Abstract
Background
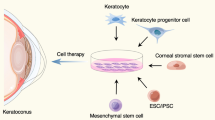
Keratoconus is a corneal ectatic disease caused by stromal thinning leading to astigmatism and progressive loss of vision. Loss of the keratocytes and excessive degradation of collagen fibres by matrix metalloproteinases are the molecular signatures of the disease. Despite several limitations, corneal collagen cross-linking and keratoplasty are the most widely used treatment options for keratoconus. In the pursuit of alternative treatment modalities, clinician scientists have explored cell therapy paradigms for treating the condition.
Methods
Articles pertaining to keratoconus cell therapy with relevant key words were used to search in PubMed, Researchgate, and Google Scholar. The articles were selected based on their relevance, reliability, publication year, published journal, and accessibility.
Results
Various cellular abnormalities have been reported in keratoconus. Diverse cell types such as mesenchymal stromal cells, dental pulp cells, bone marrow stem cells, haematopoietic stem cells, adipose-derived stem cells apart from embryonic and induced pluripotent stem cells can be used for keratoconus cell therapy. The results obtained show that there is a potential for these cells from various sources as a viable treatment option.
Conclusion
There is a need for consensus with respect to the source of cells, mode of delivery, stage of disease, and duration of follow-up, to establish a standard operating protocol. This would eventually widen the cell therapy options for corneal ectatic diseases beyond keratoconus.


Similar content being viewed by others
References
Shetty R, Vunnava KP, Dhamodaran K, Matalia H, Murali S, Jayadev C, Murugeswari P, Ghosh A, Das D (2019) Characterization of corneal epithelial cells in keratoconus. Transl Vis Sci Technol 8:2. https://doi.org/10.1167/tvst.8.1.2
Loh IP, Sherwin T (2020) Is keratoconus an inflammatory disease? The implication of inflammatory pathways. Ocul Immunol Inflamm: 1–10. https://doi.org/10.1080/09273948.2020.1780271
Sinha Roy A, Shetty R, Kummelil MK (2013) Keratoconus: a biomechanical perspective on loss of corneal stiffness. Indian J Ophthalmol 61:392–393. https://doi.org/10.4103/0301-4738.116057
Zadnik K, Barr JT, Edrington TB, Everett DF, Jameson M, McMahon TT, Shin JA, Sterling JL, Wagner H, Gordon MO (1998) Baseline findings in the Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study. Invest Ophthalmol Vis Sci 39:2537–2546
Nowak DM, Gajecka M (2011) The genetics of keratoconus. Middle East Afr J Ophthalmol 18:2–6. https://doi.org/10.4103/0974-9233.75876
Jeyabalan N, Shetty R, Ghosh A, Anandula VR, Ghosh AS, Kumaramanickavel G (2013) Genetic and genomic perspective to understand the molecular pathogenesis of keratoconus. Indian J Ophthalmol 61:384–388. https://doi.org/10.4103/0301-4738.116055
Shetty R, Sathyanarayanamoorthy A, Ramachandra RA, Arora V, Ghosh A, Srivatsa PR, Pahuja N, Nuijts RM, Sinha-Roy A, Mohan RR, Ghosh A (2015) Attenuation of lysyl oxidase and collagen gene expression in keratoconus patient corneal epithelium corresponds to disease severity. Mol Vis 21:12–25
Shetty R, Sharma A, Pahuja N, Chevour P, Padmajan N, Dhamodaran K, Jayadev C, Mman R, Ghosh A, Nallathambi J (2017) Oxidative stress induces dysregulated autophagy in corneal epithelium of keratoconus patients. PLoS One 12:e0184628. https://doi.org/10.1371/journal.pone.0184628
Pahuja N, Kumar NR, Shroff R, Shetty R, Nuijts RM, Ghosh A, Sinha-Roy A, Chaurasia SS, Mohan RR, Ghosh A (2016) Differential molecular expression of extracellular matrix and inflammatory genes at the corneal cone apex drives focal weakening in keratoconus. Invest Ophthalmol Vis Sci 57:5372–5382. https://doi.org/10.1167/iovs.16-19677
Shetty R, Ghosh A, Lim RR, Subramani M, Mihir K, Reshma AR, Ranganath A, Nagaraj S, Nuijts RM, Beuerman R, Shetty R, Das D, Chaurasia SS, Sinha-Roy A, Ghosh A (2015) Elevated expression of matrix metalloproteinase-9 and inflammatory cytokines in keratoconus patients is inhibited by cyclosporine A. Invest Ophthalmol Vis Sci 56:738–750. https://doi.org/10.1167/iovs.14-14831
Greene CA, Kuo C, Sherwin T (2017) Aberrant patterns of key epithelial basement membrane components in keratoconus. Cornea 36:1549–1555. https://doi.org/10.1097/ICO.0000000000001393
Karamichos D, Zieske JD, Sejersen H, Sarker-Nag A, Asara JM, Hjortdal J (2015) Tear metabolite changes in keratoconus. Exp Eye Res 132:1–8. https://doi.org/10.1016/j.exer.2015.01.007
McKay TB, Serjersen H, Hjortdal J, Zieske JD, Karamichos D (2020) Characterization of tear immunoglobulins in a small-cohort of keratoconus patients. Sci Rep 10:9426. https://doi.org/10.1038/s41598-020-66442-7
Li Y, Ismail S, McGhee JJ, Wadhwa H, Noord N, van der Werf B, Sherwin T (2021) Differences in sphere-forming cells from keratoconic and normal corneal tissue: Implications for keratoconus pathogenesis. Exp Eye Res 202:108301. https://doi.org/10.1016/j.exer.2020.108301
Hollingsworth JG, Bonshek RE, Efron N (2005) Correlation of the appearance of the keratoconic cornea in vivo by confocal microscopy and in vitro by light microscopy. Cornea 24:397–405. https://doi.org/10.1097/01.ico.0000151548.46231.27
Crespo Millas S, Lopez JC, Garcia-Lagarto E, Obregon E, Hileeto D, Maldonado MJ, Pastor JC (2020) Histological patterns of epithelial alterations in keratoconus. J Ophthalmol 2020:1468258. https://doi.org/10.1155/2020/1468258
Weed KH, MacEwen CJ, Cox A, McGhee CN (2007) Quantitative analysis of corneal microstructure in keratoconus utilising in vivo confocal microscopy. Eye (Lond) 21:614–623. https://doi.org/10.1038/sj.eye.6702286
Kaldawy RM, Wagner J, Ching S, Seigel GM (2002) Evidence of apoptotic cell death in keratoconus. Cornea 21:206–209. https://doi.org/10.1097/00003226-200203000-00017
Kim WJ, Rabinowitz YS, Meisler DM, Wilson SE (1999) Keratocyte apoptosis associated with keratoconus. Exp Eye Res 69:475–481. https://doi.org/10.1006/exer.1999.0719
Newsome DA, Foidart JM, Hassell JR, Krachmer JH, Rodrigues MM, Katz SI (1981) Detection of specific collagen types in normal and keratoconus corneas. Invest Ophthalmol Vis Sci 20:738–750
Ebihara N, Watanabe Y, Nakayasu K, Kanai A (2001) The expression of laminin-5 and ultrastructure of the interface between basal cells and underlying stroma in the keratoconus cornea. Jpn J Ophthalmol 45:209–215. https://doi.org/10.1016/s0021-5155(01)00328-8
Ku JY, Niederer RL, Patel DV, Sherwin T, McGhee CN (2008) Laser scanning in vivo confocal analysis of keratocyte density in keratoconus. Ophthalmology 115:845–850. https://doi.org/10.1016/j.ophtha.2007.04.067
Alio JL, Pinero DP, Aleson A, Teus MA, Barraquer RI, Murta J, Maldonado MJ, Castro de Luna G, Gutierrez R, Villa C, Uceda-Montanes A (2011) Keratoconus-integrated characterization considering anterior corneal aberrations, internal astigmatism, and corneal biomechanics. J Cataract Refract Surg 37:552–568. https://doi.org/10.1016/j.jcrs.2010.10.046
Wilson SE, He YG, Weng J, Li Q, McDowall AW, Vital M, Chwang EL (1996) Epithelial injury induces keratocyte apoptosis: hypothesized role for the interleukin-1 system in the modulation of corneal tissue organization and wound healing. Exp Eye Res 62:325–327. https://doi.org/10.1006/exer.1996.0038
Soiberman U, Foster JW, Jun AS, Chakravarti S (2017) Pathophysiology of keratoconus: what do we know today. Open Ophthalmol J 11:252–261. https://doi.org/10.2174/1874364101711010252
Joseph R, Srivastava OP, Pfister RR (2011) Differential epithelial and stromal protein profiles in keratoconus and normal human corneas. Exp Eye Res 92:282–298. https://doi.org/10.1016/j.exer.2011.01.008
Edwards M, McGhee CN, Dean S (2001) The genetics of keratoconus. Clin Exp Ophthalmol 29:345–351. https://doi.org/10.1046/j.1442-9071.2001.d01-16.x
Volatier TLA, Figueiredo FC, Connon CJ (2020) Keratoconus at a molecular level: a review. Anat Rec (Hoboken) 303:1680–1688. https://doi.org/10.1002/ar.24090
Ucakhan OO, Kanpolat A, Ylmaz N, Ozkan M (2006) In vivo confocal microscopy findings in keratoconus. Eye Contact Lens 32:183–191. https://doi.org/10.1097/01.icl.0000189038.74139.4a
Sharif R, Khaled ML, McKay TB, Liu Y, Karamichos D (2019) Transcriptional profiling of corneal stromal cells derived from patients with keratoconus. Sci Rep 9:12567. https://doi.org/10.1038/s41598-019-48983-8
Foster JW, Shinde V, Soiberman US, Sathe G, Liu S, Wan J, Qian J, Dauoud Y, Pandey A, Jun AS, Chakravarti S (2018) Integrated stress response and decreased ECM in cultured stromal cells from keratoconus corneas. Invest Ophthalmol Vis Sci 59:2977–2986. https://doi.org/10.1167/iovs.18-24367
Bitirgen G, Ozkagnici A, Bozkurt B, Malik RA (2015) In vivo corneal confocal microscopic analysis in patients with keratoconus. Int J Ophthalmol 8:534–539. https://doi.org/10.3980/j.issn.2222-3959.2015.03.17
Edelhauser HF (2006) The balance between corneal transparency and edema: the Proctor Lecture. Invest Ophthalmol Vis Sci 47:1754–1767. https://doi.org/10.1167/iovs.05-1139
de Abreu Fiuza Gomes BGVPL GVP (2021) A correlation study between a corneal endothelial count in patients with different stages of keratoconus using specular microscopy. Revista Brasileira de Oftalmologia 80:107–110
Shah Z, Shilpy N, Purohit D, Singh S (2021) Assessment and correlation of corneal endothelial cell changes in different stages of keratoconus in non-contact lens wearers. Optom Vis Sci. https://doi.org/10.1097/OPX.0000000000001805
Elmassry A, Osman A, Sabry M, Elmassry M, Katkat M, Hatata MY, El-Kateb M (2021) Corneal endothelial cells changes in different stages of keratoconus: a multi-centre clinical study. BMC Ophthalmol 21:143. https://doi.org/10.1186/s12886-021-01913-7
Dogru M, Karakaya H, Ozcetin H, Erturk H, Yucel A, Ozmen A, Baykara M, Tsubota K (2003) Tear function and ocular surface changes in keratoconus. Ophthalmology 110:1110–1118. https://doi.org/10.1016/S0161-6420(03)00261-6
Shetty R, Deshmukh R, Ghosh A, Sethu S, Jayadev C (2017) Altered tear inflammatory profile in Indian keratoconus patients - the 2015 Col Rangachari Award paper. Indian J Ophthalmol 65:1105–1108. https://doi.org/10.4103/ijo.IJO_233_17
Lema I, Duran JA, Ruiz C, Diez-Feijoo E, Acera A, Merayo J (2008) Inflammatory response to contact lenses in patients with keratoconus compared with myopic subjects. Cornea 27:758–763. https://doi.org/10.1097/ICO.0b013e31816a3591
Lema I, Duran JA (2005) Inflammatory molecules in the tears of patients with keratoconus. Ophthalmology 112:654–659. https://doi.org/10.1016/j.ophtha.2004.11.050
Balasubramanian SA, Mohan S, Pye DC, Willcox MD (2012) Proteases, proteolysis and inflammatory molecules in the tears of people with keratoconus. Acta Ophthalmol 90:e303-309. https://doi.org/10.1111/j.1755-3768.2011.02369.x
You J, Hodge C, Wen L, McAvoy JW, Madigan MC, Sutton G (2013) Tear levels of SFRP1 are significantly reduced in keratoconus patients. Mol Vis 19:509–xxx
Nishtala K, Pahuja N, Shetty R, Nuijts RM, Ghosh A (2016) Tear biomarkers for keratoconus. Eye Vis (Lond) 3:19. https://doi.org/10.1186/s40662-016-0051-9
Benhar I, London A, Schwartz M (2012) The privileged immunity of immune privileged organs: the case of the eye. Front Immunol 3:296. https://doi.org/10.3389/fimmu.2012.00296
Taylor AW (2016) Ocular immune privilege and transplantation. Front Immunol 7:37. https://doi.org/10.3389/fimmu.2016.00037
Griffith M, Alarcon EI, Brunette I (2016) Regenerative approaches for the cornea. J Intern Med 280:276–286. https://doi.org/10.1111/joim.12502
Yam GHF, Riau AK, Funderburgh ML, Mehta JS, Jhanji V (2020) Keratocyte biology. Exp Eye Res 196:108062. https://doi.org/10.1016/j.exer.2020.108062
Massoudi D, Malecaze F, Galiacy SD (2016) Collagens and proteoglycans of the cornea: importance in transparency and visual disorders. Cell Tissue Res 363:337–349. https://doi.org/10.1007/s00441-015-2233-5
Coulombre AJ, Coulombre JL (1958) Corneal development. I Corneal transparency. J Cell Comp Physiol 51:1–11. https://doi.org/10.1002/jcp.1030510102
Chakravarti S, Magnuson T, Lass JH, Jepsen KJ, LaMantia C, Carroll H (1998) Lumican regulates collagen fibril assembly: skin fragility and corneal opacity in the absence of lumican. J Cell Biol 141:1277–1286. https://doi.org/10.1083/jcb.141.5.1277
Fini ME, Stramer BM (2005) How the cornea heals: cornea-specific repair mechanisms affecting surgical outcomes. Cornea 24:S2–S11. https://doi.org/10.1097/01.ico.0000178743.06340.2c
West-Mays JA, Dwivedi DJ (2006) The keratocyte: corneal stromal cell with variable repair phenotypes. Int J Biochem Cell Biol 38:1625–1631. https://doi.org/10.1016/j.biocel.2006.03.010
Somodi S, Guthoff R (1995) Visualization of keratocytes in the human cornea with fluorescence microscopy. Ophthalmologe 92:452–457
Hahnel C, Somodi S, Weiss DG, Guthoff RF (2000) The keratocyte network of human cornea: a three-dimensional study using confocal laser scanning fluorescence microscopy. Cornea 19:185–193. https://doi.org/10.1097/00003226-200003000-00012
Jester JV, Ho-Chang J (2003) Modulation of cultured corneal keratocyte phenotype by growth factors/cytokines control in vitro contractility and extracellular matrix contraction. Exp Eye Res 77:581–592. https://doi.org/10.1016/s0014-4835(03)00188-x
Midura RJ, Hascall VC (1989) Analysis of the proteoglycans synthesized by corneal explants from embryonic chicken. II. Structural characterization of the keratan sulfate and dermatan sulfate proteoglycans from corneal stroma. J Biol Chem 264:1423–1430
Klintworth GK, Smith CF (1983) Abnormalities of proteoglycans and glycoproteins synthesized by corneal organ cultures derived from patients with macular corneal dystrophy. Lab Invest 48:603–612
Funderburgh ML, Du Y, Mann MM, SundarRaj N, Funderburgh JL (2005) PAX6 expression identifies progenitor cells for corneal keratocytes. FASEB J 19:1371–1373. https://doi.org/10.1096/fj.04-2770fje
Funderburgh JL, Funderburgh ML, Mann MM, Prakash S, Conrad GW (1996) Synthesis of corneal keratan sulfate proteoglycans by bovine keratocytes in vitro. J Biol Chem 271:31431–31436. https://doi.org/10.1074/jbc.271.49.31431
Beales MP, Funderburgh JL, Jester JV, Hassell JR (1999) Proteoglycan synthesis by bovine keratocytes and corneal fibroblasts: maintenance of the keratocyte phenotype in culture. Invest Ophthalmol Vis Sci 40:1658–1663
Foster JW, Gouveia RM, Connon CJ (2015) Low-glucose enhances keratocyte-characteristic phenotype from corneal stromal cells in serum-free conditions. Sci Rep 5:10839. https://doi.org/10.1038/srep10839
Yam GH, Yusoff NZ, Kadaba A, Tian D, Myint HH, Beuerman RW, Zhou L, Mehta JS (2015) Ex vivo propagation of human corneal stromal “activated keratocytes” for tissue engineering. Cell Transplant 24:1845–1861. https://doi.org/10.3727/096368914X685069
Yam GH, Fuest M, Yusoff N, Goh TW, Bandeira F, Setiawan M, Seah XY, Lwin NC, Stanzel TP, Ong HS, Mehta JS (2018) Safety and feasibility of intrastromal injection of cultivated human corneal stromal keratocytes as cell-based therapy for corneal opacities. Invest Ophthalmol Vis Sci 59:3340–3354. https://doi.org/10.1167/iovs.17-23575
Shafiq MA, Gemeinhart RA, Yue BY, Djalilian AR (2012) Decellularized human cornea for reconstructing the corneal epithelium and anterior stroma. Tissue Eng Part C Methods 18:340–348. https://doi.org/10.1089/ten.TEC.2011.0072
Pinnamaneni N, Funderburgh JL (2012) Concise review: Stem cells in the corneal stroma. Stem Cells 30:1059–1063. https://doi.org/10.1002/stem.1100
Du Y, Funderburgh ML, Mann MM, SundarRaj N, Funderburgh JL (2005) Multipotent stem cells in human corneal stroma. Stem Cells 23:1266–1275. https://doi.org/10.1634/stemcells.2004-0256
Patel DV, McKelvie J, Sherwin T, McGhee C (2013) Keratocyte progenitor cell transplantation: a novel therapeutic strategy for corneal disease. Med Hypotheses 80:122–124. https://doi.org/10.1016/j.mehy.2012.11.006
Funderburgh JL, Mann MM, Funderburgh ML, Roh DS, Du Y (2010) CD271 is a Cell-Surface Marker of Keratocyte Progenitor Cells. Invest Ophthalmol Visual Sci 51:2952–2952
Amano S, Yamagami S, Mimura T, Uchida S, Yokoo S (2006) Corneal stromal and endothelial cell precursors. Cornea 25:S73-77. https://doi.org/10.1097/01.ico.0000247218.10672.7e
Yamagami S, Yokoo S, Mimura T, Takato T, Araie M, Amano S (2007) Distribution of precursors in human corneal stromal cells and endothelial cells. Ophthalmology 114:433–439. https://doi.org/10.1016/j.ophtha.2006.07.042
Branch MJ, Hashmani K, Dhillon P, Jones DR, Dua HS, Hopkinson A (2012) Mesenchymal stem cells in the human corneal limbal stroma. Invest Ophthalmol Vis Sci 53:5109–5116. https://doi.org/10.1167/iovs.11-8673
Nurkovic JS, Vojinovic R, Dolicanin Z (2020) Corneal stem cells as a source of regenerative cell-based therapy. Stem Cells Int 2020:8813447. https://doi.org/10.1155/2020/8813447
Kureshi AK, Funderburgh JL, Daniels JT (2014) Human corneal stromal stem cells exhibit survival capacity following isolation from stored organ-culture corneas. Invest Ophthalmol Vis Sci 55:7583–7588. https://doi.org/10.1167/iovs.14-14448
Funderburgh JL, Funderburgh ML, Du Y (2016) Stem cells in the limbal stroma. Ocul Surf 14:113–120. https://doi.org/10.1016/j.jtos.2015.12.006
Dhamodaran K, Subramani M, Jeyabalan N, Ponnalagu M, Chevour P, Shetty R, Matalia H, Shetty R, Prince SE, Das D (2015) Characterization of ex vivo cultured limbal, conjunctival, and oral mucosal cells: a comparative study with implications in transplantation medicine. Mol Vis 21:828–845
Hashmani K, Branch MJ, Sidney LE, Dhillon PS, Verma M, McIntosh OD, Hopkinson A, Dua HS (2013) Characterization of corneal stromal stem cells with the potential for epithelial transdifferentiation. Stem Cell Res Ther 4:75. https://doi.org/10.1186/scrt226
Liu L, Yu Y, Peng Q, Porsborg SR, Nielsen FM, Jorgensen A, Grove A, Bath C, Hjortdal J, Christiansen OB, Fink T, Zachar V (2020) Distribution of stromal cell subsets in cultures from distinct ocular surface compartments. J Ophthalmic Vis Res 15:493–501. https://doi.org/10.18502/jovr.v15i4.7780
Du Y, Sundarraj N, Funderburgh ML, Harvey SA, Birk DE, Funderburgh JL (2007) Secretion and organization of a cornea-like tissue in vitro by stem cells from human corneal stroma. Invest Ophthalmol Vis Sci 48:5038–5045. https://doi.org/10.1167/iovs.07-0587
Wu J, Du Y, Mann MM, Funderburgh JL, Wagner WR (2014) Corneal stromal stem cells versus corneal fibroblasts in generating structurally appropriate corneal stromal tissue. Exp Eye Res 120:71–81. https://doi.org/10.1016/j.exer.2014.01.005
Sidney LE, Branch MJ, Dua HS, Hopkinson A (2015) Effect of culture medium on propagation and phenotype of corneal stroma-derived stem cells. Cytotherapy 17:1706–1722. https://doi.org/10.1016/j.jcyt.2015.08.003
Vereb Z, Poliska S, Albert R, Olstad OK, Boratko A, Csortos C, Moe MC, Facsko A, Petrovski G (2016) Role of human corneal stroma-derived mesenchymal-like stem cells in corneal immunity and wound healing. Sci Rep 6:26227. https://doi.org/10.1038/srep26227
Basu S, Hertsenberg AJ, Funderburgh ML, Burrow MK, Mann MM, Du Y, Lathrop KL, Syed-Picard FN, Adams SM, Birk DE, Funderburgh JL (2014) Human limbal biopsy-derived stromal stem cells prevent corneal scarring. Sci Transl Med 6:266ra172. https://doi.org/10.1126/scitranslmed.3009644
Mimura T, Amano S, Yokoo S, Uchida S, Yamagami S, Usui T, Kimura Y, Tabata Y (2008) Tissue engineering of corneal stroma with rabbit fibroblast precursors and gelatin hydrogels. Mol Vis 14:1819–1828
Wadhwa H, Ismail S, McGhee JJ, Van der Werf B, Sherwin T (2020) Sphere-forming corneal cells repopulate dystrophic keratoconic stroma: implications for potential therapy. World J Stem Cells 12:35–54. https://doi.org/10.4252/wjsc.v12.i1.35
Di Girolamo N (2011) Stem cells of the human cornea. Br Med Bull 100:191–207. https://doi.org/10.1093/bmb/ldr026
Alio Del Barrio JL, Alio JL (2018) Cellular therapy of the corneal stroma: a new type of corneal surgery for keratoconus and corneal dystrophies. Eye Vis (Lond) 5:28. https://doi.org/10.1186/s40662-018-0122-1
Mansoor H, Ong HS, Riau AK, Stanzel TP, Mehta JS, Yam GH (2019) Current trends and future perspective of mesenchymal stem cells and exosomes in corneal diseases. Int J Mol Sci 20 https://doi.org/10.3390/ijms20122853
Friedenstein AJ, Chailakhjan RK, Lalykina KS (1970) The development of fibroblast colonies in monolayer cultures of guinea-pig bone marrow and spleen cells. Cell Tissue Kinet 3:393–403. https://doi.org/10.1111/j.1365-2184.1970.tb00347.x
Caplan AI (1991) Mesenchymal stem cells. J Orthop Res 9:641–650. https://doi.org/10.1002/jor.1100090504
Phinney DG, Prockop DJ (2007) Concise review: mesenchymal stem/multipotent stromal cells: the state of transdifferentiation and modes of tissue repair–current views. Stem Cells 25:2896–2902. https://doi.org/10.1634/stemcells.2007-0637
Zhang L, Coulson-Thomas VJ, Ferreira TG, Kao WW (2015) Mesenchymal stem cells for treating ocular surface diseases. BMC Ophthalmol 15(Suppl 1):155. https://doi.org/10.1186/s12886-015-0138-4
Harkin DG, Foyn L, Bray LJ, Sutherland AJ, Li FJ, Cronin BG (2015) Concise reviews: can mesenchymal stromal cells differentiate into corneal cells? A systematic review of published data. Stem Cells 33:785–791. https://doi.org/10.1002/stem.1895
Hay ED (1980) Development of the vertebrate cornea. Int Rev Cytol 63:263–322. https://doi.org/10.1016/s0074-7696(08)61760-x
Alio Del Barrio JL, El Zarif M, de Miguel MP, Azaar A, Makdissy N, Harb W, El Achkar I, Arnalich-Montiel F, Alio JL (2017) Cellular therapy with human autologous adipose-derived adult stem cells for advanced keratoconus. Cornea 36:952–960. https://doi.org/10.1097/ICO.0000000000001228
Liu XN, Mi SL, Chen Y, Wang Y (2021) Corneal stromal mesenchymal stem cells: reconstructing a bioactive cornea and repairing the corneal limbus and stromal microenvironment. Int J Ophthalmol 14:448–455. https://doi.org/10.18240/ijo.2021.03.19
Arnalich-Montiel F, Pastor S, Blazquez-Martinez A, Fernandez-Delgado J, Nistal M, Alio JL, De Miguel MP (2008) Adipose-derived stem cells are a source for cell therapy of the corneal stroma. Stem Cells 26:570–579. https://doi.org/10.1634/stemcells.2007-0653
El Zarif M, Alio JL, Alio Del Barrio JL, De Miguel MP, Abdul Jawad K, Makdissy N (2021) Corneal stromal regeneration: a review of human clinical studies in keratoconus treatment. Front Med (Lausanne) 8:650724. https://doi.org/10.3389/fmed.2021.650724
Kao WW, Coulson-Thomas VJ (2016) Cell therapy of corneal diseases. Cornea 35(Suppl 1):S9–S19. https://doi.org/10.1097/ICO.0000000000001010
De Miguel MP, Fuentes-Julian S, Blazquez-Martinez A, Pascual CY, Aller MA, Arias J, Arnalich-Montiel F (2012) Immunosuppressive properties of mesenchymal stem cells: advances and applications. Curr Mol Med 12:574–591. https://doi.org/10.2174/156652412800619950
Zhu Q, Li M, Yan C, Lu Q, Wei S, Gao R, Yu M, Zou Y, Sriram G, Tong HJ, Hunziker W, Seneviratne CJ, Gong Z, Olsen BR, Cao T (2017) Directed differentiation of human embryonic stem cells to neural crest stem cells, functional peripheral neurons, and corneal keratocytes. Biotechnol J 12 https://doi.org/10.1002/biot.201700067
Chan AA, Hertsenberg AJ, Funderburgh ML, Mann MM, Du Y, Davoli KA, Mich-Basso JD, Yang L, Funderburgh JL (2013) Differentiation of human embryonic stem cells into cells with corneal keratocyte phenotype. PLoS One 8:e56831. https://doi.org/10.1371/journal.pone.0056831
Hertsenberg AJ, Funderburgh JL (2016) Generation of corneal keratocytes from human embryonic stem cells. Methods Mol Biol 1341:285–294. https://doi.org/10.1007/7651_2015_231
Kwack KH, Lee HW (2022) Clinical potential of dental pulp stem cells in pulp regeneration: current endodontic progress and future perspectives. Front Cell Dev Biol 10:857066. https://doi.org/10.3389/fcell.2022.857066
Yam GH, Peh GS, Singhal S, Goh BT, Mehta JS (2015) Dental stem cells: a future asset of ocular cell therapy. Expert Rev Mol Med 17:e20. https://doi.org/10.1017/erm.2015.16
Chalisserry EP, Nam SY, Park SH, Anil S (2017) Therapeutic potential of dental stem cells. J Tissue Eng 8:2041731417702531. https://doi.org/10.1177/2041731417702531
Yam GH, Teo EP, Setiawan M, Lovatt MJ, Yusoff N, Fuest M, Goh BT, Mehta JS (2018) Postnatal periodontal ligament as a novel adult stem cell source for regenerative corneal cell therapy. J Cell Mol Med 22:3119–3132. https://doi.org/10.1111/jcmm.13589
Syed-Picard FN, Du Y, Lathrop KL, Mann MM, Funderburgh ML, Funderburgh JL (2015) Dental pulp stem cells: a new cellular resource for corneal stromal regeneration. Stem Cells Transl Med 4:276–285. https://doi.org/10.5966/sctm.2014-0115
Chen J, Zhang W, Kelk P, Backman LJ, Danielson P (2017) Substance P and patterned silk biomaterial stimulate periodontal ligament stem cells to form corneal stroma in a bioengineered three-dimensional model. Stem Cell Res Ther 8:260. https://doi.org/10.1186/s13287-017-0715-y
Lan X, Sun Z, Chu C, Boltze J, Li S (2019) Dental pulp stem cells: an attractive alternative for cell therapy in ischemic stroke. Front Neurol 10:824. https://doi.org/10.3389/fneur.2019.00824
Karamichos D, Rich CB, Hutcheon AE, Ren R, Saitta B, Trinkaus-Randall V, Zieske JD (2011) Self-assembled matrix by umbilical cord stem cells. J Funct Biomater 2:213–229. https://doi.org/10.3390/jfb2030213
Coulson-Thomas VJ, Caterson B, Kao WW (2013) Transplantation of human umbilical mesenchymal stem cells cures the corneal defects of mucopolysaccharidosis VII mice. Stem Cells 31:2116–2126. https://doi.org/10.1002/stem.1481
Tsuji W, Rubin JP, Marra KG (2014) Adipose-derived stem cells: Implications in tissue regeneration. World J Stem Cells 6:312–321. https://doi.org/10.4252/wjsc.v6.i3.312
Ma XY, Bao HJ, Cui L, Zou J (2013) The graft of autologous adipose-derived stem cells in the corneal stromal after mechanic damage. PLoS One 8:e76103. https://doi.org/10.1371/journal.pone.0076103
Du Y, Roh DS, Funderburgh ML, Mann MM, Marra KG, Rubin JP, Li X, Funderburgh JL (2010) Adipose-derived stem cells differentiate to keratocytes in vitro. Mol Vis 16:2680–2689
Zhang S, Espandar L, Imhof KM, Bunnell BA (2013) Differentiation of human adipose-derived stem cells along the keratocyte lineage in vitro. J Clin Exp Ophthalmol 4. https://doi.org/10.4172/2155-9570.1000270
Zeppieri M, Salvetat ML, Beltrami A, Cesselli D, Russo R, Alcalde I, Merayo-Lloves J, Brusini P, Parodi PC (2017) Adipose derived stem cells for corneal wound healing after laser induced corneal lesions in mice. J Clin Med 6. https://doi.org/10.3390/jcm6120115
Alio del Barrio JL, Chiesa M, Garagorri N, Garcia-Urquia N, Fernandez-Delgado J, Bataille L, Rodriguez A, Arnalich-Montiel F, Zarnowski T, Alvarez de Toledo JP, Alio JL, De Miguel MP (2015) Acellular human corneal matrix sheets seeded with human adipose-derived mesenchymal stem cells integrate functionally in an experimental animal model. Exp Eye Res 132:91–100. https://doi.org/10.1016/j.exer.2015.01.020
Alio Del Barrio JL, El Zarif M, Azaar A, Makdissy N, Khalil C, Harb W, El Achkar I, Jawad ZA, de Miguel MP, Alio JL (2018) Corneal stroma enhancement with decellularized stromal laminas with or without stem cell recellularization for advanced keratoconus. Am J Ophthalmol 186:47–58. https://doi.org/10.1016/j.ajo.2017.10.026
Alio JL, Alio Del Barrio JL, El Zarif M, Azaar A, Makdissy N, Khalil C, Harb W, El Achkar I, Jawad ZA, De Miguel MP (2019) Regenerative surgery of the corneal stroma for advanced keratoconus: 1-year outcomes. Am J Ophthalmol 203:53–68. https://doi.org/10.1016/j.ajo.2019.02.009
El Zarif M, K AJ, Alio Del Barrio JL, Z AJ, Palazon-Bru A, de Miguel MP, Saba P, Makdissy N, Alio JL (2020) Corneal stroma cell density evolution in keratoconus corneas following the implantation of adipose mesenchymal stem cells and corneal laminas: an in vivo confocal microscopy study. Invest Ophthalmol Vis Sci 61: 22. https://doi.org/10.1167/iovs.61.4.22
El Zarif M, Alio JL, Alio Del Barrio JL, Abdul Jawad K, Palazon-Bru A, Abdul Jawad Z, De Miguel MP, Makdissy N (2021) Corneal stromal regeneration therapy for advanced keratoconus: long-term outcomes at 3 years. Cornea 40:741–754. https://doi.org/10.1097/ICO.0000000000002646
Alio Del Barrio JL, Arnalich-Montiel F, De Miguel MP, El Zarif M, Alio JL (2021) Corneal stroma regeneration: preclinical studies. Exp Eye Res 202:108314. https://doi.org/10.1016/j.exer.2020.108314
Liu H, Zhang J, Liu CY, Wang IJ, Sieber M, Chang J, Jester JV, Kao WW (2010) Cell therapy of congenital corneal diseases with umbilical mesenchymal stem cells: lumican null mice. PLoS One 5:e10707. https://doi.org/10.1371/journal.pone.0010707
Liu H, Zhang J, Liu CY, Hayashi Y, Kao WW (2012) Bone marrow mesenchymal stem cells can differentiate and assume corneal keratocyte phenotype. J Cell Mol Med 16:1114–1124. https://doi.org/10.1111/j.1582-4934.2011.01418.x
Park SH, Kim KW, Chun YS, Kim JC (2012) Human mesenchymal stem cells differentiate into keratocyte-like cells in keratocyte-conditioned medium. Exp Eye Res 101:16–26. https://doi.org/10.1016/j.exer.2012.05.009
Trosan P, Javorkova E, Zajicova A, Hajkova M, Hermankova B, Kossl J, Krulova M, Holan V (2016) The supportive role of insulin-like growth factor-I in the differentiation of murine mesenchymal stem cells into corneal-like cells. Stem Cells Dev 25:874–881. https://doi.org/10.1089/scd.2016.0030
Yamanaka S (2020) Pluripotent stem cell-based cell therapy-promise and challenges. Cell Stem Cell 27:523–531. https://doi.org/10.1016/j.stem.2020.09.014
Joseph R, Srivastava OP, Pfister RR (2016) Modeling keratoconus using induced pluripotent stem cells. Invest Ophthalmol Vis Sci 57:3685–3697. https://doi.org/10.1167/iovs.16-19105
Naylor RW, McGhee CN, Cowan CA, Davidson AJ, Holm TM, Sherwin T (2016) Derivation of corneal keratocyte-like cells from human induced pluripotent stem cells. PLoS One 11:e0165464. https://doi.org/10.1371/journal.pone.0165464
Foster JW, Wahlin K, Adams SM, Birk DE, Zack DJ, Chakravarti S (2017) Cornea organoids from human induced pluripotent stem cells. Sci Rep 7:41286. https://doi.org/10.1038/srep41286
Foster JW, Wahlin KJ, Chakravarti S (2020) A guide to the development of human corneaorganoids from induced pluripotent stem cells in culture. Methods Mol Biol 2145:51–58. https://doi.org/10.1007/978-1-0716-0599-8_5
Eveleth DD (2013) Cell-based therapies for ocular disease. J Ocul Pharmacol Ther 29:844–854. https://doi.org/10.1089/jop.2013.0028
Conlon KC, Miljkovic MD, Waldmann TA (2019) Cytokines in the treatment of cancer. J Interferon Cytokine Res 39:6–21. https://doi.org/10.1089/jir.2018.0019
Okada AA (1998) Cytokine therapy in eye disease. Arch Ophthalmol 116:1514–1516. https://doi.org/10.1001/archopht.116.11.1514
Tidu A, Schanne-Klein MC, Borderie VM (2020) Development, structure, and bioengineering of the human corneal stroma: a review of collagen-based implants. Exp Eye Res 200:108256. https://doi.org/10.1016/j.exer.2020.108256
Li SF, Han Y, Wang F, Su Y (2020) Progress in exosomes and their potential use in ocular diseases. Int J Ophthalmol 13:1493–1498. https://doi.org/10.18240/ijo.2020.09.23
Acknowledgements
The authors would also like to thank Dr Arkasubhra Ghosh, Dr P Narendra, and Dr K Bhujang Shetty for their administrative support needed for this work.
Funding
This study was funded by Narayana Nethralaya Foundation, India, and Velux Stiftung, Switzerland (Grant NO. 1695).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shetty, R., Mahendran, K., Joshi, P.D. et al. Corneal stromal regeneration—keratoconus cell therapy: a review. Graefes Arch Clin Exp Ophthalmol 261, 3051–3065 (2023). https://doi.org/10.1007/s00417-023-06064-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-023-06064-7