Abstract
Purpose
We have previously demonstrated that prolonged use of glaucoma medications was associated with a poor surgical outcome of ab interno trabeculotomy (µTLO). Given that almost all types of glaucoma eye drop either enhance the drainage through the uveoscleral pathway or reduce aqueous humor production, we hypothesized that prolonged use of these medications might cause disuse atrophy of the conventional pathway. In contrast, ripasudil increases the conventional outflow and eventually shows a favorable outcome of µTLO. This study aimed to evaluate the effect of ripasudil use on µTLO outcomes.
Method
The medical charts of 218 patients who underwent µTLO were analyzed retrospectively. We compared the 1-year outcome between ripasudil users versus nonusers by using propensity score matching. We set the covariates as age, sex, glaucoma types, preoperative intraocular pressure (IOP), the mean deviation values of visual field tests, the presence or absence of concomitant cataract surgery, trabecular meshwork incision range, the presence or absence of any glaucoma medication except ripasudil and duration of glaucoma medical therapy. Success was defined as a postoperative IOP between 5 and 21 mmHg, a ≥ 20% IOP reduction from baseline, and no additional glaucoma surgery at postoperative 1 year.
Result
Fifty-seven patients each were allocated to the ripasudil users or nonusers. The 1-year success rates were 74% in ripasudil users and 51% in nonusers (p = 0.01). Kaplan‒Meier survival curves also showed that the ripasudil users had a higher survival distribution (p = 0.01).
Conclusion
The patients who took ripasudil showed a favorable 1-year outcome of µTLO.
Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
Glaucoma treatment has dramatically developed both medically and surgically. Ripasudil hydrochloride hydrate (ripasudil), which is a Rho kinase inhibitor, has emerged as a drug with a new mechanism and has been used for clinical practice in Japan and South Korea [1]. Other main types of glaucoma medications available in Japan promote drainage into the uveoscleral pathway or decrease aqueous humor production. In contrast, ripasudil increases the conventional trabecular meshwork—Schlemm’s canal outflow—based on its Rho kinase inhibitory action [2]. Another study showed that ripasudil induced morphological changes in type VI collagen of the juxtacanalicular tissue [3].
From a surgical viewpoint, minimally/micro invasive glaucoma surgery (MIGS) has become applicable for treating mild to moderate glaucoma patients. MIGS is classified into two categories: Schlemm’s canal surgeries and filtration surgeries such as PreserFlo and Xen. The former type of MIGS incises the trabecular meshwork, the main aqueous humor resistance of the trabecular outflow pathway via an ab interno and ab externo approach. Ab interno Schlemm’s canal surgery [4], sometimes called trabeculotomy [5], goniotomy [6] or goniectomy [7], includes iStent, Trabectome, Kahook Dual Blade, TrabEx + , gonioscopy-assisted transluminal trabeculotomy, Hydrus Microstent, and viscocanalostomy [8]. In Japan, ab interno trabeculotomy using a “microhook” device developed by Tanito (µTLO) [9] has gained enormous popularity for two reasons. First, µTLO shows cost-effectiveness because the microhook is reusable after sterilization. Second, our recent multicenter study has shown that µTLO has a similar surgical outcome to Trabectome, the pioneer of MIGS [10].
On the other hand, our recent study revealed that the prolonged use of glaucoma medications had a negative impact on postoperative outcomes of µTLO [11]. We speculate that this may be attributable to disuse atrophy of the trabecular outflow (conventional) pathway in patients who took long-term glaucoma medications, given their mechanisms of action as mentioned above.
Taking the pharmacological action of ripasudil into consideration, it is reasonable to hypothesize that ripasudil, unlike other medications, may not cause disuse atrophy of the trabecular meshwork (Schlemm’s canal pathway), which could rather show a favorable surgical outcome of µTLO. The purpose of this study was to investigate the effect of preoperative ripasudil administration on µTLO surgical outcomes at 1 year.
Method
Subjects
The medical charts of all adult patients (≥ 20 years old) who underwent µTLO between February 2017 and April 2021 in Kobe University Hospital were reviewed retrospectively. Patients who had a history of glaucoma surgery, including laser surgery, were excluded. When both eyes were operated on, the first eye was selected. We thus analyzed 218 eyes of 218 patients in total.
Clinical characteristics
The information collected was as follows: age, sex, glaucoma types, intraocular pressure (IOP), glaucoma drug score, best-corrected decimal visual acuity (VA), the mean deviation values of Humphrey visual field tests (MD), corneal endothelial cell density (ECD), the presence or absence of any glaucoma medication at the time of surgery, the overall duration of glaucoma medical therapy, and whether antithrombotic drugs were used preoperatively.
The glaucoma drug score was counted as one point for each eye drop but two points for combined eye drops and oral administration of carbonic anhydrase inhibitors [10,11,12,13,14]. We also collected perioperative information about the presence or absence of concomitant cataract surgery and trabecular meshwork incision range (one or two quadrants). The detailed surgical technique of µTLO was described previously [11, 12, 14]. We analyzed IOP and glaucoma drug scores preoperatively and 1 week, 1, 3, 6, 9, and 12 months postoperatively and VA, MD, and ECD preoperatively. For eyes that required additional surgery within 1 year after the initial surgery, we imputed postoperative parameters using the last observation carried forward method. We counted the number of patients who had hyphema and transiently elevated IOP as early surgery-related complications. The presence of layered hyphema was regarded as hyphema in this study. The term “transiently elevated IOP” refers to postoperative IOP exceeding the preoperative value despite the use of the same glaucoma drugs as preoperatively [10, 11, 14]. After surgery, the choice of postoperative medications is based on each patient’s target IOP. Surgeons will resume appropriate drugs referring to their preoperative medications.
Data analysis
Surgical success was defined as meeting these three criteria, as follows: (1) IOP within 5–21 mmHg, (2) reduction in IOP by at least 20% from the preoperative IOP, and (3) no additional glaucoma surgery [10,11,12, 14]. Surgical failure was marked when additional glaucoma surgeries were conducted or the IOP was out of the above mentioned range on two consecutive time points after 1 month postoperatively, and the earlier point was defined as the date of failure. The distribution of surgical success between the ripasudil users and nonusers was compared using a log-rank test based on the Kaplan‒Meier survival curve. Ripasudil users were defined as individuals who took the drug at the time of surgery. We also compared the preoperative and postoperative parameters between the two groups by the Mann‒Whitney U test for continuous variables and the chi-square test or Fisher’s exact test for binary variables. A p-value < 0.05 was considered statistically significant. Statistical analysis was performed using MedCalc (version 20.015, MedCalc Software, Mariakerte, Belgium).
Propensity score matching analysis
When we compared the perioperative characteristics between the ripasudil users and nonusers, the raw data showed significant differences in the proportions of patients with steroid-induced glaucoma, the preoperative IOP, and the glaucoma drug score (Supplemental Table 1). Previous reports showed that steroid-induced glaucoma had a higher surgical success rate than primary open-angle glaucoma [15, 16]. Preoperative high IOP was a risk factor for surgical failure in Schlemm’s canal surgery [17,18,19,20]. Comparing patients from different backgrounds likely induces biases. To cope with this problem, we used a propensity score analysis. A propensity score was defined as the conditional probability of two groups given the observed covariates. The covariates used in building the propensity score were age, sex, glaucoma types, preoperative IOP, MD, the presence or absence of combined cataract surgery, incision range, the presence or absence of any glaucoma medications except ripasudil at the time of surgery, and overall duration of glaucoma medical therapy. We performed a one-to-one matching analysis between the two groups based on the estimated propensity score of each patient using a logistic regression model. A caliper width of 0.2 of the standard deviation of the propensity score was used for the one-to-one matching analysis [10].
Results
Table 1 shows the preoperative characteristics after propensity score matching between the ripasudil users and nonusers. After one-to-one matching, 57 patients each were allocated into the two groups. Propensity score matching eliminated the significant differences in the glaucoma types and preoperative IOP that existed prior to the matching. There was one eyedrop difference in the median glaucoma drop score between the ripasudil users and nonusers (median 5.0 vs. 4.0; p < 0.001).
The glaucoma medications used preoperatively in the two groups after matching adjustments are listed in Table 2. We classified the types of glaucoma medications according to the Japan Glaucoma Society Guidelines for Glaucoma [21]. Prostanoid receptor analogs were administered in 97% of the patients of both groups. The other three types of eyedrops (β-blockers, carbonic dehydrate inhibitors, and an α2 adrenergic agonist) followed the proportion of use in these patients. Few patients used the remaining three types (an α1 adrenergic antagonist, an ion-channel opener, and a parasympathomimetic). There was no significant difference in the proportion of each glaucoma eye drop except for ripasudil (p < 0.0001).
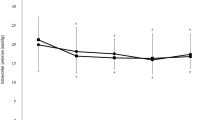
The time-course changes in the IOP and glaucoma drug scores in the two groups are shown in Fig. 1. Both groups demonstrated significantly decreased postoperative IOP and glaucoma drug scores compared to the preoperative values at each time point (p < 0.001). The median postoperative IOP in the ripasudil users was lower than that in the nonusers, but a statistically significant difference was not found at any postoperative time points. The glaucoma drug score was also not different between the two groups at any point.
Table 3 summarizes the surgical outcomes of early surgery-related complications and 1-year results. There was no difference in early surgery-related complications between the two groups. There was no significant difference in IOP at 1 year postoperatively between the ripasudil users and nonusers (median 16.0 vs. 18.0 mmHg, p = 0.09). The ripasudil users accounted for a significantly lower proportion of additional glaucoma surgeries (9% vs. 28%, p = 0.01). The success rate of the ripasudil users was 74%, while that of the nonusers was 51% at postoperative 1 year. There was a significant difference in the 1-year success rate between the two groups (p = 0.01).
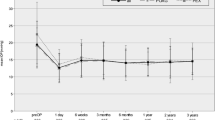
Figure 2 shows the Kaplan‒Meier survival curves in the two groups. The log-rank test revealed that the ripasudil users had a significantly higher survival distribution (p = 0.01).
Discussion
The present study elucidated that ripasudil users had significantly better IOP control 1 year after µTLO than nonusers. This is the first study to show that a certain type of preoperative eye drop influences the Schlemm’s canal surgery outcomes.
The glaucoma eye drops mainly used in Japan are classified into eight categories: prostanoid receptor analogs, β-blockers, carbonic anhydrase inhibitors, an α2 adrenergic agonist (brimonidine), an α1 adrenergic antagonist (bunazosin), an ion-channel opener (unoprostone isopropyl), a parasympathomimetic (pilocarpine), and a Rho kinase inhibitor (ripasudil). The prostanoid receptor analogs are subdivided into an EP2 receptor selective agonist (omidenepag isopropyl) and FP receptor agonists such as latanoprost, tafluprost, travoprost, and bimatoprost. As recommended by the 5th version of the Japan Glaucoma Society Guidelines for Glaucoma, prostanoid receptor analogs are deemed to be the first choice for glaucoma eye drops in Japan [21]. The second line is up to the preferences of physicians. Consequently, prostanoid receptor analogs were used in 97% of the patients in both the ripasudil users and nonusers in this study, while the proportion of other types of medication use was lower. Among these agents, ripasudil [2], an ion-channel opener [22], a parasympathomimetic [23], and an EP2 receptor selective agonist [24] are reported to increase the conventional outflow. In our study, no patients were administered an EP2 receptor selective agonist because this drug was approved in Japan quite recently (November 2018). The remaining three drugs are not prescribed as often in Japanese clinical practice due to their weak IOP-lowering effect. Therefore, the main glaucoma eye drops, except EP2 receptor selective agonist and ripasudil, may result in atrophy of the trabecular outflow pathway. It has been reported that Schlemm’s canal shrinks after trabeculectomy, a surgery for draining aqueous humor without using the physiological pathway [25].
We developed another hypothesis when we found an association between a long history of glaucoma medications and poor µTLO outcomes [11]. Eye drops contain various preservatives and additives, such as benzalkonium chloride (BAK), which might reduce the surgical success rate in µTLO. In fact, BAK is known to activate inflammatory mediators and induce apoptosis of trabecular meshwork cells in vivo [26]. Additionally, a similar mechanism has been reported in which BAK affects not only Schlemm’s canals but also subsequent collector channels [27]. Thus, we speculated that long-term exposure to BAK could contribute to reducing the surgical success rate in µTLO. However, ripasudil also contains BAK. Given the significant differences in the surgical outcomes between ripasudil users and nonusers, this scenario is unlikely.
While our study focused on the effect of µTLO in patients who did or did not receive preoperative ripasudil, it is possible that postoperative medications could have affected our results. Rho kinase inhibitors, including ripasudil, have been shown to inhibit fibroblast proliferation and reduce scarring after glaucoma surgery [28]. To investigate the potential impact of postoperative medications, we analyzed the postoperative use of ripasudil in our study population after matching (Supplemental Table 2) and compared the proportion of postoperative medications between the two groups (Supplemental Table 3). The presence or absence of postoperative medications did not significantly influence our results. Overall, the present study supports the use of preoperative ripasudil to enhance the efficacy of µTLO.
This study has several limitations. First, this is a retrospective single-center pilot study. Second, our speculation lacks histological evidence. Third, the onset and duration of ripasudil administration for each individual patient remain indeterminate. An examination of these specifics was unattainable due to prior physician-prescribed use of ripasudil. Such information may facilitate a more informed determination of the optimal time to administer ripasudil. Fourth, it may also be possible that the two groups have unintentional background biases. An assignment by propensity score has the disadvantage of equalizing only the known confounders but not any unknown background variables, which can hold bias. Almost all the current subjects were referred to our hospital, with the treatment being initiated by clinics. Whether ripasudil was prescribed essentially depended on the discretion of the clinic’s physicians; thus, there were no clear selection criteria for ripasudil administration. For example, the raw data (Supplemental Table 1) showed that the ripasudil users had a high proportion of steroid-induced glaucoma. This may be influenced by our previous report that ripasudil had a stronger IOP-decreasing effect in steroid-induced glaucoma than in primary open-angle or exfoliation glaucoma [29].
In conclusion, our study revealed that preoperative ripasudil use showed significantly better outcomes of µTLO at 1 year postoperatively. Given that ripasudil, unlike other major drugs, reduces IOP through the trabecular outflow pathway, this study may suggest that ripasudil does not induce disuse atrophy of this pathway.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Materials availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Tanihara H, Inoue T, Yamamoto T, Kuwayama Y, Abe H, Fukushima A, Suganami H, Araie M (2016) K-115 clinical study group. One-year clinical evaluation of 0.4% ripasudil (K-115) in patients with open-angle glaucoma and ocular hypertension. Acta Ophthalmol 94:e26-34. https://doi.org/10.1111/aos.12829
Honjo M, Tanihara H (2018) Impact of the clinical use of ROCK inhibitor on the pathogenesis and treatment of glaucoma. Jpn J Ophthalmol 62:109–126. https://doi.org/10.1007/s10384-018-0566-9
Okamoto M, Nagahara M, Tajiri T, Nakamura N, Fukunishi N, Nagahara K (2020) Rho-associated protein kinase inhibitor induced morphological changes in type VI collagen in the human trabecular meshwork. Br J Ophthalmol 104:392–397. https://doi.org/10.1136/bjophthalmol-2018-312991
Francis BA, Akil H, Bert BB (2017) Ab interno Schlemm’s canal surgery. Dev Ophthalmol 59:127–146. https://doi.org/10.1159/000458492
Allen L, Burian HM (1962) Trabeculotomy ab externo: a new glaucoma operation: technique and results of experimental surgery. Am J Ophthalmol 53:19–26
Sieck EG, Epstein RS, Kennedy JB, SooHoo JR, Pantcheva MB, Patnaik JL, Wagner BD, Lynch AM, Kahook MY, Seibold LK (2018) Outcomes of Kahook dual blade goniotomy with and without phacoemulsification cataract extraction. Ophthalmol Glaucoma 1:75–81. https://doi.org/10.1016/j.ogla.2018.06.006
Gosling D, Wang H, Auger G (2022) Early results of irrigating goniectomy with trabEx+: a novel device for the treatment of open-angle glaucoma. J Glaucoma 31:268–273. https://doi.org/10.1097/IJG.0000000000001994
Mathew DJ, Buys YM (2020) Minimally invasive glaucoma surgery: a critical appraisal of the literature. Annu Rev Vis Sci 6:47–89. https://doi.org/10.1146/annurev-vision-121219-081737
Tanito M, Sano I, Ikeda Y, Fujihara E (2017) Short-term results of microhook ab interno trabeculotomy, a novel minimally invasive glaucoma surgery in Japanese eyes: initial case series. Acta Ophthalmol 95:e354-360. https://doi.org/10.1111/aos.13288
Mori S, Tanito M, Shoji N, Yokoyama Y, Kameda T, Shoji T et al (2021) Noninferiority of microhook to trabectome: trabectome versus ab interno microhook trabeculotomy comparative study (Tram Trac Study). Ophthalmol Glaucoma 5:452–461. https://doi.org/10.1016/j.ogla.2021.11.005
Okuda M, Mori S, Takano F, Murai Y, Ueda K, Sakamoto M, Takuji K, Makoto Y-N (2022) Association of the prolonged use of anti-glaucoma medications with the surgical failure of ab interno microhook trabeculotomy. Acta Ophthalmol. https://doi.org/10.1111/aos.15090
Mori S, Murai Y, Ueda K, Sakamoto M, Kurimoto T, Yamada-Nakanishi Y, Makoto N (2020) A comparison of the 1-year surgical outcomes of ab externo trabeculotomy and microhook ab interno trabeculotomy using propensity score analysis. BMJ Open Ophthalmol 5:e000446. https://doi.org/10.1136/bmjophth-2020-000446
Sotani N, Kusuhara S, Matsumiya W, Okuda M, Mori S, Sotani R, Kim KW, Nishisho R, Nakamura M (2022) Outcomes of microhook ab interno trabeculotomy in consecutive 36 eyes with uveitic glaucoma. J Clin Med 11:3768. https://doi.org/10.3390/jcm11133768
Mori S, Murai Y, Ueda K, Sakamoto M, Kurimoto T, Yamada-Nakanishi Y, Makoto N (2021) Comparison of efficacy and early surgery-related complications between one-quadrant and two-quadrant microhook ab interno trabeculotomy: a propensity score matched study. Acta Ophthalmol 99:898–903. https://doi.org/10.1111/aos.14787
Iwao K, Inatani M, Tanihara H, Japanese Steroid-Induced Glaucoma Multicenter Study Group (2011) Success rates of trabeculotomy for steroid-induced glaucoma: a comparative, multicenter, retrospective cohort study. Am J Ophthalmol 151:1047-1056.e1. https://doi.org/10.1016/j.ajo.2010.11.028
Ngai P, Kim G, Chak G, Lin K, Maeda M, Mosaed S (2016) Outcome of primary trabeculotomy ab interno (Trabectome) surgery in patients with steroid-induced glaucoma. Medicine 95:e5383. https://doi.org/10.1097/MD.0000000000005383
Jea SY, Francis BA, Vakili G, Filippopoulos T, Rhee DJ (2012) Ab interno trabeculectomy versus trabeculectomy for open-angle glaucoma. Ophthalmology 119:36–42. https://doi.org/10.1016/j.ophtha.2011.06.046
Ahuja Y, Ma KhinPyi S, Malihi M, Hodge DO, Sit AJ (2013) Clinical results of ab interno trabeculotomy using the trabectome for open-angle glaucoma: the Mayo Clinic series in Rochester, Minnesota. Am J Ophthalmol 156:927-935.e2. https://doi.org/10.1016/j.ajo.2013.06.001
Okeke CO, Miller-Ellis E, Rojas M, Group TTS (2017) Trabectome success factors. Medicine (Baltimore) 96:e7061. https://doi.org/10.1097/MD.0000000000007061
Kono Y, Kasahara M, Hirasawa K, Tsujisawa T, Kanayama S, Matsumura K, Morita T, Shoji N (2020) Long-term clinical results of trabectome surgery in patients with open-angle glaucoma. Graefes Arch Clin Exp Ophthalmol 258:2467–2476. https://doi.org/10.1007/s00417-020-04897-0
The Japan Glaucoma Society Guidelilnes for Glaucoma (5th Edition) (2022) Nippon Ganka Gakkai Zasshi 126:85–177
Toris CB, Zhan G, Camras CB (2004) Increase in outflow facility with unoprostone treatment in ocular hypertensive patients. Arch Ophthalmol 122:1782–1787. https://doi.org/10.1001/archopht.122.12.1782
Barany EH (1962) The mode of action of pilocarpine on outflow resistance in the eye of a primate (Cercopithecus ethiops). Invest Ophthalmol 1:712–727
Nakamura N, Honjo M, Yamagishi R, Igarashi N, Sakata R, Aihara M (2021) Effects of selective EP2 receptor agonist, omidenepag, on trabecular meshwork cells, Schlemm’s canal endothelial cells and ciliary muscle contraction. Sci Rep 11:16257. https://doi.org/10.1038/s41598-021-95768-z
Johnson DH, Matsumoto Y (2000) Schlemm’s canal becomes smaller after successful filtration surgery. Arch Ophthalmol 118:1251–1256. https://doi.org/10.1001/archopht.118.9.1251
Baudouin C, Denoyer A, Desbenoit N, Hamm G, Grise A (2012) In vitro and in vivo experimental studies on trabecular meshwork degeneration induced by benzalkonium chloride (an American Ophthalmological Society thesis). Trans Am Ophthalmol Soc 110:40–63
Alvarado JA, Alvarado RG, Yeh RF, Franse-Carman L, Marcellino GR, Brownstein MJ (2005) A new insight into the cellular regulation of aqueous outflow: how trabecular meshwork endothelial cells drive a mechanism that regulates the permeability of Schlemm’s canal endothelial cells. Br J Ophthalmol 89:1500–1505. https://doi.org/10.1136/bjo.2005.081307
Futakuchi A, Inoue T, Fujimoto T, Inoue-Mochita M, Kawai M, Tanihara H (2016) The effects of ripasudil (K-115), a Rho kinase inhibitor, on activation of human conjunctival fibroblasts. Exp Eye Res 149:107–115. https://doi.org/10.1016/j.exer.2016.07.001
Kusuhara S, Nakamura M (2020) Ripasudil hydrochloride hydrate in the treatment of glaucoma: safety, efficacy, and patient selection. Clin Ophthalmol 14:1229–1236. https://doi.org/10.2147/OPTH.S216907
Acknowledgements
The authors thank AJE (https://www.aje.com/) for the English language review.
Funding
Open access funding provided by Kobe University.
Author information
Authors and Affiliations
Contributions
Data curation, Mina Okuda; visualization, Mina Okuda; drafting, Mina Okuda and Sotaro Mori; conceptualization, Sotaro Mori; supervision, Makoto Nakamura; critical reading and reviewing: Kaori Ueda, Mari Sakamoto, Sentaro Kusuhara, Yuko Yamada‑Nakanishi, and Makoto Nakamura. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study adhered to the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board of Kobe University (no. B200091).
Consent to participate
Opt-out consent was obtained from all patients. This method was used for participant recruitment in the study. Informed consent was not obtained from the patients as this study was retrospective and observational. However, patients were allowed to withdraw their consent anytime in an opt-out fashion.
Conflicts of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Okuda, M., Mori, S., Ueda, K. et al. Favorable effect of ripasudil use on surgical outcomes of microhook ab interno trabeculotomy. Graefes Arch Clin Exp Ophthalmol 261, 2603–2610 (2023). https://doi.org/10.1007/s00417-023-06040-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-023-06040-1