Abstract
Purpose
Determine the anatomical consequences of delaying intravitreal injection (IVI) therapy with anti-vascular endothelial growth factor (anti-VEGF) in patients using treat-and-extend (T&E) protocol.
Methods
Retrospective medical record review of consecutive patients receiving intravitreal anti-VEGF therapy using T&E protocol prior to and during the COVID-19 pandemic.
Results
The study included 923 eyes of 691patients; 58.8% (543 eyes), 25% (231 eyes), and 16.2% (149 eyes) had nvAMD, DME, and RVO, respectively. Mean (± SD) patient age was 74.5 ± 11.7 years. Overall, 56.3% of cases had a delay in therapy of ≥ 7 days; specifically, 56.2%, 61.5%, and 49.0% of nvAMD, DME, and RVO cases, respectively, had a delay. The median delay in days, among cases ≥ 7 days late was 21 (IQR 7 to 42) days, with 21(IQR 7 to 45), 22.5(IQR 8 to 42), and 14(IQR 7 to 33.5) days of delay among patients with nvAMD, DME, and RVO, respectively. Delaying therapy by ≥ 7 days resulted in increased CST in 47.5%, 58.5%, and 58.9% of nvAMD, DME, and RVO cases, respectively, with a significant correlation between the length of treatment delay and the increase in CST (Spearman’s rho: 0.196; p < 0.001).
Conclusions
Delayed IVI treatment in eyes treated with T&E protocol was associated with increased macular thickness with potential consequences with respect to visual outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
Neovascular age-related macular degeneration (nvAMD), diabetic macular edema (DME), and macular edema associated with retinal vein occlusion (RVO) are often treated long-term with intravitreal injections (IVI) of anti-vascular endothelial growth factor (anti-VEGF) in order to prevent progressive vision loss [1,2,3,4,5,6]. Additionaly, a treat-and-extend (T&E) regimen in which the treatment interval is progressively extended is often used to resolve the retinal and/or subretinal exudates often associated with these conditions and prevent their recurrence [7, 8]. The T&E approach has been shown to achieve similar visual and anatomical outcomes compared to PRN (pro re nata) and monthly treatment regimens for nvAMD and DME [6,7,8,9]. Nevertheless, limited data is available regarding the consequences of deviating from the recommended treatment schedule.
The COVID-19 pandemic has severely disrupted standard patient care worldwide, leading to deviations and/or delays in the planned treatment schedule in many patients, due primarily to difficulties related to treatment access and/or patient fears of contracting the SARS-CoV-2 virus [10,11,12,13,14,15].
Recent reports regarding compliance with anti-VEGF treatment schedules have documented a decrease of up to 50% in the number of planned IVI treatments during the pandemic compared to the corresponding pre-pandemic period [11,12,13,14,15]
Previous studies suggest that inadequately treating nvAMD can result in poor visual outcome [16,17,18]; moreover, intraretinal fluid (IRF) can have a worse effect on vision compared to subretinal fluid (SRF). In addition, an increase (or new onset) of retinal fluid is more likely to cause vision loss compared to either a lack of fluid or persistent fluid [19]. Similarly, inadequately treating central retinal vein occlusion (CRVO) can adversely affect visual outcome [5]. With respect to DME, Bressler et al. [20] reported a low risk of substantial vision loss (i.e., ≥ 2 lines) when in patients treated using anti-VEGF IVI therapy, regardless of the persistence of edema; on the other hand, Weiss et al. found that missing scheduled IVI treatments can cause reduced treatment efficacy and poorer visual outcome in patients with DME [21].
The purpose of this study was to examine the effects of delays experienced with scheduled IVI treatments in patients who were treated in our clinic using the T&E protocol, using data collected during the COVID-19 pandemic as a test case.
Methods
Study design and inclusion
We performed a retrospective review of the electronic medical records from eyes that received anti-VEGF treatment in our tertiary referral center (Hadassah – Hebrew University Medical Center). The study was approved by our institutional ethics committee of the Hadassah Medical center and conducted in adherence to the tenets of the Declaration of Helsinki. Informed consent was not required. We included eyes that received anti-VEGF treatment for nvAMD, DME, branch retinal vein occlusion (BRVO), or CRVO during the first two months of the COVID-19 pandemic in Israel (from April 1, 2020, through June 9, 2020); during this period, a lockdown and restrictive measures were enforced. Additionaly, the patients in our study had to be over 18 years old. A total of 1078 eligible eyes received IVI treatment during this period. We excluded 79 eyes that received IVI treatment for other indications, 5 eyes that received the first IVI treatment during the study period, and 71 eyes for which data were missing or had low-quality OCT data. The remaining 923 eyes were included in our analysis.
Data collection and analysis
The following data were collected from the patients’ electronic medical records: the patient’s demographics; the eye(s) involved, retinal pathology (nvAMD, DME, or RVO); the number of years since the start of IVI treatment; confirmation of the treatment protocol (T&E, and not PRN or monthly injections); the treatment compound that was recommended and used (bevacizumab, ranibizumab, or aflibercept); and the recommended treatment interval and the actual treatment interval. A delay in treatment was defined as an injection administered ≥ 7 days later than recommended.
T&E strategy aims to resolve retinal and subretinal fluid by providing an initial induction sequence involving at least three-monthly IVI treatments. After this initial series, in cases with macular drying, the eyes continue to receive regular maintenance IVI treatments at extending intervals [8, 9]. In our clinic, patients are routinely treated using an OCT-guided T&E protocol after receiving the three initial monthly injections. Prior to each injection, an OCT scan is performed in order to determine the subsequent treatment interval. Once every three injections, VA and an eye examination are performed. Modifications in treatment intervals are eye dependent and mostly independent of the treatment schedule in the fellow eye in cases of bilaterality. Every newly diagnosed patient with nvAMD, DME, or RVO is usually started on injections of 1.25 mg bevacizumab. Guidelines used to guide switching treatment from bevacizumab to either ranibizumab or aflibercept included the persistence or recurrence of IRF, SRF, and/or sub-RPE fluid despite ≥ 3 monthly injections with the previous compound. During the first months of the COVID-19 pandemic in Israel, VA measurements and clinical examinations for patients who were currently receiving anti-VEGF injections were deferred in the majority of cases [10]. Thus, during the lockdown period, VA was measured for only 65 of the 923 eyes in the study.
A spectral domain OCT (Heidelberg Engineering GmbH, Heidelberg, Germany) was used for all of the eyes included in the study. The OCT images obtained from the last visit before the pandemic and from the first visit during the pandemic were reviewed by a retina specialist prior to IVI treatment, for central subfield thickness [22] (CST, defined as the average thickness in the central 1-mm diameter circle of the ETDRS grid), maximum central subfield thickness (MCST), and the presence of IRF and/or SRF; the presence of IRF/SRF was determined based on a qualitative assessment by the treating physician [23]. Worsening was defined as an increase in CST of ≥ 10% from the pre-pandemic visit to the visit during the pandemic and/or a qualitative increase (or new onset) in the amount of fluid, within or outside of the CST area. Improvement was defined as a reduction in CST of ≥ 10% and/or a qualitative decrease in the amount of retinal fluid or a new finding of an absence of fluid, within or outside of the CST area. Finally, stability was defined as a change in CST of < 10% and no change in the presence/absence of fluid [24].
Statistical analyses were performed using SPSS Statistics, version 25.0 (IBM Corp., Armonk, NY). Frequency counts and percentages were generated where appropriate. Tests of normality were performed on the data, and parametric and non-parametric test were applied as needed. Logistic regression was used to model the probability of the occurrence of binary dependent variables (worsening/no worsening of IRF, SRF, and CST). A multiple linear regression model was calculated in order to predict the number of delayed days in IVI treatment based on the age and disease duration for each of the three retinal pathologies evaluated. Statistical significance was defined as a p-value < 0.05.
Results
Patients and demographics
Our analysis included 923 eyes in 691 patients who received anti-VEGF IVI therapy. The mean (± SD) age of the patients was 74.5 ± 11.7 years, and 52.2% of patients were female. In total, 543 eyes were treated for nvAMD (58.8%), 231 for DME (25.0%), and 149 for RVO (16.2%); 602 eyes were treated with bevacizumab (65.2%), 67 with ranibizumab (7.3%), and 254 with aflibercept (27.5%), (Table 1). The T&E algorithm was applied in all cases.
Delay in treatment compared to the recommended schedule
A delay in IVI treatment occurred in 56.3% of cases (n = 520); 34.7% of cases (n = 320) were treated on or before the recommended date, and 9.0% of cases (n = 83) were treated 1–6 days after the recommended date. Among all 520 eyes that were treated ≥ 7 days late, the median delay was 21(interquartile range (IQR) Q1 to Q3:7 to 42) days. The median delay among nvAMD, DME, and RVO patients that delayed treatment was 21 (IQR 7 to 45), 22.5 (IQR 8 to 42), and 14 (IQR 7 to 33.5) days late, respectively. The delay significantly different between the 3 groups (p < 0.001 in each case).
To analyze the relationship between treatment delay and patient characteristics (e.g., gender, age, number of years that the patient received IVI, type of anti-VEGF compound used for treatment, bilaterality, CST, and MCST), only one eye per patient was included (the right eye in patients with bilateral disease).The treatment delay was similar between men and women (median 7(IQR 0 to 28) vs. median7 (IQR 0 to 20.3) days, respectively p = 0.659), and age was not correlated with the length of delay (Spearman’s rho: 0.05; p = 0.189) In contrast, the number of years that patients received IVI treatment was directly correlated with the length of delay (Spearman’s rho: 0.090; p = 0.017). The median treatment delay was longer among patients with bilateral disease (7 days; IQR: 0 to 35 days) compared to patients with unilateral disease (5.5 days; IQR: 0 to 19.5 days; p = 0.002). Finally, we found no correlation between either baseline CST or length of delay (Spearman’s rho: − 0.012; p = 0.760) and between MCST and length of delay (Spearman’s rho: 0.026; p = 0.489), nor did we find an association between the type of anti-VEGF compound used and the length of delay.
We then performed a subgroup analysis for each retinal pathology. Among the patients with nvAMD, we found a significant correlation between number of years that the patients had received IVI treatment and length of delay (Spearman’s rho: 0.107; p = 0.031). We also found that patients in the nvAMD group who received bevacizumab had a significantly longer median delay (19 days; IQR: 0 to 42 days) compared to both patients who received ranibizumab (7 days; IQR: 0 to 10.5 days; p = 0.011) and patients who received aflibercept (4 days; IQR: 0 to 19 days; p = 0.003); the delay was similar between patients who received ranibizumab and patients who received aflibercept (p = 0.927). No other significant correlations were found between length of delay and any patient characteristics within the nvAMD, DME, or RVO patient subgroups.
Multivariate analysis to predict treatment delays
For nvAMD patients, we used a multiple linear regression model to predict the two factors—namely, the number of days until the next appointment based on disease duration and the anti-VEGF compound used—that univariate analysis indicated was associated with a delay in treatment. We found a significant regression (F(2,402): 6.971, R2 = 0.034; p = 0.001); Specifically, the next treatment was delayed by 0.8 days for each incremental year of disease duration, whereas the interval to the next treatment decreased by 6.7 days as the anti-VEGF compound changed from bevacizumab to either ranibizumab or aflibercept. Disease duration (p = 0.009) and anti-VEGF compound (p = 0.005) were the sole predictors of delayed IVI treatment.We were unable to fit a regression model to the DME and RVO patient groups.
Anatomical consequences of delaying IVI treatment
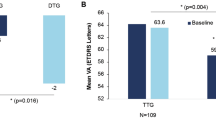
We found a direct correlation between the change in the number of days to treatment (coming either before or after the scheduled IVI treatment) and the change in CST (Spearman’s rho: 0.196; p < 0.001) and MCST (Spearman’s rho: 0.199; p < 0.001 relative to the previous treatment). These data are summarized for each retinal pathology in Table 2.
For each retinal pathology, we found a higher likelihood of increased IRF and/or SRF based on a qualitative assessment and based on a quantitative assessment of CST and MCST in eyes that were treated ≥ 7 days late compared to eyes that were treated within 0–6 days. Table 3 summarizes the number and percentage of eyes with worsening outcome based on the change in IRF and SRF, as well as the mean change in CST and MCST. These data are presented separately for four separate delay periods (7–28 days, 29–56 days, 57–84 days, and > 84 days), each of which was compared to eyes for which treatment was given within 1–6 days.
Quantitative assessment
Among the DME cases, CST increased in 83 out of the 142 eyes (58.5%) that received treatment ≥ 7 days late, with a median increase in CST of 3.5 μm, (IQR: − 9.3 to 68.2 μm; 19.7% of these eyes had an increase of > 50 μm), significantly different (p = 0.007) than eyes for which treatment was received within 0–6 days, where CST decreased by a median of − 2.0 μm, (IQR: − 40.5 to 9.3 μm; 5.2% of these eyes had an increase of > 50 μm). Similarly, among the RVO cases, CST increased in 43 out of the 73 eyes that received treatment ≥ 7 days late, with a median increase of 2.5 μm (IQR: − 9 to 21.5 μm; 17.8% of these eyes had an increase of > 50 μm), significantly different (p = 0.011) than the change in the eyes for which treatment was received between 0 and 6 days (median: − 3.0 μm, IQR: − 47 to 4 μm; 7.1% of these eyes had an increase of > 50 μm).
Regarding nvAMD, 145 of the 305 eyes (46.5%) that were treated ≥ 7 days late had an increase in CST. In these 145 eyes, delaying IVI treatment by ≥ 7 days was associated with a change in CST (median: 0.0 μm, IQR: − 9.5 to 15 μm; 12.1% of these eyes had an increase of > 50 μm), similar to the change in CST among the eyes that were treated within 0–6 days (p = 0.315; median: − 1.0 μm, IQR: − 13 to 7 μm; 4.2% of these eyes had an increase of > 50 μm). However, the proportion of eyes demonstrating an increase in CST of > 50 μm were not the same (12.1% vs 4.2%; p = 0.002, respectively).
Qualitative assessment
A qualitative assessment of the OCT scans of eyes that were treated ≥ 7 days late revealed either new retinal fluid or an increase in existing retinal fluid in 34.4%, 38.7%, and 50.7% of the nvAMD, DME, and RVO cases, respectively.
From all eyes, 179 (19.4%) had increase in the IRF with a median treatment delay of 18 days, (IQR 7 to 42 days), longer than in eyes in which IRF decreased or remained unchanged (n = 330 eyes, median 4 days, IQR 0 to 14 days; p < 0.001). Regarding SRF, from all eyes, 83 (9.0%) had increase in the SRF with a median treatment delay of 17 days (IQR 7 to 38 days), longer than in eyes in which SRF decreased or remained unchanged (n = 112 eyes, median 7 days, IQR 0 to 22.8 days; p < 0.001).
As shown in Table 4, eyes with RVO are the most likely to develop worsening CST, MCST, and/or IRF for each 1-week delay in treatment. The odds ratio (OR) of worsening CST, MCST, IRF, and SRF, as well as the OR of overall worsening (i.e., worsening in at least one of the above four parameters), is summarized for each retinal pathology.
Discussion
The T&E protocol is commonly used to manage patients receiving intravitreal anti-VEGF therapy for retinal disease; in our clinic, we use the T&E protocol to treat patients who present with nvAMD, DME, and RVO. The premise of this approach is a proactive treatment strategy that aims to preserve a dry (i.e., fluid-free) macula using anti-VEGF treatments scheduled at intervals that are based on the individual patient’s clinical progress. Despite the popularity of this treatment approach, strikingly little data is available regarding the consequences of deviating from the recommended T&E schedule. The COVID-19 pandemic has led to a major decrease in the number of patients who can receive routine treatment and has also affected the regular IVI treatment schedule [11,12,13,14]. We therefore used data regarding treatment delays experienced during the pandemic in order to gain insight into the consequences of deviating from the recommended T&E anti-VEGF schedule in patients with nvAMD, DME, and RVO.
During the initial 8 weeks of the pandemic, more than half of our patients received treatment later than recommended, with an average delay of approximately 4 weeks. This delay in treatment may have stemmed from clinic-related factors and/or patient/pandemic-related factors; however, because our clinic remained open and IVI treatments were available during the pandemic—with no change in schedule or recommended treatment interval—we believe that this delay in treatment was likely due to patient/pandemic-related factors such as patients’ fears regarding a visit to the clinic and/or difficulties associated with traveling to the clinic. Indeed, recent studies found that during the initial weeks of the COVID-19 pandemic in 2020, attendance for IVI treatment was decreased by up to 50% compared to the same period in 2019 [11, 13, 25], with one study in France showing that the decrease in IVI was not compensated fully in the first month after the lockdown was lifted [26]. Viola et al. [12] found that older patients were less adherent to treatment, and Borrelli et al. [15] reported that the largest drop in IVI treatment adherence occurred in patients who were being treated for posterior uveitis, RVO, or DME. Interestingly, our study revealed no correlation between the treatment delay and either age or gender. This difference may be explained—at least in part—by regional differences in the prevalence of COVID-19 during the pandemic and the resulting concerns among patients [27].
Among nvAMD patients, we found a significant correlation between the number of years that the patients had received IVI treatment and length of treatment delay. Long-term follow-up studies on nvAMD patients under treatment with anti-VEGF have shown that the development of complications like atrophy and scarring is common overtime and have detrimental effects on vision [28, 29]. Thus, it is possible that those patients would likely delay treatment during the pandemic, if they felt that receiving anti-VEGF injection did not significantly improve their vision. Additionally, among nvAMD patients, we found that patients on bevacizumab had a longer delay to treatment compared to patients on aflibercept and ranibizumab. A possible explanation to this could be the fact that in Israel, approval for treatment with aflibercept and ranibizumab in cases of partial or non-response to bevacizumab needs to be approved from HMOs, using special application procedures, for the patient to benefit from a partial reimbursement over a limited number of injections. Whereas treatment with bevacizumab is usually easily approved with full reimbursement, it is possible that the extra strain and monetary investment required to get treatment with aflibercept and ranibizumab render the patients to be more conscious and compliant to treatment.
We found that delaying anti-VEGF treatment was correlated with an increase in CST, regardless of the underlying retinal pathology. Thus, the treatment delay was generally longer in the eyes in which IRF and/or SRF increased compared to eyes in which the fluid either decreased of was unchanged. These data support the importance of meticulously following the recommended T&E schedule in order to prevent increased exudate formation in nvAMD, DME, and RVO [16,17,18]. For example, Chong Teo et al. examined 286 nvAMD cases and found that timely T&E treatments resulted in a larger reduction in CST and a larger gain in VA [18]. Our results confirm these findings with respect to CST in nvAMD and extend them to include DME and RVO; similarly, previous studies have shown that missing one or more IVI treatment can result in poorer visual outcome in CRVO and DME cases [4, 22]. In addition, the nvAMD, DME, and RVO cases in our study had an increased risk of worsening for each incremental week’s delay in treatment. Thus, delays in IVI treatment should be avoided, particularly in patients with RVO-related macular edema, as we found that these cases are more likely to worsen due to such delays. Interestingly, we found that patients with RVO generally had a shorter treatment delay compared to patients with DME and patients with nvAMD. One possible explanation for this finding might be that patients with RVO may have previously experienced detrimental effects after delaying treatment and are therefore more likely to receive their scheduled injections despite the ongoing pandemic.
This study has several caveats that warrant discussion. First, the study was retrospective and did not include data regarding VA. In our clinic, to reduce patient-staff interactions, we deferred measuring VA in non-acute cases during the peak of the pandemic, unless the patient complained of a subjective decline in VA [10]. In addition, data regarding VA in the pre-lockdown visit were not available for all patients, because VA is usually measured once every 3 visits. Nevertheless, although VA data were not available for our analysis, CST and retinal fluid (IRF and/or SRF) are routinely used to guide IVI therapy in treating retinal pathologies. Moreover, an overall correlation has been reported between the change in VA and the change in macular thickness for the three retinal pathologies included in our study [2, 3, 6]. Furthermore, Evans et al. [30] examined 1731 eyes with nvAMD in the CATT (Comparisons of Age-Related Macular Degeneration Treatments Trials) study and IVAN (Inhibition of VEGF in Age-related Choroidal Neovascularisation) trial and found that eyes with a large change in retinal thickness had worse best-corrected VA. Recently, Song et al. [31] reported the visual consequences of delaying anti-VEGF therapy in 376 eyes by an average of approximately 5 weeks. The authors found that delaying therapy was more common among older patients and was associated with lower VA, DME, and PDR; moreover, they found that patients who missed a treatment had a larger loss of vision compared to patients who received their scheduled treatment [31]. Thus, our finding that delaying treatment is associated with increased macular thickness suggests that delaying treatment in eyes being treated using a T&E protocol is likely associated with a decrease in VA.
Our findings highlight the importance of continuing to follow these patients closely, as lockdown measures remain a key tool for helping reduce the risk of spreading the SARS-CoV-2 virus [32], thereby continuing to affect the ability to follow the recommended IVI treatment schedule, with delays in treatment leading to negative consequences with respect to anatomical and visual outcome.
In conclusion, the COVID-19 pandemic provided an interesting test case for evaluating the putative consequences of delaying IVI treatment in patients who have nvAMD, DME, or RVO and are being treated using the T&E protocol. Importantly, we found that delaying treatment was associated with increased macular thickness and with an increase in retinal fluid in these patients; moreover, the risk of worsening outcome increased with each incremental week of delayed treatment. Taken together, these data underscore the importance of strictly adhering to the recommended treatment schedule when using the T&E protocol.
Availability of data and material
All data is availably by request.
References
Rosenfeld PJ, Brown DM, Heier JS et al (2006) Ranibizumab for neovascular age-related macular degeneration. N Engl J Med 355:1419–1431
CATT Research Group, Martin DF, Maguire MG et al (2011) Ranibizumab and bevacizumab for neovascular age-related macular degeneration. N Engl J Med 364:1897–1908
Diabetic Retinopathy Clinical Research Network, Wells JA, Glassman AR et al (2015) Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema. N Engl J Med 372:1193–1203
Brown DM, Heier JS, Clark WL et al (2013) Intravitreal aflibercept injection for macular edema secondary to central retinal vein occlusion: 1-year results from the phase 3 COPERNICUS study. Am J Ophthalmol 155:429-437.e7
Heier JS, Campochiaro PA, Yau L et al (2012) Ranibizumab for macular edema due to retinal vein occlusions: long-term follow-up in the HORIZON trial. Ophthalmology 119:802–809
Schmidt-Erfurth U, Lang GE, Holz FG et al (2014) Three-year outcomes of individualized ranibizumab treatment in patients with diabetic macular edema: the RESTORE extension study. Ophthalmology 121:1045–1053
Prünte C, Fajnkuchen F, Mahmood S et al (2016) Ranibizumab 0.5 mg treat-and-extend regimen for diabetic macular oedema: the RETAIN study. Br J Ophthalmol 100:787–795
Engelbert M, Zweifel SA, Freund KB (2010) Long-term follow-up for type 1 (subretinal pigment epithelium) neovascularization using a modified “treat and extend” dosing regimen of intravitreal antivascular endothelial growth factor therapy. Retina 30:1368–1375
Silva R, Berta A, Larsen M et al (2018) Treat-and-extend versus monthly regimen in neovascular age-related macular degeneration: results with ranibizumab from the TREND Study. Ophthalmology 125:57–65
Safadi K, Kruger JM, Chowers I et al (2020) Ophthalmology practice during the COVID-19 pandemic. BMJ Open Ophthalmol 5:e000487
Wasser LM, Weill Y, Brosh K et al (2020) The impact of COVID-19 on intravitreal injection compliance. SN Compr Clin Med 28:1–4
Viola F, Milella P, Pozzo Giuffrida F et al (2021) Impact of coronavirus disease pandemic on intravitreal injections treatment for macular diseases: Report From a Referral Hospital in Milan. Retina 41:701–705
Xu D, Starr MR, Boucher N et al (2020) Real-world vitreoretinal practice patterns during the 2020 COVID-19 pandemic: a nationwide, aggregated health record analysis. Curr Opin Ophthalmol 31:427–434
Saleh OA, Jammal H, Alqudah N et al (2020) Clinical experience in the administration of intravitreal injection therapy at a tertiary university hospital in Jordan during the COVID-19 lockdown. Clin Ophthalmol 14:2473–2480
Borrelli E, Grosso D, Vella G et al (2020) Impact of COVID-19 on outpatient visits and intravitreal treatments in a referral retina unit: let’s be ready for a plausible “rebound effect.” Graefes Arch Clin Exp Ophthalmol 258:2655–2660
Lanzetta P, Cruess AF, Cohen SY et al (2018) Predictors of visual outcomes in patients with neovascular age-related macular degeneration treated with anti-vascular endothelial growth factor therapy: post hoc analysis of the VIEW studies. Acta Ophthalmol 96:e911–e918
Nguyen V, Vaze A, Fraser-Bell S et al (2019) Outcomes of suspending VEGF inhibitors for neovascular age-related macular degeneration when lesions have been inactive for 3 months. Ophthalmol Retina 3:623–628
Chong Teo KY, Saxena N, Gan A et al (2020) Detrimental effect of delayed re-treatment of active disease on outcomes in neovascular age-related macular degeneration: the RAMPS study. Ophthalmol Retina 4:871–880
Wickremasinghe SS, Janakan V, Sandhu SS et al (2016) Implication of recurrent or retained fluid on optical coherence tomography for visual acuity during active treatment of neovascular age-related macular degeneration with a treat and extend protocol. Retina 36:1331–1339
Bressler NM, Beaulieu WT, Glassman AR et al (2018) Persistent macular thickening following intravitreous aflibercept, bevacizumab, or ranibizumab for central-involved diabetic macular edema with vision impairment: a secondary analysis of a randomized clinical trial. JAMA Ophthalmol 136:257–269
Weiss M, Sim DA, Herold T et al (2018) Compliance and adherence of patients with diabetic macular edema to intravitreal anti-vascular endothelial growth factor therapy in daily practice. Retina 38:2293–2300
Bressler NM, Edwards AR, Antoszyk AN et al (2008) Retinal thickness on Stratus optical coherence tomography in people with diabetes and minimal or no diabetic retinopathy. Am J Ophthalmol 145:894–901
Guymer RH, Markey CM, McAllister IL et al (2019) Tolerating subretinal fluid in neovascular age-related macular degeneration treated with ranibizumab using a treat-and-extend regimen: FLUID study 24-month results. Ophthalmology 126:723–734
Wells JA, Glassman AR, Jampol LM et al (2016) Association of baseline visual acuity and retinal thickness with 1-year efficacy of aflibercept, bevacizumab, and ranibizumab for diabetic macular edema. JAMA Ophthalmol 134:127–134
Centers for Disease Control and Prevention (2020) People who are at higher risk for severe illness. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html. Accessed 26 August 2020.
Billioti de Gage S, Drouin J, Desplas D et al (2021) Intravitreal anti-vascular endothelial growth factor use in France during the coronavirus disease 2019 pandemic. JAMA Ophthalmol 139:240–242
World Health Organization (WHO) (2020) Coronavirus disease (COVID-19) situation report – 198. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200805-COVID-19-sitrep-198.pdf?sfvrsn=f99d1754_2 Accessed 11 September 2020.
Vofo BN, Beykin G, Levy J, Chowers I (2021) Long-term outcome of neovascular age-related macular degeneration: association between treatment outcome and major risk alleles. Br J Ophthalmol. https://doi.org/10.1136/bjophthalmol-2021-319054. Epub ahead of print.
Chandra S, Arpa C, Menon D et al (2020) Ten-year outcomes of antivascular endothelial growth factor therapy in neovascular age-related macular degeneration. Eye 34:1888–1896
Evans RN, Reeves BC, Maguire MG et al (2020) Associations of variation in retinal thickness with visual acuity and anatomic outcomes in eyes with neovascular age-related macular degeneration lesions treated with anti-vascular endothelial growth factor agents. JAMA Ophthalmol 138:1043–1051
Song W, Singh RP, Rachitskaya AV (2021) The effect of delay in care among patients requiring intravitreal injections. Ophthalmol Retina 5:975–980
Verma BK, Verma M, Verma VK et al (2020) Global lockdown: an effective safeguard in responding to the threat of COVID-19. J Eval Clin Pract 26:1592–1598
Acknowledgements
This work was supported by an Israel Science Foundation grant (#3485/19).
Funding
This work was supported by an Israel Science Foundation grant (#3485/19). This funding organization had no role in the design or conduct of this research. Ministry of Science and Technology,Israel,Israel Science Foundation 3485/19,Jaime Levy
Author information
Authors and Affiliations
Contributions
Research design (Navarrete Ana, Levy Jaime, Chowers Itay), Data acquisition (Navarrete Ana, Matos Katherine, Rivera Antonio, Levy Jaime, Chowers Itay), Data analysis and/or interpretation (Navarrete Ana, Vofo Brice, Levy Jaime, Chowers Itay), Manuscript preparation (Navarrete Ana, Vofo Brice, Levy Jaime, Chowers Itay).
Corresponding author
Ethics declarations
Ethics approval
The study was approved by our institutional ethics committee and conducted in adherence to the tenets of the Declaration of Helsinki. Informed consent was not required.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest/Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Navarrete, A., Vofo, B., Matos, K. et al. The detrimental effects of delayed intravitreal anti-VEGF therapy for treating retinal pathology: lessons from a forced test-case. Graefes Arch Clin Exp Ophthalmol 260, 2201–2208 (2022). https://doi.org/10.1007/s00417-021-05549-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-021-05549-7