Abstract
Purpose
To determine the predictability of success and the risk of open conjunctival revision in the subsequent eye after XEN45 Gel Stent implantation according to lens status.
Methods
This was a retrospective single-centre study involving 132 eyes of 66 participants who had undergone intraocular pressure (IOP)-lowering XEN45 Gel Stent implantation, either as a standalone procedure in phakic and pseudophakic eyes or in combination with phacoemulsification. Successful surgery was defined by three scores: IOP at follow-up < 21 mmHg (score A) or < 18 mmHg (score B) and an IOP reduction > 20% or IOP ≤ 15 mmHg and an IOP reduction ≥ 40% (score C). In all scores, one open conjunctival revision was allowed, and additional repeat surgery was considered a failure. The predictability of success and revision rate depending on the outcome of the first eye were calculated using Bayes’ theorem.
Results
IOP-lowering did not differ significantly between the first and second eyes. Success rates of standalone surgery in the second eye after successful surgery in the first eye significantly exceed rates after prior failure. For the combined procedure, the rates did not differ significantly. For score A, we determined a 76.6% chance of success following a prior success and a 57.9% chance, if prior surgery failed. The corresponding probabilities were 75% and 59.1% for score B, while 66.7% and 15.7% for score C, respectively. We calculated a 60% risk for revision surgery in the standalone phakic group. If the first eye was not revised, the risk of revision in the subsequent eye was 20%. The corresponding risks were 72.7% and 5% for the standalone procedure in pseudophakic patients and 38.4% and 41.7% for the combined procedure, respectively.
Conclusion
The results of our study offer a tool to predict the outcome of subsequent eye surgeries based on either the outcome in the initial eye and the type of surgery performed, owing to the high predictive potential.
Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
Being a primarily bilateral disease, glaucoma often requires surgical treatment on both eyes. Few studies have focused on whether the positive outcome of glaucoma surgery in the first eye has a predictive potential for success or clinical course influence in the subsequent eye. Mietz et al. reported that primary trabeculectomy in the fellow eye is associated with a greater risk of cyst formation in Tenon’s capsule [1].
In the past decades, traditional filtering surgeries, such as trabeculectomy or implantation of large lumen drainage devices, are the main treatment options for uncontrolled glaucoma. More recently, microinvasive glaucoma surgery (MIGS) has been used in routine clinical practice, in addition to established procedures. One of such is XEN45 Gel Stent implantation (Allergan, Dublin, CA, USA), which is a subconjunctival bleb-forming procedure that pursues an ab interno approach. Primary implantation is carried out via the anterior chamber through the trabecular meshwork and the scleral wall; hence, it does not require penetration of the conjunctiva. In addition to a moderate flow of aqueous humour through the small lumen, these factors contribute to a favourable safety profile, along with a promising intraocular pressure (IOP)-lowering potential [2,3,4,5,6].
In a recent study, Gillmann et al. determined considerable outcome predictability for the second eye based on the outcome after XEN45 Gel Stent implantation in the first eye, but they did not differentiate between the standalone and combined procedures [7].
However, secondary interventions are frequently needed because of postoperative scarring of the conjunctiva. Several studies have shown that combined stent implantation with phacoemulsification results in higher revision rates than the standalone procedure [2, 8]. This finding supports the question of whether phakic status or the combination with phacoemulsification exerts an influence on the predictive potential of successful XEN45 Gel Stent implantation in subsequent eyes, based on the outcome of the first operated eye.
For this reason, we investigated the outcomes between fellow eyes using different clinical scores to determine the predictive potential of the second eye surgery within groups of phakic or pseudophakic patients who underwent the standalone procedure and those who received combined stent implantation with phacoemulsification.
Methods
This was a single-centre retrospective study based on the data acquired from the Department of Ophthalmology, St. Martinus-Krankenhaus, Düsseldorf, Germany. This study included all patients who underwent XEN45 Gel Stent implantation either as a standalone procedure or in combination with phacoemulsification, from 2015 to 2021. A total of 812 eyes of 737 patients were identified in our database, with 154 patients having received XEN45 Gel Stent implantation in both eyes. The inclusion criteria were an available baseline and a postoperative follow-up IOP value in patients undergoing XEN45 Gel Stent implantation in both eyes after at least 6 months and a maximum latency of 6 months between the surgery of the first and second eye. Eyes with secondary types of glaucoma, such as uveitic, neovascular, pigment dispersion, or dysgenetic glaucoma, were excluded (n = 6).
Considering the aforementioned criteria, 132 eyes of 66 patients remained in the study group, 122 were classified as having primary open-angle glaucoma (POAG), and 10 had exfoliation glaucoma (XFG). The epidemiological and baseline data are presented in Table 1.
The spectrum of prior eye surgery comprised selective laser trabeculoplasty (n = 27), ab interno trabeculectomy (n = 8), and 23 g pars plana vitrectomy (n = 2).
IOP was assessed using Goldmann applanation tonometry. A maximum of three IOP measurements prior to the date of the surgery were collected and averaged to evaluate the baseline IOP. Additional parameters included from the patients’ files were the type of glaucoma, maximum preoperative IOP, number of preoperative glaucoma medications, cup/disc ratio, and best-corrected visual acuity (BCVA) at baseline. The medication score comprised the amount of IOP-lowering medication classes applied at baseline and at follow-up.
The clinical endpoint at the longest follow-up examination was defined as either success or failure based on three separate scores. According to scores A and B, an absolute IOP < 21 mmHg (score A) or < 18 mmHg (score B) at follow-up examination and a postoperative IOP reduction of > 20% qualified for success. The two scores were chosen according to the tube versus trabeculectomy study [9]. The criteria for score C were an absolute IOP of 15 mmHg or less, and a postoperative IOP reduction of 40% or more, according to the criteria of the World Glaucoma Association [10]. In all scores, one open conjunctival revision was allowed. The aim of surgery was to lower the IOP without the use of medication; therefore, surgical revision was prioritised over repeat prescription of anti-glaucoma medication, unless the patient did not prefer additional surgery. Performing a second open conjunctival revision or repeat surgery was considered a failure.
Surgical technique
Implantation of the XEN45 Gel Stent was performed as previously described [2, 11]. First, 0.1 ml of mitomycin C (0.1 mg/ml) was injected under the conjunctiva of the upper nasal quadrant, at a distance of 6 mm from the limbus. After temporal paracentesis, paracentesis at the 5 or 7 o’clock position, and anterior chamber stabilisation using a viscoelastic substance, the stent was placed using its injector device. The apex of the injector was driven through the trabecular meshwork and sclera at a distance of 3 mm from the limbus. The stent was then injected under the conjunctiva and the injector was removed. The position of the stent was confirmed via gonioscopy, and the viscoelastic substance was removed from the anterior chamber by irrigation.
For performing combined XEN45 Gel Stent implantation with phacoemulsification, a standard 2.5–2.8-mm clear corneal incision was made in the temporal cornea after the subconjunctival injection of mitomycin C. Two paracenteses were positioned at a 90° angle to the tunnel following bimanual phacoemulsification with posterior chamber and in-the-bag intraocular lens (IOL) implantation. Thereafter, stent implantation was performed as previously described [2, 11].
The aim of the surgery was to regulate the IOP without antiglaucomatous medication. Therefore, all patients without a sufficiently reduced IOP postoperatively underwent surgical revision. Instead of needling, we performed an open conjunctival approach, as described in our previous study [2, 12]. Briefly, the conjunctiva was incised at the limbus, the stent was located, and surrounding tissue was removed using microscissors and microforceps. After removal of scar tissues, the conjunctiva was refixated at the limbus with two absorbable 9.0 vicryl sutures (Coated Vicryl, Ethicon, New Brunswick, NJ, USA).
Standardised postoperative topical therapy was applied, including antibiotics (Floxal AS, Bausch & Lomb, Frankfurt, Germany) and steroid ointments (Ultracortenol AG, Agepha, Senec, Slovakia), both administered three times a day for 4 weeks. Previous topical anti-glaucomatous medications were discontinued.
Ethics and statistics
The study and data collection were conducted with the approval of the institutional review board (Ethik und Kommission Klinische Studien, Dernbacher Gruppe Katharina Kasper, Germany). The tenets of the Declaration of Helsinki were regarded. Statistical analyses were performed using SPSS (version 24.0; IBM Corp. Armonk, NY, USA) and the statistical programming language R V3.2.2 (R Foundation for Statistical Computing, Vienna, Austria).
Outcomes in the first and second eyes, as well as the surgical success in subsequent eyes following either success or failure in the first eye, were compared using the log-rank test and visualised using Kaplan–Meier curves. Comparative analyses between mean IOP measurements at different time intervals as well as between preoperative and postoperative medication scores at follow-up were performed using Student’s t-test for paired samples. The chances of success in the subsequent eye after successful or failed surgery in the first eye as well as the risk for open conjunctival revision in the second eye after revision or absence of revision surgery in the first eye were calculated according to Bayes’ theorem. The use of the model for determining positive predictive values and conditional probabilities in clinical situations has been described in detail previously [13,14,15]. Statistical significance was set at p < 0.05.
Results
Baseline characteristics
The mean follow-up time interval was 17.6 ± 9.6 months in the first eye group and 15.6 ± 8.6 months in the second eye group (p = 0.22). During this follow-up period, XEN45 Gel Stent implantation significantly reduced the IOP (Table 1).
A total of 52 eyes (39%) underwent one open conjunctival revision, of which, three eyes (2%) required a second surgical revision using the same technique. Four of these eyes (3%) underwent additional glaucoma surgery at a later time point: trabeculectomy (n = 2) and cyclophotocoagulation (n = 2). In seven revised eyes (5%), intraoperative preparation of the stent showed a functional deficit, and the stent was replaced in the same surgical session.
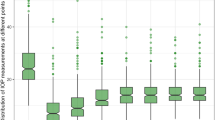
Survival analysis in the first and second eyes
For both standalone and combined procedures, a comparative analysis between the outcome in the first and second eyes, with regard to the defined criteria for surgical success, did not show a significant difference. The Kaplan–Meier curves displayed corresponding trends, which remained parallel throughout the study (Fig. 1).
Kaplan–Meier survival curves comparing the success rates in the first and second eyes after standalone vs. combined XEN45 Gel Stent implantation. Score A: IOP at follow-up < 21 mmHg, IOP reduction > 20%, no repeat surgery. Score B: IOP at follow-up < 18 mmHg, IOP reduction > 20%, no repeat surgery. Score C: IOP at follow-up ≤ 15 mmHg, IOP reduction ≥ 40%, no repeat surgery
Mean preoperative IOP was 21.9 ± 5.4 mmHg in the first eye, which was higher than that of the second eye at 20.6 ± 3.7 mmHg and no significant difference was determined (p = 0.12).
In both groups, postoperative IOP values and medication scores remained stable at significantly lower levels throughout the follow-up timeframes at 6, 9, 12, 18, 24, 36, and 48 months, as the first and subsequent eyes did not show significant differences during follow-up (Table 2).
Survival analysis in the subsequent eyes regarding the outcome in the first eyes
For standalone stent implantation survival analysis in the second eye, comparing cases with prior success or failure in the first eye determined a significant difference in the success rates for all scores (p < 0.05). Standalone stent implantation in the second eye after successful surgery in the first eye led to significantly better success rates than that in cases of prior failure (Fig. 2). In the combined group, there was no significant difference according to this criterion (p > 0.05).
Kaplan–Meier survival curves comparing the success rates in the second eye after either successful or failed surgery of the first eye following standalone vs. combined XEN45 Gel Stent implantation. Score A: IOP at follow-up < 21 mmHg, IOP reduction > 20%, no repeat surgery. Score B: IOP at follow-up < 18 mmHg, IOP reduction > 20%, no repeat surgery. Score C: IOP at follow-up ≤ 15 mmHg, IOP reduction ≥ 40%, no repeat surgery
Probability calculations
According to Bayes’ theorem, which was used for probability calculation in determining the success and risk for open conjunctival revision in the second eye based on the outcome of the first eye, we found a 76.6% chance of success following a prior success for score A. However, if the first eye failed after surgery, the chance of success in the subsequent eye was reduced to 57.9%. The corresponding probabilities were 75% and 59.1% for score B and 66.7% and 15.7% for score C, respectively (Table 3).
Probability calculations determined a 60% risk for revision surgery following a prior revision of the first eye for the standalone procedure in phakic patients. If the first eye was not revised, the risk of revision in the subsequent eye was 20%. The corresponding probabilities were 72.7% and 5% for the standalone procedure in pseudophakic patients and 38.4% and 41.7% for the combined procedure, respectively (Table 4).
In the combined surgery group, the latter turned out to be relatively high, compared to the moderate chance of success for the second eye after prior success. In contrast, the range between both chances of success is considerably larger in cases that have undergone a standalone procedure.
Side effects
Side effects included hyphema (n = 5), stent exposure (n = 2), cystoid macular edema (n = 1), and self-limited choroidal effusion due to transient hypotony (n = 1). Stent exposure required surgical revision and was counted as a re-surgery. No severe side effects were observed.
Discussion
Consistent with previous studies, our study provided further evidence that XEN45 Gel Stent implantation effectively reduces both IOP and medication scores [2,3,4, 8].
Including only patients who underwent surgery in both eyes, we addressed three questions: First, does the outcome of the first eye influence the outcome of the second eye. Second, do intra-individual correlations differ between pseudophakic and phakic eyes or combined surgery, and third, does revision surgery in the first eye have a predictive value for revision surgery in the second eye.
Only a few studies have described the outcomes of the fellow eye after glaucoma surgery. Predictive values for trabecular aspiration and trabectome surgery have been reported [15, 16]. Upon filtering surgery investigations, Mietz et al. showed similar trends in the success rate of fellow eyes after trabeculectomy [1].
Recently, Gillmann et al. found a considerable intra-individual correlation between the outcomes following bilateral XEN45 Gel Stent implantation in a mixed cohort [7]. This study did not investigate differences between subgroups according to lens status and did not compare standalone surgery versus combined surgery.
Our results suggest that the predictability of success or revision rates is highly dependent on either phakic status and the combination with phacoemulsification at the time XEN45 Gel Stent implantation was performed. Predictability was higher when aiming at lower postoperative IOP values.
Considering the predictive potential for standalone surgery in second eyes derived from our data, we can conclude that, if surgical success is defined according to score A (IOP at follow-up < 21 mmHg, IOP reduction > 20%) and score B (IOP at follow-up < 18 mmHg, IOP reduction > 20%), XEN45 Gel Stent implantation for the subsequent eye still is a viable option after a failed first case. However, if the surgeon aims for lower IOP values for the second eye (score C: IOP at follow-up ≤ 15 mmHg, IOP reduction ≥ 40%), it might be reasonable to consider other filtering approaches.
Our results on the intra-individual correlation raise the question of whether there are factors that influence individual surgical outcomes. One of which might be individual susceptibility to subconjunctival scarring. In an extensive literature review, Broadway et al. listed unilateral predisposing issues, such as previous ocular surgery or secondary glaucoma due to trauma, uveitis, or neovascularisation, as well as bilateral risk factors. The latter include black skin colour, young age, and previous glaucoma medication when applied simultaneously. There is evidence that large amounts of benzalkonium chloride can cause drug-induced conjunctival inflammation and fibroblast proliferation, which is of crucial importance in the postoperative setting [17, 18].
Another factor that could act as an inter-individual variable in the surgical success rate is the lymphatics of the subconjunctival tissue, assuming that the function of drainage pathways is parallel among fellow eyes [19].
A reason for either diverging outcomes after standalone and combined surgery, as well as for a tendency toward more asymmetric outcomes among fellow eyes after the latter, could be found in the inflammatory response after surgery. Fellow-eye investigations after phacoemulsification have determined diverse concentrations of inflammatory chemokines in the aqueous humour of the first and second operated eyes as a reason for increased pain after second-eye surgery [20].
These molecular factors may contribute to the asymmetric response of IOP as a result of postoperative inflammation and subconjunctival scarring.
Combining traditional filtering surgery with phacoemulsification has been the subject of numerous studies. In the context of a meta-analysis, Friedman et al. found evidence that shows how phacotrabeculectomy results in less sufficient IOP reduction than standalone trabeculectomy [21].
It was postulated that increased trauma associated with a combined surgery leads to higher levels of transforming growth factor-beta 2 in the aqueous humour and prolonged alteration of the blood-aqueous barrier [22, 23]. These mechanisms might apply to combined XEN45 Gel Stent implantation with cataract surgery and the greater extent of its inter-individually varying outcomes compared to standalone surgery.
Notably, baseline IOP was lower in the combined surgery group than in both groups that received standalone surgery, which might have influenced a weaker relative IOP reduction. However, the mean postoperative IOP at the longest follow-up examination was markedly higher in the combined surgery group than in the standalone phakic and standalone pseudophakic group.
Moreover, the mean preoperative IOP in the second eye was significantly lower than that in the first eye. This might be brought about by the standard operating procedures of our department, which specifies that when the indication for XEN45 Gel Stent implantation is given for both eyes, surgery on the eye with the higher IOP is performed first, which in turn might have an impact on lower postoperative IOP values and higher success rates. The limitations of our study include its retrospective design, limited availability of follow-up data, and limited sample sizes among the three subgroups.
In summary, the results of our study offer a tool for glaucoma surgeons to estimate the success rates and risk of open conjunctival revision of the subsequent eye. We conclude that either the outcome of the first eye following XEN45 Gel Stent implantation or the type of surgery performed has an impact on the predictive potential and may help in decision-making when a second eye is considered for surgery.
Change history
03 March 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00417-022-05614-9
Abbreviations
- BCVA:
-
Best-corrected visual acuity
- C/D:
-
Cup/disc
- IOL:
-
Intraocular lens
- IOP:
-
Intraocular pressure
- MIGS:
-
Microinvasive glaucoma surgery
- POAG:
-
Primary open-angle glaucoma
- SD:
-
Standard deviation
- XFG:
-
Exfoliation glaucoma
References
Mietz H, Jacobi PC, Welsandt G, Krieglstein GK (2002) Trabeculectomies in fellow eyes have an increased risk of tenon’s capsule cysts. Ophthalmology 109(5):992–997
Widder RA, Dietlein TS, Dinslage S, Kühnrich P, Rennings C, Rössler G (2018) The XEN45 Gel Stent as a minimally invasive procedure in glaucoma surgery: success rates, risk profile, and rates of re-surgery after 261 surgeries. Graefes Arch Clin Exp Ophthalmol 256(4):765–771
Schlenker MB, Gulamhusein H, Conrad-Hengerer I, Somers A, Lenzhofer M, Stalmans I, Reitsamer H, Hengerer FH, Ahmed IIK (2017) Efficacy, safety, and risk factors for failure of standalone ab interno gelatin microstent implantation versus standalone trabeculectomy. Ophthalmology 124(11):1579–1588
Reitsamer H, Sng C, Vera V, Lenzhofer M, Barton K, Stalmans I (2019) Two-year results of a multicenter study of the ab interno gelatin implant in medically uncontrolled primary open-angle glaucoma. Graefes Arch Clin Exp Ophthalmol 257(5):983–996
Reitsamer H, Vera V, Ruben S, Au L, Vila-Arteaga J, Teus M, Lenzhofer M, Shirlaw A, Bai Z, Balaram M, Stalmans I (2021) Three-year effectiveness and safety of the XEN gel stent as a solo procedure or in combination with phacoemulsification in open-angle glaucoma: a multicentre study. Acta Ophthalmol. Online ahead of print.
Gabbay IE, Goldberg M, Allen F, Lin Z, Morley C, Pearsall T, Muraleedharan V, Ruben S (2021) Efficacy and safety data for the ab interno XEN45 gel stent implant at 3 years: a retrospective analysis. Eur J Ophthalmol. Online ahead of print.
Gillmann K, Bravetti GE, Rao HL, Mermoud A, Mansouri K (2020) Bilateral XEN stent implantation: a long-term prospective study of the difference in outcomes between first-operated and fellow eyes. J Glaucoma 29(7):536–541
Gillmann K, Bravetti GE, Rao HL, Mermoud A, Mansouri K (2020) Combined and stand-alone XEN 45 gel stent implantation: 3-year outcomes and success predictors. Acta Ophthalmol 99(4):e531–e539
Gedde SJ, Schiffman JC, Feuer WJ, Herndon LW, Brandt JD, Budenz DL (2009) Three-year follow-up of the tube versus trabeculectomy study. Am J Ophthalmol 148(5):670–684
Shaarawy TM, Sherwood MB, Grehn F (2009) Guidelines on design and reporting of glaucoma surgical trials. Kugler, Amsterdam
Widder RA, Lappas A, Rennings C, Matthias H, Dietlein TS, Rößler GF (2020) Primary versus post-trabeculectomy XEN45 Gel Stent implantation. J Glaucoma 29(12):1115–1119
Widder RA, Rennings C, Rössler GF (2020) [Open conjunctival revision after XEN45 gel stent implantation as a standardized procedure A step by step guide.]. Der Ophthalmologe. 117(8): 806–810
Kasahara N (2013) Bayesian methods and decision making in glaucoma. Vis Pan-Am 12(3):69–72
Thomas R, Mengersen K, Parikh RS, Walland MJ, Muliyil J (2011) Enter the reverend: introduction to and application of Bayes’ theorem in clinical ophthalmology. Clin Exp Ophthalmol 39(9):865–870
Kiessling D, Rennings C, Hild M, Lappas A, Dietlein TS, Roessler GF, Widder RA (2021) Predictability of ab-interno trabeculectomy success in the subsequent eye: a contralateral eye comparison study. Clin Experiment Ophthalmol 49(3):242–250
Rosentreter A, Dinslage S, Krieglstein GK, Dietlein TS (2009) Intra-individual comparison after combined phaco-trabecular aspiration in pairs of pseudoexfoliative eyes. Graefes Arch Clin Exp Ophthalmol 248(1):79–83
Broadway DC, Chang LP (2001) Trabeculectomy, risk factors for failure and the preoperative state of the conjunctiva. J Glaucoma 10(3):237–249
Baudouin C, Pisella PJ, Fillacier K, Goldschild M, Becquet F, De Saint JM, Béchetoille A (1999) Ocular surface inflammatory changes induced by topical antiglaucoma drugs: human and animal studies. Ophthalmology 106(3):556–563
Yu D-Y, Morgan WH, Sun X, Su E-N, Cringle SJ, Yu PK, House P, Guo W, Yu X (2009) The critical role of the conjunctiva in glaucoma filtration surgery. Prog Retin Eye Res 28(5):303–328
Zhu XJ, Wolff D, Zhang KK, He WW, Sun XH, Lu Y, Zhou P (2015) Molecular inflammation in the contralateral eye after cataract surgery in the first eye. Invest Ophthalmol Vis Sci 56(9):5566–5573
Friedman DS, Jampel HD, Lubomski LH, Kempen JH, Quigley H, Congdon N, Levkovitch-Verbin H, Robinson KA, Bass EB (2002) Surgical strategies for coexisting glaucoma and cataract: an evidence-based update. Ophthalmology 109(10):1902–1913
Siriwardena D, Kotecha A, Minassian D, Dart JK, Khaw PT (2000) Anterior chamber flare after trabeculectomy and after phacoemulsification. Br J Ophthalmol 84(9):1056–1057
Verges C, Cazal J, Lavin C (2005) Surgical strategies in patients with cataract and glaucoma. Curr Opin Ophthalmol 16(1):44–52
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional review board as well as the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The Institutional Review Board (Ethik und Kommission Klinische Studien, Dernbacher Gruppe Katharina Kasper, Germany) approved the study.
Conflict of interest
David Kiessling: none; Corinna Rennings: none; Matthias Hild: none; Alexandra Lappas: none; Gernot F. Roessler: none; Randolf A. Widder: none; Thomas S. Dietlein: Santen Pharmaceutical Osaka Japan, Alcon Fort Worth USA. Stock interest: Bayer Leverkusen Germany, Johnson and Johnson New Brunswick, NJ. Lectures: Thea Pharma Schaffhausen Switzerland, iStar Medical Wawre Belgium, MeyeTech Alsdorf, Germany.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised. Author names are now corrected.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kiessling, D., Rennings, C., Hild, M. et al. Predictability of success and open conjunctival revision rates in the subsequent eye after XEN45 Gel Stent implantation according to lens status. Graefes Arch Clin Exp Ophthalmol 260, 2639–2647 (2022). https://doi.org/10.1007/s00417-022-05569-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-022-05569-x