Abstract
Purpose
To evaluate spontaneous decompression of the medial orbital wall and orbital floor in thyroid eye disease using new measurement methods and to analyze the influential factors.
Methods
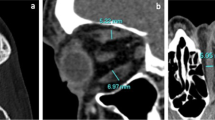
This retrospective study included 86 patients (172 sides). Regarding evaluation of spontaneous medial orbital decompression, an anteroposterior line was drawn between the posterior lacrimal crest and the junction between the ethmoid bone and corpus ossis sphenoidalis. The bulged and/or dented areas from that line were measured. Regarding evaluation of spontaneous orbital floor decompression, the length of the perpendicular distance from a line that was drawn between the inferior orbital rim and the orbital process of palatal bone to the tip of the superior bulge of the orbital floor was measured.
Results
Multivariate linear regression analysis revealed that the maximum cross-sectional areas of the superior rectus/levator palpebrae superioris complex (P = 0.020) and medial rectus muscle (P = 0.028) were influential factors for spontaneous decompression of medial orbital wall (adjusted r2 = 0.090; P < 0.001), whereas the number of cycles of steroid pulse therapy (P = 0.002) and the maximum cross-sectional area of the inferior rectus muscle (P = 0.007) were the ones for that of the orbital floor (adjusted r2 = 0.096; P < 0.001).
Conclusion
We believe that the identification of multiple influential factors of spontaneous decompression of the medial orbital wall and orbital floor will be helpful for better understanding and planned management of thyroid eye disease patients undergoing orbital decompression surgery.


Similar content being viewed by others
Data availability
All data are included in this report.
References
Kang EM, Yoon JS (2015) Clinical and radiological characteristics of Graves’ orbitopathy patients showing spontaneous decompression. J Craniomaxillofac Surg 43:48–52
Kahaly GJ (2001) Imaging in thyroid-associated orbitopathy. Eur J Endocrinol 145:107–118
Tan NYQ, Leong YY, Lang SS, Htoon ZM, Young SM, Sunder G (2017) Radiologic parameters of orbital bone remodeling in thyroid eye disease. Invest Ophthalmol Vis Sci 58:2527–2533
Bhermi GS, Gauba V, Brittain P (2006) Spontaneous bony orbital auto-decompression in thyroid ophthalmopathy. Orbit 25:123–125
Weis E, Heran MK, Jhamb A, Chan AK, Chiu JP, Hurley MC, Rootman J (2012) Quantitative computed tomographic predictors of compressive optic neuropathy in patients with thyroid orbitopathy: a volumetric analysis. Ophthalmology 119:2174–2178
Chan LL, Tan HE, Fook-Chong S, Teo TH, Lim LH, Seah LL (2009) Graves ophthalmopathy: the bony orbit in optic neuropathy, its apical angular capacity, and impact on prediction of risk. Am J Neuroradiol 30:597–602
Detorakis ET (2014) Spontaneous medial orbital decompression associated with medial wall remodeling in Graves’ orbitopathy. Ophthalmic Plast Reconstr Surg 30:79–80
Bokman CL, Ugradar S, Rootman DB (2018) Measurement of medial wall bowing and clinical associations in thyroid eye disease. Ophthalmic Plast Reconstr Surg 34:557–559
Kashkouli MB, Pakdel F (2010) Spontaneous orbital floor fracture in thyroid eye disease. Ophthalmic Plast Reconstr Surg 26:301–302
Blandford AD, Zhang D, Chundury RV, Perry JD (2017) Dysthyroid optic neuropathy: update on pathogenesis, diagnosis, and management. Expert Rev Ophthalmol 12:111–121
Takahashi Y, Nakano T, Miyazaki H, Kakizaki H (2016) An anatomical study of the orbital floor in relation to the infraorbital groove: implications of predisposition to orbital floor fracture site. Graefes Arch Clin Exp Ophthalmol 254:2049–2055
Sabundayo MS, Kakizaki H, Takahashi Y (2018) Normative measurements of inferior oblique muscle thickness in Japanese by magnetic resonance imaging using a new technique. Graefes Arch Clin Exp Ophthalmol 256:839–844
Murakami Y, Kanamoto T, Tuboi T, Maeda T, Inoue Y (2001) Evaluation of extraocular muscle enlargement in dysthyroid ophthalmopathy. Jpn J Ophthalmol 45:622–627
Valencia MRP, Miyazaki H, Kakizaki H, Takahashi Y (2020) Thickness of retro- and sub-orbicularis oculi fat in thyroid eye disease: comparison with controls and its influential factors. Ophthalmic Plast Reconstr Surg. https://doi.org/10.1097/IOP.0000000000001597
Song WK, Lew H, Yoon JS, Oh MJ, Lee SY (2009) Role of medial orbital wall morphologic properties in orbital blow-out fractures. Invest Ophthalmol Vis Sci 50:495–499
Takahashi Y, Nakakura S, Sabundayo MS, Kitaguchi Y, Miyazaki H, Mito H, Kakizaki H (2018) Differences in common orbital blowout fracture sites by age. Plast Reconstr Surg 141:893e–901e
Haugeberg G, Griffiths B, Sokoll KB, Emery P (2004) Bone loss in patients treated with pulses of methylprednisolone is not negligible: a short term prospective observational study. Ann Rheum Dis 63:940–944
LoCascio V, Bonucci E, Imbimbo B, Ballanti P, Adami S, Milani S, Tartarotti D, DellaRocca C (1990) Bone loss in response to long-term glucocorticoid therapy. Bone Miner 8:39–51
Abrahamsen B, Jørgensen HL, Laulund AS, Nybo M, Bauer DC, Brix TH, Hegedüs L (2015) The excess risk of major osteoporotic fractures in hypothyroidism is driven by cumulative hyperthyroid as opposed to hypothyroid time: an observational register-based time-resolved cohort analysis. J Bone Miner Res 30:898–905
Vestergaard P, Rejnmark L, Mosekilde L (2005) Influence of hyper- and hypothyroidism, and the effects of treatment with antithyroid drugs and levothyroxine on fracture risk. Calcif Tissue Int 77:139–144
Vestergaard P, Mosekilde L (2003) Hyperthyroidism, bone mineral, and fracture risk—a meta-analysis. Thyroid 13:585–593
Ana-Magadia MG, Valencia MRP, Naito M, Nakano T, Miyazaki H, Kakizaki H, Takahashi Y (2020) Location of the myoneural junction of the inferior oblique muscle: an anatomic study. Ann Anat 227:151429
Kakutani S, Ito M, Kakizaki H, Takahashi Y (in press) Orbital decompression for exorbitism and exophthalmos in a patient with thyroid eye disease. J Craniofac Surg in press
Author information
Authors and Affiliations
Contributions
All authors qualify for authorship based on contributions to the conception and design (YT), acquisition of data (YT), statistical analysis (YK and YT), literature search (AV and YT), and interpretation of data (all authors). All authors contributed to drafting the article and revising it critically for important intellectual content and final approval of the version to be published. No one contributed to the work who did not meet our authorship criteria.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
This study was approved by the Institutional Review Board (IRB) of our institution (Aichi Medical University Hospital, approval No. 2019-175) and followed the tenets of the 1964 Declaration of Helsinki.
Consent to participate
The IRB granted a waiver of informed consent for this study on the basis of the ethical guidelines for medical and health research involving human subjects established by the Japanese Ministry of Education, Culture, Sports, Science, and Technology and the Ministry of Health, Labour, and Welfare. The waiver was granted because the study was a retrospective review and not an interventional study and because it was difficult to obtain consent from patients who had been treated several years prior to this study. Nevertheless, at the request of the IRB, an outline of the study was published on the website of our institution and this was made available for public viewing. This public posting also gave patients an opportunity to decline participation, although no refusal was made known to us. Personal identifiers were removed from the records prior to data analysis.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vaidya, A., Lee, P.A.L., Kitaguchi, Y. et al. Spontaneous orbital decompression in thyroid eye disease: new measurement methods and its influential factors. Graefes Arch Clin Exp Ophthalmol 258, 2321–2329 (2020). https://doi.org/10.1007/s00417-020-04762-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-020-04762-0