Abstract
Purpose
To compare the degree of postoperative medial rectus (MR) muscle misalignment in patients who underwent medial orbital wall decompression with or without a periosteal flap along the MR muscle.
Methods
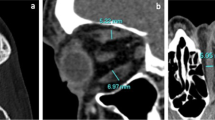
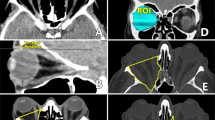
This retrospective, observational study included 40 sides from 26 patients. The following parameters were measured on axial computed tomographic images taken post- and/or preoperatively: the distance of the anteroposterior line between the posterior lacrimal crest and the junction of the ethmoid and sphenoid sinuses from the most medial point of the medial margin of the MR muscle; the angle created at the point of the MR globe insertion, the most medial point of the MR muscle, and the junction of the ethmoid and sphenoid sinuses; and the MR muscle cross-sectional area. Postoperative changes in the distance (MR muscle shift) and area (MR muscle expansion) were calculated, and MR muscle shift, MR muscle angle, and the rate of MR muscle expansion were compared between the groups with (22 sides) and without (18 sides) a periosteal flap.
Results
MR muscle shift (P = 0.325), MR muscle angle (P = 0.219), and the rate of MR muscle expansion (P = 0.904) were not significantly different between the groups.
Conclusions
Preservation of the periosteum along the MR muscle is thought to prevent MR muscle misalignment after medial orbital wall decompression. However, the results of this study indicate that preservation of a periosteal flap may not contribute to lessening MR muscle shift after surgery.


Similar content being viewed by others
Data availability
All data are included in this paper.
Code availability
N/A.
References
Rootman DB (2018) Orbital decompression for thyroid eye disease. Surv Ophthalmol 63:86–104
Oeverhaus M, Copei A, Mattheis S, Ringelstein A, Tiemessen M, Esser J, Eckstein A, Stähr K (2019) Influence of orbital morphology on proptosis reduction and ocular motility after decompression surgery in patients with Graves’ orbitopathy. PLoS One 14:e0218701
Abràmoff MD, Kalmann R, de Graaf MEL, Stilma JS, Mourits MP (2002) Rectus extraocular muscle paths and decompression surgery for Graves orbitopathy: mechanism of motility disturbances. Invest Ophthalmol Vis Sci 43:300–307
Alsuhaibani AH, Carter KD, Policeni B, Nerad JA (2011) Effect of orbital bony decompression for Graves’ orbitopathy on the volume of extraocular muscles. Br J Ophthalmol 95:1255–1258
Gupta A, Nobori A, Wang Y, Rootman D, Goldberg R (2018) Lateral rectus muscle expands more than medial rectus following maximal deep balanced orbital decompression. Ophthalmic Plast Reconstr Surg 34:140–142
Platt MP, Metson R (2009) Endoscopic management of exophthalmos. Facial Plast Surg 25:38–42
Metson R, Samaha M (2002) Reduction of diplopia following endoscopic orbital decompression: the orbital sling technique. Laryngoscope 112:1753–1757
Hill RH, Czyz CN, Bersani TA (2012) Transcaruncular medial wall decompression: an effective approach for patients with unilateral Graves ophthalmopathy. Scientific World J 2012:312361
Nishimura K, Takahashi Y, Katahira N, Uchida Y, Ueda H, Ogawa T (2019) Visual changes after transnasal endoscopic versus transcaruncular medial orbital wall decompression for dysthyroid optic neuropathy. Auris Nasus Larynx 46:876–881
Vaidya A, Kakizaki H, Takahashi Y (2021) Changes in field of binocular single vision and medial ocular deviation angle after balanced orbital decompression. Ophthalmic Plast Reconstr Surg 37:154–160
Stähr K, Eckstein A, Buschmeier M, Hussain T, Daser A, Oeverhaus M, Lang S, Mattheis S (2021) (in press) Risk factors for new onset diplopia after graduated orbital decompression. Ophthalmic Plast Reconstr Surg x. https://doi.org/10.1097/IOP.0000000000001949
Goldberg RA, Shorr N, Cohen MS (1992) The medial strut in the prevention of postdecompression dystopia in dysthyroid ophthalmopathy. Ophthal Plast Reconstr Surg 8:32–34
Jefferis JM, Jones RK, Currie ZI, Tan JH, Salvi SM (2018) Orbital decompression for thyroid eye disease: methods, outcomes, and complications. Eye 32:626–636
Graham SM, Brown CL, Carter KD, Song A, Nerad JA (2003) Medial and lateral orbital wall surgery for balanced decompression in thyroid eye disease. Laryngoscope 113:1206–1209
Seiff SR, Tovilla JL, Carter SR, Choo PH (2000) Modified orbital decompression for dysthyroid orbitopathy. Ophthalmic Plast Reconstr Surg 16:62–66
Mainville NP, Jordan DR (2014) Effect of orbital decompression on diplopia in thyroid-related orbitopathy. Ophthalmic Plast Reconstr Surg 30:137–140
May A, Zubcov A, Fries U, Reimold I, Weber A (2001) Ancillary procedures in microscopic endonasal orbital decompression for thyroid-associated ophthalmopathy. ORL 63:137–140
Vaidya A, Lee PAL, Kitaguchi Y, Kakizaki H, Takahashi Y (2020) Spontaneous orbital decompression in thyroid eye disease: new measurement methods and its influential factors. Graefes Arch Clin Exp Ophthalmol 258:2321–2329
Lee PAL, Vaidya A, Kono S, Kakizaki H, Takahashi Y (2021) (in press) Extraocular muscle expansion after deep lateral orbital wall decompression: influence on proptosis reduction and its predictive factors. Graefes Arch Clin Exp Ophthalmol: https://doi.org/10.1007/s00417-021-05286-x
Koornneef L (1977) New insights in the human orbital connective tissue: result of a new anatomical approach. Arch Ophthalmol 95:1269–1273
Kamisasanuki T, Katori N, Kasai K, Hayashi K, Kokubo K, Ota Y, Sakamoto T (2014) Adhesiotomy with grafting of fat and perifascial areolar tissue for adhesions of extraocular muscles after trauma or surgery. Graefes Arch Clin Exp Ophthalmol 252:829–836
Kang H, Takahashi Y, Nakano T, Asamoto K, Ikeda H, Kakizaki H (2015) Medial canthal support structures: the medial retinaculum: a review. Ann Plast Surg 74:508–514
Ettl A, Priglinger S, Kramer J, Koornneef L (1996) Functional anatomy of the levator palpebrae superioris muscle and its connective tissue system. Br J Ophthalmol 80:702–707
Ana-Magadia MG, Valencia MRP, Naito M, Nakano T, Miyazaki H, Kakizaki H, Takahashi Y (2020) Location of the myoneural junction of the inferior oblique muscle: an anatomic study. Ann Anat 227:151429
Author information
Authors and Affiliations
Contributions
QueryAll the authors qualify for authorship based on contributions to the conception and design (YT), acquisition of data (YT), literature search (YT), and analyses and interpretation of data (all authors). All the authors contributed to drafting the article and revising it critically for important intellectual content and final approval of the version to be published.
Other contributors
No one contributed to the work who did not meet our authorship criteria.
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Institutional Review Board (IRB) of Aichi Medical University Hospital (approval No, 2019–034) and followed the tenets of the 1964 Declaration of Helsinki.
Consent to participate
The IRB granted a waiver of informed consent for this study based on the ethical guidelines for medical and health research involving human subjects established by the Japanese Ministry of Education, Culture, Sports, Science, and Technology and the Ministry of Health, Labour, and Welfare. The waiver was granted because the study was a retrospective chart review, not an interventional study, and because it was difficult to obtain consent from patients who had been treated several years prior to the study. Nevertheless, at the request of the IRB, we published an outline of the study, which is available for public viewing on the Aichi Medical University Hospital website. This public posting also allowed patients the opportunity to decline participation, although none of the patients did so. Personal identifiers were removed from all records before data analysis.
Consent for publication
All the authors agreed with publication of this paper.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Takahashi, Y., Vaidya, A., Yo, K. et al. Comparison of degree of medial rectus muscle misalignment after medial orbital wall decompression with or without periosteal flap. Graefes Arch Clin Exp Ophthalmol 260, 1025–1031 (2022). https://doi.org/10.1007/s00417-021-05413-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-021-05413-8