Study (GHS) is a population-based, prospective, single-center cohort study at the medical center of the Johannes Gutenberg University Mainz in Germany [14]. The sample was randomly drawn via local residents’ registration offices and equally stratified by sex for each decade of age. Exclusion criteria for participation in the GHS were physical or mental inability or insufficient knowledge of German to participate in the examinations in the study center. The baseline examination with a total of 15,010 participants aged 35 to 74 years was conducted from 2007 to 2012. We included a subsample of 541 subjects with AMD and 490 control subjects in this analysis.
The GHS mainly focuses on the general health status of the population to develop better cardiovascular risk stratification. Thus, the ophthalmologic examination is embedded in an interdisciplinary setting including general examinations emphasising cardiovascular parameters, completed by psychological questionnaires, and laboratory tests with biobanking for proteomic and genetic analyses. The setting of our study enables the detection of associations between ophthalmic and systemic findings and their development over time [2].
The ophthalmic part has been described in detail elsewhere [15]. In brief, we conducted measurements of objective refraction and distance-corrected visual acuity, intraocular pressure, visual field testing, pachy- and keratometry, and posterior segment photography.
AMD grading
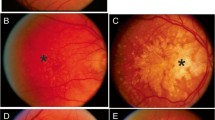
The fundus images were taken with a non-mydriatic fundus camera (Visucam PRO NMTM, Carl Zeiss AG, Jena, Germany) in a darkened room and with the pupil’s natural width. Three photographs were taken of each eye: at 30° and 45° centered on the optic nerve, and at 30° centered on the macula.
We evaluated data from the first 5,000 subjects enrolled in the GHS between April 2007 and October 2008. The grading was performed based on the Rotterdam Eye Study classification and was described in detail previously [2, 16]. As control, a group of age- and sex-matched participants without AMD was used. The control group was defined as having no signs of AMD at all, without drusen or pigmentary abnormalities in either eye. AMD1 was defined as early AMD (stage 1a: soft, distinct drusen (≥63 μm) only; stage 1b: pigmentary abnormalities only, no soft drusen (≥63 μm), AMD2 was defined as early AMD (stage 2a: soft, indistinct drusen (≥125 μm) or reticular drusen only; stage 2b: soft, distinct drusen (≥63 μm) with pigmentary abnormalities), AMD3 was defined as early AMD (stage 3: soft, indistinct (≥125 μm) or reticular drusen with pigmentary abnormalities) and AMD4 was defined as late AMD in one eye corresponding to geographic atrophy or neovascular AMD [16].
AMD4 participants were defined as atrophic or neovascular AMD. Participants with maculopathy unrelated to AMD were excluded. When different stages of AMD were noted between the right and the left eye, we chose the classification for the worse eye. Cases of strict unilateral, nonspecific maculopathy were grade as being unrelated to AMD.
Sera
Full blood samples of the GHS participants with different AMD stages and matched participants without AMD were allowed to clog for 30 minutes and were centrifuged for 10 minutes at 4°C and 1000g. The supernatant was collected and serum samples were stored at -80°C until further use.
Microarray manufacturing and incubation
Customized microarrays were manufactured in our lab using a non-contact piezo-dispenser (SciFEXARRAYER S3, Scienion, Berlin, Germany). The 61 selected antigens (S1 Table) were spotted in triplicates onto nitrocellulose coated microarray slides (AVID Oncyte, 16 Pad NC slides, Grace Biolabs, Bend, Oregon, USA). The 61 antigens were selected based on literature and previous studies regarding AMD and (eye-) diseases with autoimmune components. The spotting process was carried out in a humidity chamber with humidity set to 60%. To allow optimal immobilization of the proteins on the microarray surface, slides were kept on the spotter platform to dry overnight prior to incubation. For the incubation steps, the slides were clamped into incubation chambers (ProPlate Multiwell chambers, Grace Biolabs, Bend, USA), separating the slide into 16 distinct subarrays. The following incubation steps were performed at 4°C on an orbital shaker. To decrease background signals, the arrays were incubated with blocking buffer (Super G, Grace Biolabs, Bend, Oregon, USA) for one hour. Afterwards, the blocking buffer was removed and residual buffer was removed by washing three times with phosphate-buffered saline containing 0.5% Tween-20 (PBST). The arrays then were incubated with 100μL serum samples in a 1:250 dilution in PBS overnight. Positive and negative controls were included on each slide. Slides were washed again three times with PBST followed by incubation for one hour with a secondary anti-human antibody conjugated with Alexa fluor 647 (Alexa Fluor® 647 AffiniPure Goat Anti-Human IgG, Fcγ fragment specific, 109-605-008, Jackson Immunoresearch) in a 1:500 dilution in PBS. After the incubation with the secondary antibody, the slides were washed two times with PBST and two times with ultrapure water. Slides were dried for two minutes in a vacuum concentrator (SpeedVac, Thermo Scientific, Waltham, Massachusetts, USA).
Image acquisition and data preprocessing
The microarray slides were scanned with a high resolution confocal laser scanner (428 Array Scanner, Affymetrix, Santa Clara, California, USA). The scans were saved as 16 bit Tagged Image File Format (TIFF)images. Spot intensities were quantified with an image processing software (Imagene 5.5, BioDiscovery Inc., Los Angeles, California, USA). Spots with poor quality were manually flagged and removed from further analysis. Local background intensity was subtracted from median pixel intensities and the means from the three technical replicates were calculated. The resulting data for each array was normalized using a constant scale factor.
Statistical analysis
Descriptive statistics included for dichotomous parameters absolute and relative frequencies, for continuous measurements mean and standard deviations for approximately normal distributed data, and otherwise median and interquartile ranges. To find possible differences between subjects with AMD and controls in the underlying antibody data Mann-Whitney’s U test was used. Shapiro Wilk’s test was computed to test normal distribution of autoantibody levels.
In a second step, the three different groups (Control, AMD1 and AMD2) were compared using Kruskal-Wallis-Test followed by between-groups comparisons with Bonferroni correction.
Logistic regression analysis was performed with AMD Group (yes/no) as dependent variable and Antibody-level (per 1000 units) as independent variable adjusted for smoking, body-mass-index, glycated hemoglobin (HbA1c) level, level of high-density lipoproteins, of low-density lipoproteins and triglycerides.
Protein interaction networks, biological pathways and protein clusters were generated with Ingenuity Pathway Analysis (IPA v.01–04).
The statistical analysis was performed in Statistica (Statistica 13, Statsoft, Tulsa, Oklahoma, USA) and in R version 3.3.1 (R Core Team (2016). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/.).
Results
In this nested case-control study, 1116 subjects (601 AMD patients and 515 control subjects) were included. 85 subjects had less than 75% valid values for the antibodies and were therefore excluded. Finally, 541 subjects with AMD (AMD1: n=454, AMD2: n=64, AMD3: n=15, AMD4: n=8) and 490 control subjects were included. Characteristics of the study population are demonstrated in Tables 1 and 2.
Shapiro Wilk’s test showed that neither the laboratory parameters nor the antibody levels were normally distributed. Therefore, Mann-Whitney’s U test was applied for the following analysis.
Antibody levels were compared between subjects with and without AMD. 8 out of 61 antibodies showed different levels between both groups (p<0.05): a decrease of autoantibody levels against mitogen-activated protein kinase 3 (p=0.016), glutathione peroxidase 4 (p=0.026), clusterin (p=0.028), lysozyme (p=0.029), transferrin (p<0.001) and protein kinase C substrate 80K-H (p=0.013) was observed in the AMD group (Table 3). On the other side, heat shock 70 kDa protein 1A (p=0.028) and insulin (p=0.017) were upregulated. The other autoantibodies showed no up- or downregulation.
Logistic regression analysis showed, that the association between AMD and autoantibody level was still present after including the following parameters as independent variables into the model to adjust for: (yes vs. no), body-mass-index, HbA1c level, level of high-density lipoproteins, of low-density lipoproteins and triglycerides (all continuous) in case of mitogen-activated protein kinase 3 (p=0.04), lysozyme (p=0.013), transferrin (p<0.007) and protein kinase C substrate 80K-H (p=0.019) and insulin (p=0.02) (Table 4).
For further detailed investigation of the different AMD stages, Control, AMD1 and AMD2 were compared. Using Kruskal-Wallis-Test followed by between-groups comparisons only transferrin (p<0.001) could be confirmed between Control and AMD1 after applying the false discovery rate (FDR for n=183; 3 groups, 61 antibodies) of 5% using the Benjamini-Hochberg procedure. Mitogen-activated protein kinase 3 (p=0.041), glutathione peroxidase 4 (p=0.048), clusterin (p=0.045), lysozyme (p=0.19), protein kinase C substrate 80K-H (p=0.02), heat shock 70 kDa protein 1A (p=0.04) and insulin (p=0.018) show a trend between Control and AMD1, but are rejected as significant after applying the FDR. No significant regulations could be observed between AMD2 versus AMD1 or Control (Fig 1).
Box-and-whisker plot for detected autoantibodies. Box-and-whisker plot for detected autoantibodies. The X-axis represents the three groups (Control, AMD 1 and AMD 2) and the Y-axis the measured intensity values. Using Kruskal-Wallis-Test followed by between-groups comparisons only transferrin (p<0.001) could be confirmed between Control and AMD1 after applying the false discovery rate (FDR) of 5% using the Benjamini-Hochberg procedure
Protein interaction networks showed most of the proteins targeted by the regulated antibodies are involved in Connective Tissue Disorders, Organismal Injury and Abnormalities, Skeletal and Muscular Disorders and Neurological Diseases (Table 5). Furthermore, canonical pathways were discovered including multiple targeted proteins (Table 6).
Discussion
In our study, we report an evaluation of autoantibodies in human sera by antigen-microarrays of participants with different stages of AMD and healthy controls in a large population-based, prospective, observational cohort study in Germany (The Gutenberg Health Study (GHS)). Autoantibodies against mitogen-activated protein kinase 3, glutathione peroxidase 4, clusterin, lysozyme, transferrin and protein kinase C substrate 80K-H were downregulated in AMD 1 compared to Control. Autoantibodies against transferrin were significantly downregulated in participants with early AMD and soft, distinct drusen (≥63 μm) or pigmentary abnormalities only compared to Controls. Autoantibodies against heat shock 70kDa protein 1A and insulin were upregulated in AMD 1.
Transferrin might serve as a component of oxidative defense system of the retina [17]. Chowers and coworkers demonstrated that transferrin expression is increased in the retinas of patients with AMD relative to those of healthy control patients supposed a role in the oxidative defense system [17]. Transferrin is an iron transport protein and is expressed at high levels in the retina [17]. Wysokinski et al. showed that the serum level of transferrin was higher in the AMD group (p< 0.001) than in the control, but the total serum iron levels did not differ between both groups [18]. Also, genetic polymorphisms in iron homeostasis genes constituted potential risk markers for AMD [18]. In our study, autoantibodies against transferrin were significantly downregulated in the AMD 1 group compared to individuals without AMD.
Yang and coworkers demonstrated, that inhibition of protein kinase C increased retinal pigment epithelium (RPE) cell susceptibility to complement attack [19]. Complement activation is clearly involved in the pathogenesis of AMD [20, 21]. Zhang et al. also suggested, that light induced phagocytic crisis of RPE cells may result from the down-regulation of protein kinase C alpha (PKC-α)/ezrin signaling, with PKC-α/ezrin as a key signal pathway regulating the phagocytosis of many types of cells [22, 23]. Accordingly, autoantibodies against protein kinase C substrate 80K-H were downregulated in AMD 1 in our study.
The etiology of AMD is complex and multifactorial, but there is evidence that oxidative stress is involved in AMD pathogenesis and progression [24, 25]. In recent years, studies indicated that MAPK (mitogen-activated protein kinases) pathways are involved in the development of AMD [25, 26]. Oxidative stress and reactive oxygen species (ROS) have been implicated in the activation of various signaling pathways, including the MAPKs [25, 27]. Several studies suggested that MAPKs play a major role in oxidative stress-induced RPE degeneration [25, 28]. Koinzer and coworkers showed a biphasic activation of MAPK3 ERK1/2 after oxidative insult in RPE cells, of which the late activation was pro-apoptotic [28]. Recently, there has been described an important role of ERK1/2 activation in the pathogenesis of geographic atrophy, a late manifestation of AMD [29]. Autoantibodies against MAPK3 were downregulated in AMD 1 compared to Control in our analysis. Hypothetically, the downregulation in the AMD 1 group might indicate a loss of the protective function and an enhancement of the pro-apoptotic activation with resulting RPE degeneration.
Anti-carbonic anhydrase II (anti-CA II) autoantibodies were detected in sera of patients with autoimmune retinopathies (AR), including cancer-associated retinopathy (CAR) and also in normal population [30]. Anti-Carbonic anhydrase II is involved in retinal disorders [31, 32], additionally, antiretinal antibodies against CAII have been detected in the sera of patients with autoimmune diseases, such as type 1 diabetes [33], Sjögren´s syndrome [34] or systemic lupus erythematodes [35]. Because of the wide occurrence of anti-CAII antibodies in diseases, it is likely that all of these diseases may have a common pathogenic mechanism based on autoimmune responses [30]. Transferably, suspected immunologic origins of AMD include e.g. the alternative complement pathway, immune cell activation, and autoimmunity [36].
Basic proteins such as lysozyme were shown to promote melanin polymerization under acidic conditions [37]. In the present study, autoantibodies against lysozyme were downregulated in AMD 1 compared to Control. Sarangajan et al. stated that the ability of the melanin polymer to act as an anti- or as an pro-oxidant may be dependent upon its state of aggregation [37]. Age related changes in the state of aggregation, as e.g. also in age-related macular degeneration, are suspected to alter the degree of polimerization and also the pro-oxidant state of the melanin polymer, thus possibly interfering with the digestion of cellular components including outer segment components [37].
Oxidative stress is recognized as a major pathogenic factor in age-related macular degeneration [38]. Diabetic conditions may lead to the accumulation of advanced glycation end products (AGEs) e.g. in the retinal pigment epithelium cell layers or photoreceptors [38, 39]. AGEs and also RAGE (receptor for AGEs) were also found in the retinal pigment epithelium or the retinal pigment epithelium and the photoreceptors in the maculae of human donor retina from patients with AMD, indicating to some extent similar biological pathways in AMD and diabetes [38, 40]. In the present study, antibodies against insulin were significantly upregulated in AMD patients.
Molecular chaperones and heat shock proteins are regulators for protein trafficking through cell organelle membranes and play a role in chaperoning damaged proteins to either the proteasome or lysosome for degredation [41, 42]. As stated above, autoantibodies against heat shock 70kDa protein 1A were significantly upregulated in the AMD 1 group in this investigation.
Logistic regression analysis showed, that the association between AMD and autoantibody level was still present after adjustment for smoking, body-mass-index, HbA1c level, level of high-density lipoproteins, of low-density lipoproteins and triglycerides in case of mitogen-activated protein kinase 3, lysozyme, transferrin and protein kinase C substrate 80K-H , insulin and heat shock 70 kDa protein 1A.
In general, it remains unclear whether the described autoantibodies play a causative role during the pathogenesis of AMD or appear as secondary effects during the disease’s progression. Several studies reported the involvement of antiretinal autoantibodies in age-related macular degeneration [10, 11, 43, 44]. Moreover, it has been suggested that certain autoantibody signatures may exist in different stages of age-related macular degeneration [11]. However, it still has to be elucidated whether the detected autoantibodies play a causative role in the pathogenesis of AMD or appear as secondary effects. Although the role of anti-retinal autoantibodies in the induction or progress of retinal degeneration presently is not well defined, it has been shown that anti-retinal autoantibodies can develop on average 3-15 years prior to the first clinical signs [45, 46]. In order to clarify the question whether the antiretinal autoantibodies play a causative role, future longitudinal studies, possibly with additional mass spectrometry to detect associated proteins, could be desirable.
Previous studies indicate that a causal association of autoantibodies with either pathogenesis or progression of AMD will require a higher number of subjects with early and late stages of AMD and that serum samples collected from the same patient, before and after AMD development or during progression of disease are not generally accessible [45]. A comparison of the retinal autoantibody profile in 63 individuals with and without early AMD from the Blue Mountains Eye Study showed an enhanced autoantibody response in early AMD [10]. In the GHS, the baseline examination with a total of 15,010 participants aged 35 to 74 years was conducted from 2007 to 2012. In this study, we evaluated data from a subsample of 1031 subjects enrolled in the GHS. In subsequent reports, after the 5- and 10-year follow-up of the same participants, the presence of antiretinal autoantibodies in early AMD stages might be associated with progression to later stages of AMD. Identification of serum autoantibodies associated with AMD might thus serve as a screening tool for prediction, give invaluable hints regarding prognosis as well as possibly monitor treatment response to intravitreal therapy in the future.
Strengths of the present study are the analysis by antigen-microarrays, an attractive tool which allows fast evaluation with high sensitivity of potential autoantibody biomarkers using microliter sample volumes. The present GHS study has a population-based, prospective design with broad assessment of phenotype information and large sample size. Fundus pictures of all participants and participants without AMD were graded independently by two experienced graders. This, to our knowledge, is the first report on microarray-based evaluation of autoantibody-levels in different AMD stages in a large German population-based cohort.
Since the GHS baseline recruitment was limited to participants below the age of 75, there were only 23 participants with AMD Stage 3 or 4, so these subjects had to be excluded for further statistical analysis. In addition, due to the relatively young age at the time of study entry, there were only 64 participants with AMD Stage 2 compared to 454 participants with AMD Stage 1 and 490 controls. The different group size explains the fact that significant differences in the antibody profile were only found between the controls and participants with AMD Stage 1. Subsequent reports will provide data on the autoantibody profile in different AMD stages compared to healthy controls after 5- and 10-year follow-up.
Any extrapolation to other populations should be done with caution, as the GHS cohort is predominantly Caucasian and of European ancestry. Although the age range reflects a broad proportion of the population, extrapolation of our data to other age groups may not be valid, especially as AMD is strongly associated with age.
Conclusion
This study contributes towards a growing knowledge of autoantibodies in association with AMD by a microarray-based evaluation of human sera in the context of a large population-based, prospective, observational cohort study in Germany. Especially autoantibodies against inflammatory proteins were downregulated in participants with AMD.
Data availability
The analysis presents clinical data of a large-scale population-based cohort with ongoing follow-up examinations. This project constitutes a major scientific effort with high methodological standards and detailed guidelines for analysis and publication to ensure scientific analyses on highest level. Therefore, data are not made available for the scientific community outside the established and controlled workflows and algorithms. To meet the general idea of verification and reproducibility of scientific findings, we offer access to data at the local database in accordance with the ethics vote upon request at any time. The GHS steering committee, which comprises a member of each involved department and the head of the Gutenberg Health Study (PSW), convenes once a month. The steering committee decides on internal and external access of researchers and use of the data and biomaterials based on a research proposal to be supplied by the researcher. Interested researchers make their requests to the head of the Gutenberg Health Study (Philipp S. Wild; philipp.wild@unimedizin-mainz.de). More detailed contact information is available at the homepages of the GHS (www.gutenberghealthstudy.org) or the ophthalmic branch of the GHS (www.unimedizin-mainz.de/augenklinik/forschung/gutenberg-gesundheitsstudie.html).
Abbreviations
- AMD:
-
age-related macular degeneration
- GHS:
-
Gutenberg Health Study
- PBS:
-
phosphate-buffered saline
- MAPK:
-
mitogen-activated protein kinase
- ROS:
-
reactive oxygen species
- RPE:
-
retinal pigment epithelium
- Anti-CA II:
-
anti-carbonic anhydrase II
- CAR:
-
cancer-associated retinopathy
- AGE:
-
advanced glycation end products
- RAGE:
-
receptor for advanced glycation end products
- BMI:
-
body mass index
- Hba1c:
-
glycated hemoglobin
- HDL:
-
high-density lipoproteins
- LDL:
-
low-density lipoproteins
- OR:
-
odds ratio
References
Lim LS, Mitchell P, Seddon JM, Holz FG, Wong TY (2012) Age-related macular degeneration. Lancet 379(9827):1728–1738
Korb CA, Kottler UB, Wolfram C, Hoehn R, Schulz A, Zwiener I, Wild PS, Pfeiffer N, Mirshahi A (2014) Prevalence of age-related macular degeneration in a large European cohort: results from the population-based Gutenberg Health Study. Graefes Arch Clin Exp Ophthalmol 252(9):1403–1411. https://doi.org/10.1007/s00417-014-2591-9
Dumonde DC, Kasp-Grochowska E, Graham E, Sanders MD, Faure JP, de Kozak Y, van Tuyen V (1982) Anti-retinal autoimmunity and circulating immune complexes in patients with retinal vasculitis. Lancet 2(8302):787–792
Heckenlively JR, Fawzi AA, Oversier J, Jordan BL, Aptsiauri N (2000) Autoimmune retinopathy: patients with antirecoverin immunoreactivity and panretinal degeneration. Arch Ophthalmol 118(11):1525–1533
Savchenko MS, Bazhin AV, Shifrina ON, Demoura SA, Kogan EA, Chuchalin AG, Philippov PP (2003) Antirecoverin autoantibodies in the patient with non-small cell lung cancer but without cancer-associated retinopathy. Lung Cancer 41(3):363–367
Galbraith GM, Emerson D, Fudenberg HH, Gibbs CJ, Gajdusek DC (1986) Antibodies to neurofilament protein in retinitis pigmentosa. J Clin Invest 78(4):865–869. https://doi.org/10.1172/JCI112672
Penfold PL, Provis JM, Furby JH, Gatenby PA, Billson FA (1990) Autoantibodies to retinal astrocytes associated with age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol 228(3):270–274
Gurne DH, Tso MO, Edward DP, Ripps H (1991) Antiretinal antibodies in serum of patients with age-related macular degeneration. Ophthalmology 98(5):602–607
Chen H, Wu L, Pan S, Wu DZ (1993) An immunologic study on age-related macular degeneration. Yan Ke Xue Bao 9(3):113–120
Cherepanoff S, Mitchell P, Wang JJ, Gillies MC (2006) Retinal autoantibody profile in early age-related macular degeneration: preliminary findings from the Blue Mountains Eye Study. Clin Experiment Ophthalmol 34(6):590–595. https://doi.org/10.1111/j.1442-9071.2006.01281.x
Adamus G, Chew EY, Ferris FL, Klein ML (2014) Prevalence of anti-retinal autoantibodies in different stages of Age-related macular degeneration. BMC Ophthalmol 14:154. https://doi.org/10.1186/1471-2415-14-154
Morohoshi K, Ohbayashi M, Patel N, Chong V, Bird AC, Ono SJ (2012) Identification of anti-retinal antibodies in patients with age-related macular degeneration. Exp Mol Pathol 93(2):193–199. https://doi.org/10.1016/j.yexmp.2012.03.007
Joachim SC, Bruns K, Lackner KJ, Pfeiffer N, Grus FH (2007) Analysis of IgG antibody patterns against retinal antigens and antibodies to alpha-crystallin, GFAP, and alpha-enolase in sera of patients with "wet" age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol 245(5):619–626. https://doi.org/10.1007/s00417-006-0429-9
Wild PS, Zeller T, Beutel M, Blettner M, Dugi KA, Lackner KJ, Pfeiffer N, Munzel T, Blankenberg S (2012) The Gutenberg Health Study. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 55(6-7):824–829. https://doi.org/10.1007/s00103-012-1502-7
Höhn R, Kottler U, Peto T, Blettner M, Munzel T, Blankenberg S, Lackner KJ, Beutel M, Wild PS, Pfeiffer N (2015) The Ophthalmic Branch of the Gutenberg Health Study: Study Design, Cohort Profile and Self-Reported Diseases. PloS One 10(3):e0120476. https://doi.org/10.1371/journal.pone.0120476
van Leeuwen R, Klaver CC, Vingerling JR, Hofman A, de Jong PT (2003) The risk and natural course of age-related maculopathy: follow-up at 6 1/2 years in the Rotterdam study. Arch Ophthalmol 121(4):519–526. https://doi.org/10.1001/archopht.121.4.519
Chowers I, Wong R, Dentchev T, Farkas RH, Iacovelli J, Gunatilaka TL, Medeiros NE, Presley JB, Campochiaro PA, Curcio CA, Dunaief JL, Zack DJ (2006) The iron carrier transferrin is upregulated in retinas from patients with age-related macular degeneration. Invest Ophthalmol Vis Sci 47(5):2135–2140. https://doi.org/10.1167/iovs.05-1135
Wysokinski D, Danisz K, Blasiak J, Dorecka M, Romaniuk D, Szaflik J, Szaflik JP (2013) An association of transferrin gene polymorphism and serum transferrin levels with age-related macular degeneration. Exp Eye Res 106:14–23. https://doi.org/10.1016/j.exer.2012.10.003
Yang P, Baciu P, Kerrigan BC, Etheridge M, Sung E, Toimil BA, Berchuck JE, Jaffe GJ (2014) Retinal pigment epithelial cell death by the alternative complement cascade: role of membrane regulatory proteins, calcium, PKC, and oxidative stress. Invest Ophthalmol Vis Sci 55(5):3012–3021. https://doi.org/10.1167/iovs.13-13554
Lores-Motta L, Paun CC, Corominas J, Pauper M, Geerlings MJ, Altay L, Schick T, Daha MR, Fauser S, Hoyng CB, den Hollander AI, de Jong EK (2018) Genome-Wide Association Study Reveals Variants in CFH and CFHR4 Associated with Systemic Complement Activation: Implications in Age-Related Macular Degeneration. Ophthalmology 125(7):1064–1074. https://doi.org/10.1016/j.ophtha.2017.12.023
Whitmore SS, Sohn EH, Chirco KR, Drack AV, Stone EM, Tucker BA, Mullins RF (2015) Complement activation and choriocapillaris loss in early AMD: implications for pathophysiology and therapy. Prog Retin Eye Res 45:1–29. https://doi.org/10.1016/j.preteyeres.2014.11.005
Zhang YQ, Fan YG, Dang YL, Liu YL, Liu H, Li LH (2017) Down-regulation of protein kinase C alpha/ezrin signals in light-induced phagocytic crisis of retinal pigment epithelium cells. Int J Ophthalmol 10(7):1040–1045. https://doi.org/10.18240/ijo.2017.07.04
Ng T, Parsons M, Hughes WE, Monypenny J, Zicha D, Gautreau A, Arpin M, Gschmeissner S, Verveer PJ, Bastiaens PI, Parker PJ (2001) Ezrin is a downstream effector of trafficking PKC-integrin complexes involved in the control of cell motility. EMBO J 20(11):2723–2741. https://doi.org/10.1093/emboj/20.11.2723
Hollyfield JG (2010) Age-related macular degeneration: the molecular link between oxidative damage, tissue-specific inflammation and outer retinal disease: the Proctor lecture. Invest Ophthalmol Vis Sci 51(3):1275–1281. https://doi.org/10.1167/iovs.09-4478
Kyosseva SV (2016) Targeting MAPK Signaling in Age-Related Macular Degeneration. Ophthalmol Eye Dis 8:23–30. https://doi.org/10.4137/OED.S32200
Chan CM, Huang CH, Li HJ, Hsiao CY, Su CC, Lee PL, Hung CF (2015) Protective effects of resveratrol against UVA-induced damage in ARPE19 cells. Int J Mol Sci 16(3):5789–5802. https://doi.org/10.3390/ijms16035789
Torres M, Forman HJ (2003) Redox signaling and the MAP kinase pathways. Biofactors 17(1-4):287–296
Koinzer S, Reinecke K, Herdegen T, Roider J, Klettner A (2015) Oxidative Stress Induces Biphasic ERK1/2 Activation in the RPE with Distinct Effects on Cell Survival at Early and Late Activation. Curr Eye Res 40(8):853–857. https://doi.org/10.3109/02713683.2014.961613
Dridi S, Hirano Y, Tarallo V, Kim Y, Fowler BJ, Ambati BK, Bogdanovich S, Chiodo VA, Hauswirth WW, Kugel JF, Goodrich JA, Ponicsan SL, Hinton DR, Kleinman ME, Baffi JZ, Gelfand BD, Ambati J (2012) ERK1/2 activation is a therapeutic target in age-related macular degeneration. Proc Natl Acad Sci U S A 109(34):13781–13786. https://doi.org/10.1073/pnas.1206494109
Adamus G, Yang S, Weleber RG (2016) Unique epitopes for carbonic anhydrase II autoantibodies related to autoimmune retinopathy and cancer-associated retinopathy. Exp Eye Res 147:161–168. https://doi.org/10.1016/j.exer.2016.05.012
Adamus G (2009) Autoantibody targets and their cancer relationship in the pathogenicity of paraneoplastic retinopathy. Autoimmun Rev 8(5):410–414. https://doi.org/10.1016/j.autrev.2009.01.002
Adamus G, Karren L (2009) Autoimmunity against carbonic anhydrase II affects retinal cell functions in autoimmune retinopathy. J Autoimmun 32(2):133–139. https://doi.org/10.1016/j.jaut.2009.02.001
Taniguchi T, Okazaki K, Okamoto M, Seko S, Tanaka J, Uchida K, Nagashima K, Kurose T, Yamada Y, Chiba T, Seino Y (2003) High prevalence of autoantibodies against carbonic anhydrase II and lactoferrin in type 1 diabetes: concept of autoimmune exocrinopathy and endocrinopathy of the pancreas. Pancreas 27(1):26–30
Bournia VK, Vlachoyiannopoulos PG (2012) Subgroups of Sjogren syndrome patients according to serological profiles. J Autoimmun 39(1-2):15–26. https://doi.org/10.1016/j.jaut.2012.03.001
Itoh Y, Reichlin M (1992) Antibodies to carbonic anhydrase in systemic lupus erythematosus and other rheumatic diseases. Arthritis Rheum 35(1):73–82
Frederick PA, Kleinman ME (2014) The Immune System and AMD. Curr Ophthalmol Rep 2(1):14–19. https://doi.org/10.1007/s40135-013-0037-x
Sarangarajan R, Apte SP (2005) Melanin aggregation and polymerization: possible implications in age-related macular degeneration. Ophthalmic Res 37(3):136–141. https://doi.org/10.1159/000085533
Ardeljan D, Chan CC (2013) Aging is not a disease: distinguishing age-related macular degeneration from aging. Prog Retin Eye Res 37:68–89. https://doi.org/10.1016/j.preteyeres.2013.07.003
Stitt AW (2010) AGEs and diabetic retinopathy. Invest Ophthalmol Vis Sci 51(10):4867–4874. https://doi.org/10.1167/iovs.10-5881
Howes KA, Liu Y, Dunaief JL, Milam A, Frederick JM, Marks A, Baehr W (2004) Receptor for advanced glycation end products and age-related macular degeneration. Invest Ophthalmol Vis Sci 45(10):3713–3720. https://doi.org/10.1167/iovs.04-0404
Kaarniranta K, Sinha D, Blasiak J, Kauppinen A, Vereb Z, Salminen A, Boulton ME, Petrovski G (2013) Autophagy and heterophagy dysregulation leads to retinal pigment epithelium dysfunction and development of age-related macular degeneration. Autophagy 9(7):973–984. https://doi.org/10.4161/auto.24546
Ferrington DA, Sinha D, Kaarniranta K (2016) Defects in retinal pigment epithelial cell proteolysis and the pathology associated with age-related macular degeneration. Prog Retin Eye Res 51:69–89. https://doi.org/10.1016/j.preteyeres.2015.09.002
Patel N, Ohbayashi M, Nugent AK, Ramchand K, Toda M, Chau KY, Bunce C, Webster A, Bird AC, Ono SJ, Chong V (2005) Circulating anti-retinal antibodies as immune markers in age-related macular degeneration. Immunology 115(3):422–430. https://doi.org/10.1111/j.1365-2567.2005.02173.x
Morohoshi K, Goodwin AM, Ohbayashi M, Ono SJ (2009) Autoimmunity in retinal degeneration: autoimmune retinopathy and age-related macular degeneration. J Autoimmun 33(3-4):247–254. https://doi.org/10.1016/j.jaut.2009.09.003
Adamus G (2017) Can innate and autoimmune reactivity forecast early and advance stages of age-related macular degeneration? Autoimmun Rev 16(3):231–236. https://doi.org/10.1016/j.autrev.2017.01.005
Deane KD (2014) Preclinical rheumatoid arthritis (autoantibodies): an updated review. Curr Rheumatol Rep 16(5):419. https://doi.org/10.1007/s11926-014-0419-6
Acknowledgments
We thank all study participants for their willingness to provide data for this research project, and we are indebted to all coworkers for their enthusiastic commitment.
Funding
Open Access funding enabled and organized by Projekt DEAL. The Gutenberg Health Study is funded through the government of Rhineland-Palatinate (“Stiftung Rheinland-Pfalz für Innovation“, contract AZ 961-386261/733), the research programs “Wissen schafft Zukunft” and “Center for Translational Vascular Biology (CTVB)” of the Johannes Gutenberg-University of Mainz, and its contracts with Boehringer Ingelheim and PHILIPS Medical Systems, including unrestricted grants for the Gutenberg Health Study. This analysis was supported by Novartis Pharma GmbH. Philipp S. Wild is funded by the Federal Ministry of Education and Research (BMBF 01EO1503), and he is the PI of the German Center for Cardiovascular Research (DZHK). Schuster AK holds the professorship for ophthalmic healthcare research donated by „Stiftung Auge“ and financed by „Deutsche Ophthalmologische Gesellschaft“ and „Berufsverband der Augenärzte Deutschlands e.V.“ He received research funding from Bayer Vital, Novartis and Heidelberg Engineering.
Author information
Authors and Affiliations
Contributions
Conceived and designed the study: CAK, KJL , DW, AKS, SN, VMB, TM , PSW, MEB, IS, NP, FHG; analyzed and interpreted the data: CAK, KJL, DW , AKS, SN, VMB, TM , PSW, MEB, IS, NP, FHG; wrote the paper: CAK, AKS, DW, VMB, NP, FHG; all authors revised the manuscript critically and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol and study documents were approved by the local ethics committee of the Medical Chamber of Rhineland-Palatinate, Germany (reference no. 837.020.07; original vote: 22.3.2007, latest update: 20.10.2015). According to the tenets of the Declaration of Helsinki, written informed consent was obtained from all participants prior to entering the study.
Competing interests
The authors declare that they have no competing interests that are relevant to the content of this article.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 17 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Korb, C.A., Lackner, K.J., Wolters, D. et al. Association of autoantibody levels with different stages of age-related macular degeneration (AMD): Results from the population-based Gutenberg Health Study (GHS). Graefes Arch Clin Exp Ophthalmol 261, 2763–2773 (2023). https://doi.org/10.1007/s00417-023-06085-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-023-06085-2