Abstract
Purpose
Complicated retinal re-detachment with inferior proliferative vitreoretinopathy (PVR) remains a challenge. This study’s aim was to compare vitrectomy with conventional silicon oil (CSO) combined with an encircling band (EB) and vitrectomy with heavy silicon oil (HSO) alone to treat retinal re-detachment through inferior PVR, where standard procedures have already failed.
Methods
A retrospective analysis was done on patients with inferior complex re-detachment with secondary PVR after primary surgery, who received pars plana vitrectomy (PPV) with CSO combined with EB (group 1) or PPV alone with HSO (group 2) between December 2006 and August 2017. The primary endpoint was retinal reattachment, and the secondary endpoint was visual acuity (VA) change and complications in both groups.
Results
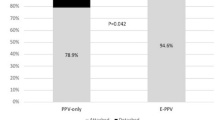
This study included 119 eyes. Total single surgery anatomical success (SSAS) was 64%, with 80% (52/65) achieved in group 1 and 44.5% (24/54) in group 2 (p < 0.0001). The total final anatomical success (FAS) rate was 79% (94/119). In group 1, FAS was 91% (59/65) compared with 65% (35/54) in group 2 (p = 0.003). The pretreatment VA of group 1 had a median of 1.4 logMAR (95% CI 0.3–1.8), and group 2 showed a median of 1.4 logMAR (95% CI 0.2–1.8). The post-treatment decrease in group 1 was a median equal to − 0.6 versus − 0.1 for group 2 (p = 0.0001). Serious complications were similar in both groups.
Conclusion
For complicated retinal re-detachment through inferior PVR, the combination of PPV with EB may lead to better anatomical (SSAS, FAS) and functional success compared with PPV alone with HSO.
Similar content being viewed by others
Availability of data
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
References
Pastor JC, Rojas J, Pastor-Idoate S, Di Lauro S, Gonzalez-Buendia L, Delgado-Tirado S (2016) Proliferative vitreoretinopathy: a new concept of disease pathogenesis and practical consequences. Prog Retin Eye Res 51:125–155
Pastor JC, de la Rúa ER, Martín F (2002) Proliferative vitreoretinopathy: risk factors and pathobiology. Prog Retin Eye Res 21(1):127–144
Choudhary MM, Choudhary MM, Saeed MU, Ali A (2012) Removal of silicone oil: prognostic factors and incidence of retinal re-detachment. Retina 32(10):2034–2038
Sandner D, Herbrig E, Engelmann K (2007) High-density silicone oil (Densiron) as a primary intraocular tamponade: 12-month follow up. Graefes Arch Clin Exp Ophthalmol 245:1097–1105
Stappler T, Heimann H, Wong D, Gibran SK, Groenewald C, Pearce IA (2008) Heavy tamponade 2 Densiron 68® in routine clinical practice: anatomical and functional outcomes of a consecutive case series. Eye (Lond) 22:1360–1365
Wickham L, Tranos P, Hiscott P, Charteris D (2010) The use of silicone oil-RMN3 (Oxane HD) as heavier-than-water internal tamponade in complicated inferior retinal detachment surgery. Graefes Arch Clin Exp Ophthalmol 248:1225–1231
Joussen AM, Rizzo S, Kirchhof B, Schrage N, Li X, Lente C, Hilgers RD, HSO -Study Group (2011) Heavy silicone oil versus standard silicone oil in as vitreous tamponade in inferior PVR (HSO Study): interim analysis. Acta Ophthalmol 89(6):483–489
Bottoni F, Sborgia M, Arpa P, De Casa N, Bertazzi E, Monticelli M, De Molfetta V (1993) Perfluorocarbon liquids as postoperative short-term vitreous substitutes in complicated retinal detachment. Graefes Arch Clin Exp Ophthalmol 231(11):619–628
Gremillion CM Jr, Peyman GA, Liu KR, Naguib KS (1990) Fluorosilicone oil in the treatment of retinal detachment. Br J Ophthalmol 74(11):643–646
Wolf S, Schön V, Meier P, Wiedemann P (2003) Silicone oil-RMN3 mixture (“heavy silicone oil”) as internal tamponade for complicated retinal detachment. Retina 23:335–342
Wong D, Van Meurs JC, Stappler T, Groenewald C, Pearce IA, McGalliard JN, Manousakis E, Herbert EN (2005) A pilot study on the use of a perfluorohexyloctane/silicone oil solution as a heavier than water internal tamponade agent. Br J Ophthalmol 89:662–665
Theelen T, Tilanus MA, Klevering BJ (2004) Intraocular inflammation following endotamponade with high-density silicone oil. Graefes Arch Clin Exp Ophthalmol 242:617–620
Rizzo S, Genovesi-Ebert F, Vento A, Cresti F, Di Bartolo E, Belting C (2007) A new heavy silicone oil (HWS 46-3000) used as a prolonged internal tamponade agent in complicated vitreoretinal surgery: a pilot study. Retina 27:613–620
Rizzo S, Genovesi-Ebert F, Belting C, Vento A, Cresti F (2005) A pilot study on the use of silicone oil-RMN3 as heavier-than-water endotamponade agent. Graefes Arch Clin Exp Ophthalmol 243:1153–1157
Ziemssen F, Bartz-Schmidt KU (2004) Vitrectomy with or without cerclage in the treatment of retinal detachment. Ophthalmologe 101:554–562
Walter P, Hellmich M, Baumgarten S, Schiller P, Limburg E, Agostini H, Pielen A, Helbig H, Lommatzsch A, Rössler G, Mazinani B, VIPER Study Group (2017) Vitrectomy with and without encircling band for pseudophakic retinal detachment: VIPER Study Report No 2-main results. Br J Ophthalmol 101:712–718
Kinori M, Moisseiev E, Shoshany N, Fabian ID, Skaat A, Barak A, Loewenstein A, Moisseiev J (2011) Comparison of pars plana vitrectomy with and without scleral buckle for the repair of primary rhegmatogenous retinal detachment. Am J Ophthalmol 152:291–297
Weichel ED, Martidis A, Fineman MS, McNamara JA, Park CH, Vander JF, Ho AC, Brown GC (2006) Pars plana vitrectomy versus combined pars plana vitrectomy-scleral buckle for primary repair of pseudophakic retinal detachment. Ophthalmology 113:2033–2040
Ambati J, Arroyo JG (2000) Postoperative complications of scleral buckling surgery. Int Ophthalmol Clin 40:175–185
Farr AK, Guyton DL (2000) Strabismus after retinal detachment surgery. Curr Opin Ophthalmol 11:207–210
Hayreh SS, Scott WE (1979) Anterior segment ischemia following retinal detachment surgery. Mod Probl Ophthalmol 20:148–153
Nguyen QD, Lashkari K, Hirose T, Pruett RC, McMeel JW, Schepens CL (2001) Erosion and intrusion of silicone rubber scleral buckle. Presentation and management. Retina 21:214–220
Hilton G, Machemer R, Michels R, Okun E, Schepens C, Schwartz A (1983) The classification of retinal detachment with proliferative vitreoretinopathy. Ophthalmology 90:121–125
Desai UR, Strassman IB (1997) Combined pars plana vitrectomy and scleral buckling for pseudophakic and aphakic retinal detachments in which a break is not seen preoperatively. Ophthalmic Surg Lasers 28:718–722
Stangos AN, Petropoulos IK, Brozou CG, Kapetanios AD, Whatham A, Pournaras CJ (2004) Pars-plana vitrectomy alone vs vitrectomy with scleral buckling for primary rhegmatogenous pseudophakic retinal detachment. Am J Ophthalmol 138:952–958
Wickham L, Connor M, Aylward GW (2004) Vitrectomy and gas for inferior break retinal detachments: are the results comparable to vitrectomy, gas, and scleral buckle? Br J Ophthalmol 88:1376–1379
Storey P, Alshareef R, Khuthaila M, London N, Leiby B, DeCroos C, Kaiser R, Wills PVR Study Group (2014) Pars plana vitrectomy and scleral buckle versus pars plana vitrectomy alone for patients with rhegmatogenous retinal detachment at high risk for proliferative vitreoretinopathy. Retina 34:1945–1951
Mancino R, Aiello F, Ciuffoletti E, Di Carlo E, Cerulli A, Nucci C (2015) Inferior retinotomy and silicone oil tamponade for recurrent inferior retinaldetachment and grade C PVR in eyes previously treated with pars plana vitrectomy or scleral buckle. BMC Ophthalmol 15:173
Velikay-Parel M, Kiss CG, Ivastinovic D, Richter-Mueksch S (2011) Encircling band, laser retinopexy and lens removal as standard procedure in complicated retinal detachment shows a good clinical outcome. Acta Ophthalmol 89:629–633
Abu Eleinen KG, Mohalhal AA, Ghalwash DA, Abdel-Kader AA, Ghalwash AA, Mohalhal IA, Abdullatif AM (2018) Vitrectomy with scleral buckling versus with inferior retinectomy in treating primary rhegmatogenous retinal detachment with PVR and inferior breaks. Eye (Lond) 32:1839–1844
Boscia F, Furino C, Recchimurzo N, Besozzi G, Sborgia G, Sborgia C (2008) Oxane HD vs silicone oil and scleral buckle in retinal detachment with proliferative vitreoretinopathy and inferior retinal breaks. Graefes Arch Clin Exp Ophthalmol 246:943–948
Sheng Y, Sun W, Mo B, Yu YJ, Gu YS, Liu W (2012) Non-buckled vitrectomy for retinal detachment with inferior breaks and proliferative vitreoretinophathy. Int J Ophthalmol 5:591–595
Tan HS, Mura M, Oberstein SY, de Smet MD (2010) Primary retinectomy in proliferative vitreoretinopathy. Am J Ophthalmol 149:447–452
Auriol S, Pagot-Mathis V, Mahieu L, Lemoine C, Mathis A (2008) Efficacy and safety of heavy silicone oil Densiron 68 in the treatment of complicated retinaldetachment with large inferior retinectomy. Graefes Arch Clin Exp Ophthalmol 246:1383–1389
Joussen AM, Wong D (2008) The concept of heavy tamponades-chances and limitations. Graefes Arch Clin Exp Ophthalmol 246:1217–1224
Rizzo S, Romagnoli MC, Genovesi-Ebert F, Belting C (2011) Surgical results of heavy silicone oil HWS-45 3000 as internal tamponade for inferior retinal detachment with PVR: a pilot study. Graefes Arch Clin Exp Ophthalmol 249:361–367
Heimann H, Stappler T, Wong D (2008) Heavy tamponade 1: a review of indications, use, and complications. Eye (Lond) 22:1342–1359
Kirchhof B, Wong D, Van Meurs J, Hilgers RD, Macek M, Lois N, Schrage NF (2002) Use of perfluorohexyloctane as a long-term internal tamponade agent in complicated retinal detachment surgery. Am J Ophthalmol 133:95–101
Roider J, Hoerauf H, Kobuch K, Gabel VP (2002) Clinical findings on the use of long-term heavy tamponades (semifluorinated alkanes and their oligomers) in complicated retinal detachment surgery. Graefes Arch Clin Exp Ophthalmol 240:965–971
Hoerauf H, Roider J, Kobuch K, Laqua H (2005) Perfluorohexylethan (O62) as ocular endotamponade in complex vitreoretinal surgery. Retina 25:479–488
Tognetto D, Minutola D, Sanguinetti G, Ravalico G (2005) Anatomical and functional outcomes after heavy silicone oil tamponade in vitreoretinal surgery for complicated retinal detachment: a pilot study. Ophthalmology 112:1574
Murchison A, Feldman BH, Wilkinson CP, Karth PA (2019) Scleral buckling for rhegmatogenous retinal detachment. American Academy of Ophthalmology. https://eyewiki.aao.org/Scleral_buckling_for_rhegmatogenous_retinal_detachment. Accessed 08 July 2020
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Measurements and data collection were performed by Dimopoulos, Bartz-Schmidt, and Ziemssen. Data analysis was performed by Dimopoulos Williams and Voykov. The first draft of the manuscript was written Dimopoulos, Ziemssen, and Leitritz. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest
Ethics approval
Approval was obtained from the local ethics committee (University Hospital Tübingen, Project Number (122/2020BO2).
Consent to participate
Not applicable due to the retrospective and anonymous character of our database analysis.
Consent for publication
No photographs of persons were submitted.
Code availability
Not applicable
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dimopoulos, S., William, A., Voykov, B. et al. Results of different strategies to manage complicated retinal re-detachment. Graefes Arch Clin Exp Ophthalmol 259, 335–341 (2021). https://doi.org/10.1007/s00417-020-04923-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-020-04923-1