Abstract
Keratoconus is a progressive, ectatic and blinding disorder of the cornea, characterized by thinning of corneal stroma. As a highly prevalent among adolescents, keratoconus has been a leading indication for corneal transplantation worldwide. However, the severe shortage of donor corneas is a global issue, and the traditional corneal transplantation surgeries may superinduce multiple complications, necessitating efforts to develop more effective strategies for keratoconus treatment. In this review, we summarized several strategies to promote corneal stromal regeneration or improve corneal stromal thickness, including cell-based therapies, biosynthetic alternatives for inducing corneal regeneration, minimally invasive intrastromal implantation and bioengineered tissues for implantation. These strategies provided more accessible but safer alternatives from various perspectives for keratoconus treatment, paving the way for arresting the keratoconus progression in its earlier stage. For the treatments of corneal ectatic diseases beyond keratoconus, these approaches will provide important references and widen the therapy options in a donor tissue-independent manner.
Similar content being viewed by others
Background
Keratoconus is a progressive corneal ectatic disorder characterized by thinning of corneal stroma and asymmetrical conical protrusion of the cornea, which can lead to visual impairment or even blindness [1,2,3]. Keratoconus is one of the leading indications for corneal transplantation surgery worldwide [4, 5], with an incidence of 1/2000 in the general population and even higher among young adults [2, 6]. Keratoconus is the result of complex genetic and environmental interactions [7,8,9]. The most severe stage of keratoconus manifests with excessive ectasia, scarring and thinning stroma, which significantly impairs the vision, and the only option left for patients is corneal transplantation [1]. However, the severe shortage of the donor corneas available for transplant represents a global burden of blindness, with one cornea available for every 70 recipients in waiting [10]. Besides, traditional corneal transplantation surgeries can cause various complications, such as the severed corneal nerve plexus, dry eye, glaucoma and tissue rejection. Due to the immune rejection and chronic corneal allograft dysfunction, the poor long-term graft survival rate after keratoplasty usually brings a huge burden on patients. For these reasons, intense research effort has focused on corneal stromal regeneration to increase the corneal thickness of patients with keratoconus, and multiple therapy paradigms have been explored as alternative treatment modalities to preserve and improve the vision [11,12,13,14]. In this review, the strategies for corneal stromal regeneration are summarized, highlighting potential approaches for keratoconus treatment.
Strategies for corneal stromal regeneration
Cell therapy for keratoconus treatment
Currently, corneal collagen cross-linking and corneal transplant remain the most preferred or even the only option for keratoconus treatment. However, neither of these approaches can fundamentally solve the underlying issue of the disease. Approximately 80–85% of the corneal thickness is composed of the corneal stroma, in which collagen fibrils and extracellular matrix are tightly arranged [15, 16]. Keratocyte loss and excessive degradation of collagen fiber by matrix metalloproteinases are the culprit of keratoconus pathogenesis [17, 18]. Hence, replacing or reviving the corneal stromal cells might be an ideal and direct approach; therefore, cell-based therapies for corneal stromal regeneration during keratoconus treatment have emerged and gained great concern.
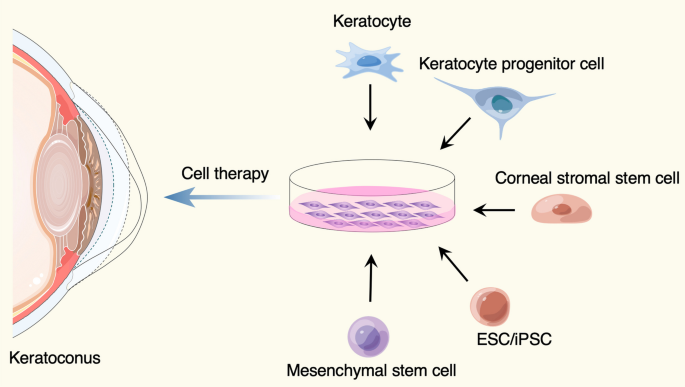
To date, various ideas and choices for cell therapy of keratoconus were developed (Fig. 1, Table 1). Keratocytes in the cornea are derived from neural crest cells. The number of keratocytes are limited in vivo, but they can be cultured in vitro and supplied as reliable cell source for intrastromal injection [19, 20]. Besides, keratocyte progenitor cells, the committed stem cell populations that maintain capacity to self-renewal and differentiation, are thought to be a potential option for keratoconus treatment. The transplantation of healthy keratocyte progenitor cells into keratoconus corneas would provide a novel treatment modality that may slow the progression of keratoconus [21]. Moreover, the corneal stromal stem cells, a rare cell population resident in the peripheral cornea and limbus, can be isolated by specific surface markers from limbal stromal tissues [22,23,24,25]. Du et al. injected the human corneal stromal stem cells into mice corneas and did not observe elicit immune rejection over an extended period of time, suggesting an opportunity to develop cell-based therapies for corneal stromal diseases [26].
Cell sources used for keratoconus treatment. The figure was prepared by our group, and some of the elements in the diagram were provided by Figdraw (http://www.figdraw.com)
However, several cell types mentioned above are still dependent on the corneal tissues, and the shortage of donor corneal tissues and the limited numbers of the particular cell populations is a significant challenge. The corneal stromal cells were found to have properties similar to other mesenchymal stem cells from various tissues [24, 27, 28], including adipose tissue [29,30,31], hematopoietic stem cells [32], dental pulp [33, 34] and umbilical cord blood [35], which have been demonstrated to be used for keratoconus cell therapy [11]. For example, implantation of autologous adipose tissue-derived stem cells (ADSCs) into corneal stroma has been successfully tested for the treatment of keratoconus [30, 31, 36, 37]. In addition, embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs) also provide sufficient cell sources that could be differentiated to keratocytes required for keratoconus therapy [38].
Biosynthetic alternatives for inducing corneal regeneration
Replacement of the damaged tissue with corneal transplants is widely accepted treatment for corneal blindness. Over ten years ago, Per Fagerholm et al. developed a kind of recombinant human collagen type III (RHCIII), which has undergone synthesized in yeast, chemically cross-linked, and molded into a biosynthetic cornea mimic [39]. They conducted a phase 1 clinical study in which the biosynthetic cornea mimics were implanted to replace the distorted corneas of 10 patients with keratoconus or central scar. Strikingly, corneal re-epithelialization occurred in all patients, and nerve regeneration and touch sensitivity were also restored, demonstrating the property of the biosynthetic mimics in facilitating endogenous tissue regeneration. After then, further optimization of the biosynthetic corneal implants was done [40, 41]. More significantly, Christopher D. McTiernan et al. developed a regeneration-stimulating liquid corneal replacement in a syringe that gels in situ, LiQD cornea, that comprises short collagen-like peptides, polyethylene glycol and fibrinogen [42]. The self-assembling synthetic collagen analog, as a low-cost and immune-compatible alternative, offering a safe and effective option to help address the current donor cornea shortage. Detailed information of these approaches is listed in Table 1.
Mechanical methods to improve corneal stomal thickness
Minimally invasive intrastromal implantation
Beside the strategy of corneal stromal cell replacement, restoring the physical properties of the corneal stroma cannot be ignored during keratoconus treatment [14]. Substantial biomechanical imbalance and weakening of the cornea can distinctly deteriorate the ocular surface homeostasis [43, 44]. As we know, eye-rubbing is one of the major risk factors for keratoconus progressive, which can induce distinct alterations in corneal biomechanics [45,46,47]. And mechanical stretch was a trigger for keratoconus development and biomechanics-enzymes axis played a pathogenic role in keratoconus, as identified in our study [48]. Therefore, strengthening the biomechanical properties of the cornea should be considered during keratoconus treatment.
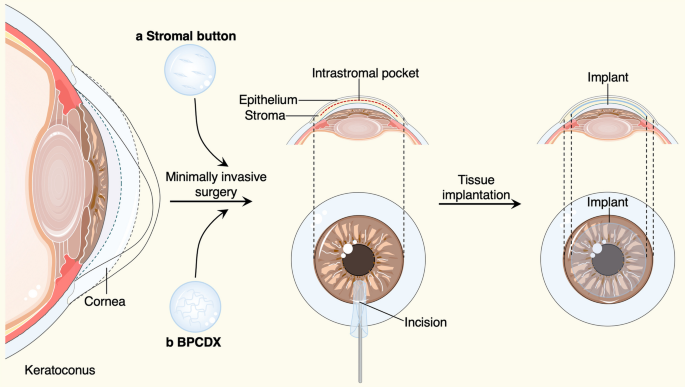
In recent years, corneal collagen cross-linking therapy, as a primary operative correction for progressive keratoconus, are used routinely to increase the biomechanical stability of the cornea. However, for keratoconus that has progressed to the most severe stage, corneal transplantation is the only option [1] (Table 2). Penetrating keratoplasty (PK) is a transplant procedure with full-thickness resection of the cornea, followed by grafting it with a full-thickness donor cornea, which was the treatment of choice for keratoconus until the late twentieth century [49,50,51]. When indicated, refinements in surgical approaches, like the deep anterior lamellar keratoplasty (DALK) [49,50,51] and anterior lamellar keratoplasty (ALK) [52], that were surgical procedures for removing part of the cornea. For instance, DALK involves replacement of the pathological corneal stroma down to the Descemet’s membrane but with the functional corneal endothelium retained, offers an effective alternative procedure that may lessen the risks including graft rejection and irregular astigmatism in PK. Despite DALK's success in restoring keratoconus patients' vision, there is still room for improvement regarding the operational complexity, restoring the physical properties of corneal stroma, preservation of the anterior corneal structure and nerve plexus, and suture-related complications. Therefore, suture-free implementation with smaller access cuts may be a preferred surgical option to arrest the progress of keratoconus, such as epikeratophakia (EP) [53, 54], Bowman layer (BL) transplantation [55, 56] and allogenic lenticule implantation [57,58,59,60]. Besides, our group have introduced a new effective procedure for the treatment of advanced keratoconus, named “femtosecond laser-assisted minimally invasive lamellar keratoplasty” (FL-MILK), in which partial thickness corneal stroma (stromal button) was implanted to the allogeneic corneal stroma through a small incision created by femtosecond laser (intrastromal pocket) [61] (as illustrated schematically in Fig. 2). Our study also indicated that FL-MILK can stabilize progressive KC in mild-to-moderate cases and advanced cases at 24-month follow-up with sustainable flattening effect of the anterior cornea curvature [62]. Indeed, while improving the stromal thickness, this minimally invasive surgical methods can maximally maintain the structural integrity and physical properties of the cornea, providing a feasible option for keratoconus treatment that should be put on the agenda.
Minimally invasive surgical methods and bioengineered grafts for keratoconus treatment. An intrastromal pocket with a small incision were created by femtosecond laser, the human stromal button (a) or bioengineered BPCDX graft (b) were gently inserted into the intrastromal pocket to increase the corneal thickness. The figure was prepared by our group
Bioengineered corneal tissues for implantation
For the keratoplasty to treat keratoconus, several materials can be used as biomedical implants. The natural cornea has particular advantage in mechanical properties and structures, while the severe shortage of donor corneas presents a global concern. Hence, intense research efforts have focused on effective alternatives to conventional corneal grafts. May Grifith et al. successfully multilayered corneal equivalents constructed from immortalized cell lines [63]. Per Fagerholm et al. conducted a phase 1 clinical study in which biosynthetic mimics of corneal extracellular matrix were implanted to induce corneal regeneration [39]. Our group have developed a protective decellularization strategy for the preparation of decellularized porcine cornea (DPC), which achieved equivalent levels in numerous properties compared with that of human cornea grafts [64]. All these studies offered prospects for visual rehabilitation of corneal blindness. Even more to the point, Mehrdad Rafat and colleagues have described a cell-free engineered corneal tissue, which was derived from purified type I porcine collagen with dual chemical and photochemical cross-linking applied, termed the bioengineered porcine construct, double cross-linked (BPCDX) [65] (Fig. 2). The authors extracted and purified collagen from a by-product of the food industry, the porcine skin, providing an abundant yet sustainable and cost-effective supply of raw materials for implants. At the same time, likewise, the authors insert the implant within the corneal stroma through a minimally invasive procedure. Notably, after 2 years of follow-up, no adverse event was reported, all participants' vision improved to the same degree as with a standard donor tissue transplant. The strategy proposed by this work in which accessible bioengineered corneal tissues and minimally invasive surgical methods were elaborately combined, would be an attractive option for treatment of advanced keratoconus, especially in resource-limited settings. Details of the approaches mentioned in this part are listed in Table 2.
Discussion
In this review, we summarized several approaches to promote corneal stromal regeneration or improve corneal stromal thickness, including cell-based therapies, biosynthetic alternatives for inducing corneal regeneration, minimally invasive intrastromal implantation and bioengineered tissues for implantation. Among these, a series of mechanical methods to improve corneal stomal thickness have been applied in clinical treatment of keratoconus. For instance, historically, PK has been the gold standard approach for the surgical treatment of advanced keratoconus with its good visual outcomes [50, 51]. However, DALK is increasingly becoming the preferred primary surgical option in contemporary practice owing to its reduced rejection and astigmatism in PK complications. But the complexity of operation and risks of suture-related complications in DALK complications cannot be ignored, which prompted the occurrence of minimally invasive surgical methods [49,50,51]. For example, FL-MILK can maximally maintain the structural integrity and physical properties of the cornea while improving the stromal thickness, and its more precise and quick recovery might make it an effective alternative for the treatment of advanced keratoconus [61]. Besides, combined more accessible bioengineered corneal tissues and minimally invasive methods would be an attractive option for keratoconus treatment. Indeed, longer follow-up period and more cases are needed for several new improving approaches.
In addition, the severe shortage of donor tissue impeded the treatment of keratoconus through corneal transplant surgery, especially in resource-limited settings. Therefore, explorations in developing strategies to promote corneal stromal regeneration has never stopped. The ideal cell-based therapy is expected to replace or revive the diseased keratocyte cells by inducing regeneration or by exogenous transplantation of keratocyte-committed cells. Here we listed the cell sources, stage of research, advantages and limitations for various cell-based therapeutic methods. Among these, implantation of autologous ADSCs into corneal stroma has been successfully tested for the treatment of keratoconus in clinical trials [30, 31, 36, 37], with its abundant and easily accessible cell source. Besides, biosynthetic alternatives for inducing corneal regeneration, including RHCIII [39] and LiQD cornea [42], providing low-cost and immune-compatible alternatives to help address the donor cornea shortage.
Conclusions
Collectively, this review highlighted the advances in therapeutic strategies that can promote corneal stromal regeneration or improve corneal stromal thickness for keratoconus treatment, providing important reference and foundations for developing potential interventions. These approaches have brought hopes for keratoconus therapy with more safe and accessible alternative options, reducing the surgical complication and burden of limited donor corneas globally. Generally, DALK has become an alternative to PK, while minimally invasive surgery will become a major trend in the future treatment of keratoconus. And keratocyte regeneration therapies will also usher in a new era, especially for the ADSCs-based treatment, though the potential of several novel therapies for achieving effective stromal regeneration need further explorations. Certainly, further studies should be conducted to confirm the optimal therapeutic methods and conditions for keratoconus intervention, and novel approaches would be developed to control and arrest the progression of keratoconus in its much earlier stage, which might hopefully postpone or prevent an invasive corneal surgery. For keratoconus treatment, the light is shining brighter on its way.
Availability of data and materials
All datasets used in this study are available from the corresponding author on reasonable request.
Abbreviations
- ADSCs:
-
Adipose tissue-derived stem cells
- ESCs:
-
Embryonic stem cells
- iPSCs:
-
Induced pluripotent stem cells
- PK:
-
Penetrating keratoplasty
- DALK:
-
Deep anterior lamellar keratoplasty
- ALK:
-
Anterior lamellar keratoplasty
- EP:
-
Epikeratophakia
- BL:
-
Bowman layer
- FL-MILK:
-
Femtosecond laser-assisted minimally invasive lamellar keratoplasty
- BPCDX:
-
Bioengineered porcine construct, double cross-linked
- RHCIII:
-
Recombinant human collagen type III
References
Gomes JA, Tan D, Rapuano CJ, Belin MW, Ambrosio R Jr, Guell JL, Malecaze F, Nishida K, Sangwan VS, Group of Panelists for the Global Delphi Panel of K, et al. Global consensus on keratoconus and ectatic diseases. Cornea. 2015;34(4):359–69.
Kymes SM, Walline JJ, Zadnik K, Sterling J, Gordon MO. Collaborative longitudinal evaluation of keratoconus study g: changes in the quality-of-life of people with keratoconus. Am J Ophthalmol. 2008;145(4):611–7.
Nichols JJ, Steger-May K, Edrington TB, Zadnik K. Group Cs: the relation between disease asymmetry and severity in keratoconus. Br J Ophthalmol. 2004;88(6):788–91.
Park CY, Lee JK, Gore PK, Lim CY, Chuck RS. Keratoplasty in the United States: a 10-year review from 2005 through 2014. Ophthalmology. 2015;122(12):2432–42.
Gao H, Huang T, Pan Z, Wu J, Xu J, Hong J, Chen W, Wu H, Kang Q, Zhu L, et al. Survey report on keratoplasty in China: a 5-year review from 2014 to 2018. PLoS ONE. 2020;15(10): e0239939.
Jian W, Shen Y, Chen Y, Tian M, Zhou X. Ocular dimensions of the Chinese adolescents with keratoconus. BMC Ophthalmol. 2018;18(1):43.
Rabinowitz YS. Keratoconus. Surv Ophthalmol. 1998;42(4):297–319.
Davidson AE, Hayes S, Hardcastle AJ, Tuft SJ. The pathogenesis of keratoconus. Eye (Lond). 2014;28(2):189–95.
Hao XD, Chen XN, Zhang YY, Chen P, Wei C, Shi WY, Gao H. Multi-level consistent changes of the ECM pathway identified in a typical keratoconus twin’s family by multi-omics analysis. Orphanet J Rare Dis. 2020;15(1):227.
Gain P, Jullienne R, He Z, Aldossary M, Acquart S, Cognasse F, Thuret G. Global survey of corneal transplantation and eye banking. JAMA Ophthalmol. 2016;134(2):167–73.
Shetty R, Mahendran K, Joshi PD, Jeyabalan N, Jayadev C, Das D. Corneal stromal regeneration-keratoconus cell therapy: a review. Graefes Arch Clin Exp Ophthalmol. 2023.
Lagali N. Corneal stromal regeneration: current status and future therapeutic potential. Curr Eye Res. 2020;45(3):278–90.
El Zarif M, Alio JL, Alio Del Barrio JL, De Miguel MP, Abdul Jawad K, Makdissy N. Corneal stromal regeneration: a review of human clinical studies in keratoconus treatment. Front Med (Lausanne). 2021;8: 650724.
Brunette I, Roberts CJ, Vidal F, Harissi-Dagher M, Lachaine J, Sheardown H, Durr GM, Proulx S, Griffith M. Alternatives to eye bank native tissue for corneal stromal replacement. Prog Retin Eye Res. 2017;59:97–130.
Matthyssen S, Van den Bogerd B, Dhubhghaill SN, Koppen C, Zakaria N. Corneal regeneration: a review of stromal replacements. Acta Biomater. 2018;69:31–41.
Song P, Wang S, Zhang P, Sui W, Zhang Y, Liu T, Gao H. The superficial stromal scar formation mechanism in keratoconus: a study using laser scanning in vivo confocal microscopy. Biomed Res Int. 2016;2016:7092938.
Fini ME, Yue BY, Sugar J. Collagenolytic/gelatinolytic metalloproteinases in normal and keratoconus corneas. Curr Eye Res. 1992;11(9):849–62.
Kao WW, Vergnes JP, Ebert J, Sundar-Raj CV, Brown SI. Increased collagenase and gelatinase activities in keratoconus. Biochem Biophys Res Commun. 1982;107(3):929–36.
Jester JV, Jin HC. Modulation of cultured corneal keratocyte phenotype by growth factors/cytokines control in vitro contractility and extracellular matrix contraction. Exp Eye Res. 2003;77(5):581–92.
Yam GHF, Fuest M, Yusoff NZBM, Goh TW, Bandeira F, Setiawan M, Seah XY, Lwin NC, Stanzel TP, Ong HS, et al. Safety and feasibility of intrastromal injection of cultivated human corneal stromal keratocytes as cell-based therapy for corneal opacities. Invest Ophth Vis Sci. 2018;59(8):3340–54.
Patel DV, McKelvie J, Sherwin T, McGhee C. Keratocyte progenitor cell transplantation: a novel therapeutic strategy for corneal disease. Med Hypotheses. 2013;80(2):122–4.
Nagymihaly RM, Moe MC, Petrovski G. Isolation and culture of corneal stromal stem cells. Methods Mol Biol. 2020;2145:1–15.
Kureshi AK, Funderburgh JL, Daniels JT. Human corneal stromal stem cells exhibit survival capacity following isolation from stored organ-culture corneas. Invest Ophthalmol Vis Sci. 2014;55(11):7583–8.
Pinnamaneni N, Funderburgh JL. Concise review: Stem cells in the corneal stroma. Stem Cells. 2012;30(6):1059–63.
Basu S, Hertsenberg AJ, Funderburgh ML, Burrow MK, Mann MM, Du Y, Lathrop KL, Syed-Picard FN, Adams SM, Birk DE, et al. Human limbal biopsy-derived stromal stem cells prevent corneal scarring. Sci Transl Med. 2014;6(266):266–172.
Du Y, Carlson EC, Funderburgh ML, Birk DE, Pearlman E, Guo N, Kao WW, Funderburgh JL. Stem cell therapy restores transparency to defective murine corneas. Stem Cells. 2009;27(7):1635–42.
Vereb Z, Poliska S, Albert R, Olstad OK, Boratko A, Csortos C, Moe MC, Facsko A, Petrovski G. Role of human corneal stroma-derived mesenchymal-like stem cells in corneal immunity and wound healing. Sci Rep. 2016;6:26227.
Branch MJ, Hashmani K, Dhillon P, Jones DR, Dua HS, Hopkinson A. Mesenchymal stem cells in the human corneal limbal stroma. Invest Ophthalmol Vis Sci. 2012;53(9):5109–16.
El Zarif M, Alio JL, Alio Del Barrio JL, Abdul Jawad K, Palazon-Bru A, Abdul Jawad Z, De Miguel MP, Makdissy N. Corneal stromal regeneration therapy for advanced keratoconus: long-term outcomes at 3 years. Cornea. 2021;40(6):741–54.
Alio Del Barrio JL, El Zarif M, de Miguel MP, Azaar A, Makdissy N, Harb W, El Achkar I, Arnalich-Montiel F, Alio JL. Cellular therapy with human autologous adipose-derived adult stem cells for advanced keratoconus. Cornea. 2017;36(8):952–60.
Donthineni PR, Bagga B, Singh V, Shukla S. Cellular therapy with human autologous adipose-derived adult stem cells for advanced keratoconus. Cornea. 2017;36(12):e36–7.
Liu H, Zhang J, Liu CY, Hayashi Y, Kao WW. Bone marrow mesenchymal stem cells can differentiate and assume corneal keratocyte phenotype. J Cell Mol Med. 2012;16(5):1114–24.
Mansoor H, Ong HS, Riau AK, Stanzel TP, Mehta JS, Yam GH. Current trends and future perspective of mesenchymal stem cells and exosomes in corneal diseases. Int J Mol Sci 2019;20(12).
Syed-Picard FN, Du Y, Lathrop KL, Mann MM, Funderburgh ML, Funderburgh JL. Dental pulp stem cells: a new cellular resource for corneal stromal regeneration. Stem Cells Transl Med. 2015;4(3):276–85.
Liu H, Zhang J, Liu CY, Wang IJ, Sieber M, Chang J, Jester JV, Kao WW. Cell therapy of congenital corneal diseases with umbilical mesenchymal stem cells: lumican null mice. PLoS ONE. 2010;5(5): e10707.
Arnalich-Montiel F, Pastor S, Blazquez-Martinez A, Fernandez-Delgado J, Nistal M, Alio JL, De Miguel MP. Adipose-derived stem cells are a source for cell therapy of the corneal stroma. Stem Cells. 2008;26(2):570–9.
Ramin S, Abbasi A, Ahadi M, Moallemi Rad L, Kobarfad F. Assessment of the effects of intrastromal injection of adipose-derived stem cells in keratoconus patients. Int J Ophthalmol. 2023;16(6):863–70.
Joseph R, Srivastava OP, Pfister RR. Modeling keratoconus using induced pluripotent stem cells. Invest Ophthalmol Vis Sci. 2016;57(8):3685–97.
Fagerholm P, Lagali NS, Merrett K, Jackson WB, Munger R, Liu Y, Polarek JW, Soderqvist M, Griffith M. A biosynthetic alternative to human donor tissue for inducing corneal regeneration: 24-month follow-up of a phase 1 clinical study. Sci Transl Med. 2010;2(46):46–61.
Fagerholm P, Lagali NS, Ong JA, Merrett K, Jackson WB, Polarek JW, Suuronen EJ, Liu Y, Brunette I, Griffith M. Stable corneal regeneration four years after implantation of a cell-free recombinant human collagen scaffold. Biomaterials. 2014;35(8):2420–7.
Jangamreddy JR, Haagdorens MKC, Islam MM, Lewis P, Samanta A, Fagerholm P, Liszka A, Ljunggren MK, Buznyk O, Alarcon EI, et al. Short peptide analogs as alternatives to collagen in pro-regenerative corneal implants. Acta Biomater. 2018;69:120–30.
McTiernan CD, Simpson FC, Haagdorens M, Samarawickrama C, Hunter D, Buznyk O, Fagerholm P, Ljunggren MK, Lewis P, Pintelon I et al. LiQD cornea: pro-regeneration collagen mimetics as patches and alternatives to corneal transplantation. Sci Adv. 2020;6(25).
Vinciguerra R, Herber R, Wang Y, Zhang F, Zhou X, Bai J, Yu K, Chen S, Fang X, Raiskup F, et al. Corneal biomechanics differences between Chinese and Caucasian healthy subjects. Front Med (Lausanne). 2022;9: 834663.
Zhang X, Ding L, Sun L, Huang Y, Han T, Qian Y, Zhou X. Prognostic nomograms predicting risk of keratoconus in very asymmetric ectasia: combined corneal tomographic and biomechanical assessments. Front Bioeng Biotechnol. 2022;10: 839545.
Sahebjada S, Al-Mahrouqi HH, Moshegov S, Panchatcharam SM, Chan E, Daniell M, Baird PN. Eye rubbing in the aetiology of keratoconus: a systematic review and meta-analysis. Graefes Arch Clin Exp Ophthalmol. 2021;259(8):2057–67.
Bawazeer AM, Hodge WG, Lorimer B. Atopy and keratoconus: a multivariate analysis. Br J Ophthalmol. 2000;84(8):834–6.
Yang KL, Xu LY, Fan Q, Ren SW: Association between corneal stiffness parameter at the first applanation and keratoconus severity. J Ophthalmol. 2020;2020.
Dou S, Wang Q, Zhang B, Wei C, Wang H, Liu T, Duan H, Jiang H, Liu M, Qi X, et al. Single-cell atlas of keratoconus corneas revealed aberrant transcriptional signatures and implicated mechanical stretch as a trigger for keratoconus pathogenesis. Cell Discov. 2022;8(1):66.
Borderie VM, Sandali O, Bullet J, Gaujoux T, Touzeau O, Laroche L. Long-term results of deep anterior lamellar versus penetrating keratoplasty. Ophthalmology. 2012;119(2):249–55.
Yoshida J, Toyono T, Shirakawa R, Miyai T, Usui T. Risk factors and evaluation of keratoconus progression after penetrating keratoplasty with anterior segment optical coherence tomography. Sci Rep. 2020;10(1):18594.
Feizi S, Javadi MA, Karimian F, Bayat K, Bineshfar N, Esfandiari H. Penetrating keratoplasty versus deep anterior lamellar keratoplasty for advanced stage of keratoconus. Am J Ophthalmol. 2023;248:107–15.
Patil M, Mehta JS. Lamellar keratoplasty for advanced keratoconus. Asia Pac J Ophthalmol (Phila). 2020;9(6):580–8.
Krumeich JH, Daniel J, Knulle A. Live-epikeratophakia for keratoconus. J Cataract Refract Surg. 1998;24(4):456–63.
Krumeich JH, Daniel J. Live epikeratophakia and deep lamellar keratoplasty for I-III stage-specific surgical treatment of keratoconus. Klin Monbl Augenheilkd. 1997;211(2):94–100.
Dragnea DC, Birbal RS, Ham L, Dapena I, Oellerich S, van Dijk K, Melles GRJ. Bowman layer transplantation in the treatment of keratoconus. Eye Vis (Lond). 2018;5:24.
van der Star L, van Dijk K, Vasiliauskaite I, Dapena I, Oellerich S, Melles GRJ. Long-term outcomes of bowman layer inlay transplantation for the treatment of progressive keratoconus. Cornea. 2022;41(9):1150–7.
Li M, Zhao F, Li M, Knorz MC, Zhou X. Treatment of corneal ectasia by implantation of an allogenic corneal lenticule. J Refract Surg. 2018;34(5):347–50.
Ganesh S, Brar S. Femtosecond intrastromal lenticular implantation combined with accelerated collagen cross-linking for the treatment of keratoconus-initial clinical result in 6 eyes. Cornea. 2015;34(10):1331–9.
Jin H, He M, Liu H, Zhong X, Wu J, Liu L, Ding H, Zhang C, Zhong X. Small-incision femtosecond laser-assisted intracorneal concave lenticule implantation in patients with keratoconus. Cornea. 2019;38(4):446–53.
Wei Q, Ding H, Nie K, Jin H, Zhong T, Yu H, Yang Z, Hu S, He L, Zhong X. Long-term clinical outcomes of small-incision femtosecond laser-assisted intracorneal concave lenticule implantation in patients with keratoconus. J Ophthalmol. 2022;2022:9774448.
Gao H, Liu M, Li N, Chen T, Qi X, Xie L, Shi W. Femtosecond laser-assisted minimally invasive lamellar keratoplasty for the treatment of advanced keratoconus. Clin Exp Ophthalmol. 2022;50(3):294–302.
Li N, Liu M, Tian G, Chen T, Lin Y, Qi X, Shi W, Gao H. Effects of femtosecond laser-assisted minimally invasive lamellar keratoplasty (FL-MILK) on mild-to-moderate and advanced keratoconus. Graefes Arch Clin Exp Ophthalmol. 2023;
Griffith M, Osborne R, Munger R, Xiong X, Doillon CJ, Laycock NL, Hakim M, Song Y, Watsky MA. Functional human corneal equivalents constructed from cell lines. Science. 1999;286(5447):2169–72.
Shi W, Zhou Q, Gao H, Li S, Dong M, Wang T, Jia Y, Dong C, Wang X, Guo Z, et al. Protectively decellularized porcine cornea versus human donor cornea for lamellar transplantation. Adv Funct Mater. 2019;29(37).
Rafat M, Jabbarvand M, Sharma N, Xeroudaki M, Tabe S, Omrani R, Thangavelu M, Mukwaya A, Fagerholm P, Lennikov A, et al. Bioengineered corneal tissue for minimally invasive vision restoration in advanced keratoconus in two clinical cohorts. Nat Biotechnol. 2022;
Acknowledgements
We thank Tong Liu for constructive suggestions on this review. Some of the elements in the diagram were provided by Figdraw (http://www.figdraw.com)
Funding
This work was supported by the National Natural Science Foundation of China (82070923, 82101092, 82371032), Taishan Scholar Program (201812150, 202306390), Major Basic Research Project of Natural Science Foundation of Shandong Province (ZR2023ZD60) and the Academic Promotion Program and Innovation Project of Shandong First Medical University (2019RC009).
Author information
Authors and Affiliations
Contributions
H.G. conceptualized, acquired funding and supervised this study. S.D. drafted the manuscript. X.L. performed literature search and collection. W.S. provided advice and discussed the manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dou, S., Liu, X., Shi, W. et al. New dawn for keratoconus treatment: potential strategies for corneal stromal regeneration. Stem Cell Res Ther 14, 317 (2023). https://doi.org/10.1186/s13287-023-03548-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13287-023-03548-5