Abstract
Background
To investigate the influence of different types of retinopexy on the outcome of rhegmatogenous retinal detachment (RRD) repair.
Method
All patients with RRD who underwent pars plana vitrectomy (PPV) between January 2013 and December 2017 were included. Analysed surgical factors were types of retinopexy (cryocoagulation, endolaser, combined). Subgroup analysis was performed in patients with primary proliferative vitreoretinopathy (PVR), and/or the necessity of a primary silicone oil fill.
Results
A total of 1017 eyes with retinal detachment were included. The predominant type of retinopexy used during PPV was cryocoagulation in 492 eyes, followed by a combined cryocogulation/endolaser in 306 eyes and laserretinopexy in only 219 eyes. Overall, the re-detachment rate was 10.1%. In most of the cases (53.6%) the main reason for re-detachment was insufficient retinopexy, followed by a PVR-reaction in 37.3%, and new site break in 9.1%. No significant difference in the rate of re-detachment was found between the different types of retinopexy (p = 0.309). However, subgroup analysis showed a significantly higher rate of re-detachment in patients with a primary PVR (p = 0.0003), and in the group with silicone oil as the primary tamponade (p = 0.0001).
Conclusion
The data suggests that the type of retinopexy has little relevance for the surgical outcome of PPV for the primary RRD. However, patients with primary PVR and primary silicone oil fills were at a significantly increased risk for re-detachment.
Similar content being viewed by others
Background
Only a hundred years ago, rhegmatogenous retinal detachment (RRD) was declared untreatable at the International Congress in Paris. Since then, a few new methods have been developed [1]. Pars plana vitrectomy (PPV), which was first introduced in 1972 by Machemer, has revolutionized the treatment of RRD. Over the last few years, PPV has undergone a major technical development towards small incision vitreoretinal surgery, and has become a standard procedure for almost all types of retinal detachments [2, 3].
An integral part of the treatment of all kinds of RRD is to create a barrier around the retinal break [4, 5]. Usually, this is performed by using either cryocoagulation or endolaser. Both techniques lead through scarring to create a durable chorioretinal connection after 2–3 weeks [6,7,8]. Another crucial step in the treatment of RRD is the use of a tamponade such as gas or silicone oil until the barrier around the retinal break becomes stable [4, 6]. To date, there is limited evidence as to which type of retinopexy provides the best outcomes. However, some older studies have shown that cryotherapy can be a stimulating factor for postoperative proliferative vitreoretinopathy (PVR) [9,10,11,12].
This present study compares the retinopexy techniques regarding the surgical failure rate after PPV for rhegmatogenous retinal detachment.
Method
The study was approved by the local ethic committee(Ethikkommission Ostschweiz, Business Administration System for Ethics Committees number 2018–00104) and was performed as a part of departmental quality control. Research adhered to the tenets of the Declaration of Helsinki.
All patients with RRD who underwent PPV at the Cantonal Hospital Sankt Gallen (tertiary referral centre) between January 2013 and December 2017 were included. Patients with other types of retinal detachment, such as tractional or exsudative types, were excluded. Collected data included: demographics, side, macula involvement, PVR preoperatively, lens status (phakic, pseudophakic), type of tamponade (oil, gas), occurrence and reason for re-detachment (PVR, insufficient retinopexy, new break).
All surgeries were performed by three experienced vitreoretinal surgeons. The type of retinopexy was determined during the procedure, and was solely chosen according the surgeon’s preference. In phakic eyes, phacoemulsification and PPV were both performed in one procedure.
All patients were followed up for six months in our outpatient clinic. Thereafter, patients were referred back to the private ophthalmologist. In case of re-detachment after six months, patients were referred back to hospital for re-treatment.
Surgical technique
A standard core and peripheral 3-port PPV (23-gauge) (Stellaris, Bausch and Lomb, New York, USA) was performed for all patients. Surgery was performed under general anaesthesia. After a complete vitrectomy and the separation of posterior hyaloids with suction techniques, retina reattachment was obtained either by direct fluid-air exchange with the drainage of subretinal fluid through the main break, or by using perfluorocarbon liquid followed by fluid-air exchange. Adjuvant retinotomies were performed to achieve complete retinal reattachment, if required. Retinopexy was performed either, with transconjuctival cryocoagulation or by endolaser. The type of retinopexy was determined during the procedure and was solely chosen according the surgeon’s preference. In some eyes, both retinopexy types were applied, e.g. if additionally to a retinal break, large lattice area or if multiple breaks were present. At the end of surgery, gas (20% Sulfur hexafluoride [SF6 gas], 12% perfluoropropane [C3F8 gas]) or silicone oil tamponade was applied. The choice of intraocular tamponade depended on RRD characteristics. However, as a rule, SF6 gas was injected in case of retinal breaks located in the upper 240 retinal degrees; while C3F8 gas was injected when inferior retinal tears were present and in patients with low-compliance posture. Silicone oil tamponade were reserved for complex RRD’s, such as PVR and giant retinal tears. In phakic eyes, phacoemulsification and PPV were both performed in one procedure.
Statistical analysis
The binary outcome was whether or not retinal re-detachment occurred. The predictor of interest was the type of retinopexy. Because the rate of re-detachment is known to depend on the presence of PVR and/or the type of tamponade (silicone oil, e.g. primary silicone oil in giant retinal tears), subgroup analyses were carried out to ensure that predictor-outcome associations were not confounded by these factors. In addition, adjusted analyses were carried out to account for patient characteristics (macula status). The association between the predictor (type of retinopexy) and the outcome (re-detachment) was analysed with a chi-squared test with continuity correction, either for all patients or for the high-risk subgroups (patients with primary PVR or with primary silicone oil tamponade). Generalized linear models with binomial error distribution were used to test whether predictor-outcome associations depend on PVR or the type of tamponade. Generalized linear models were also used for adjusted analyses of associations between predictors and outcome, taking patient characteristics (macula status) into account. A power calculation was performed to demonstrate that the study is adequately powered to detect a meaningful and expected difference in re-detachment rates between the two groups (the number of patients per group needed to show a significant difference with 90% probability was n = 342). All analyses were carried out with R, version 3.3.3.
Results
Overall, 1017 consecutive eyes with RRD were included in this study. The median age at surgery was 63.2 years with a range between 15.2 and 94.5. Macula involvement occurred in 587 eyes (57.7%). Primary PVR was found in 93 eyes (9.1%) and silicone oil was used in 138 eyes (13.6%). In 492 eyes (48.4%) cryocoagulation and in 219 eyes (21.5%) endolaser only was performed. In 306 (30.1%) eyes both types of retinopexy were combined. The patient characteristics are shown in Table 1.
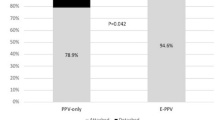
The re-detachment rate was 10.1% (103 patients). Insufficiency of the retinopexy was the main reason for re-detachment, and occurred in 53.6% of these eyes. In 37.3% of patients, PVR-reaction led to re-detachment, and in 9.1% retinal detachment occurred at a different location caused by another break. In general, there was no significant difference in the re-detachment rate between the different types of retinopexy (p = 0.309). Further analysis showed that using cryotherapy is not associated with higher rates of re-detachments caused by PVR, or by insufficient treatment of retinal breaks when compared to endolaser alone (Table 2). Subgroup analysis showed a significantly higher rate of re-detachment in patients with a primary PVR (p = 0.0003), and in the group with silicone oil as the primary tamponade (p = 0.0001). The two confounders were strongly associated with each other (X2 = 290, p < 0.0001). Further, patients with a macula-off detachment experienced a significantly higher re-detachment rate (Table 3). Nevertheless, when associations between the type of retinopexy and re-detachment were separately analysed for the high-risk groups, the results were not different from those of all patients: again, there were no significant associations between predictors and outcome (Table 4).
Discussion
Creating a sufficient barrier around the retinal break is the crucial step when performing PPV for RRD, and one of the key factors for determining the outcome [4,5,6]. Usually, this is performed by using cryocoagulation and/or endolaser. Both methods for retinopexy cause an alteration of the blood-retinal barrier, which leads to a breakdown of the barrier and freeing RPE cells, which can cause PVR [13].
PVR is the clinical syndrome associated with retinal traction and detachment in which cells with proliferative potential multiply and contract on retinal surfaces. PVR is another important factor for surgical success after retinal detachment repair. Various studies report an incidence of PVR before surgery in 5–11% of all patients with RRD [3, 14, 15] and in 50–75% of re-detachment after retinal detachment repair PVR is the cause for failure [15]. In our study population, insufficiency of the retinopexy was the main reason for re-detachment, and occurred in 53.6% of patients, followed by PVR with 37.3%. In 9.1%, retinal re-detachment occurred at a different location caused by another break, which had newly developed or was missed during the first procedure. In this study, there was no significant difference in the re-detachment rate between the different types of retinopexy (p = 0.309). Further, cryotherapy was not associated with higher rates of re-detachments caused by PVR.
In both techniques, there is a reduction in adhesive strength in the first week caused by chorioretinal edema and cellular infiltration [6,7,8]. Until a sufficient adhesion is achieved, usually 2–3 weeks after surgery, a tamponade is required. Young et al. showed in an experimental study with rabbit retina that the adhesive force after photocoagulation was reduced 50% at 8 h, but increased beyond normal by 24 h, and remained twice normal between 3 days and 4 weeks [8]. The tamponade agents displace the preretinal and subretinal fluid away from retinal breaks and appose the retina in the underlying retinal pigment epithelium [16, 17]. Despite not reaching statistical significance, patients treated with cryotherapy had a tendency to have more insufficiency in the retinopexy and suffer from re-detachments caused by a new or missed break (Table 3). From our experience, most of the re-detachments caused by insufficiently treated breaks are not because of under- but rather due to overtreatment of the retinal break producing atrophic scars. A new type of retinopexy, such as high-frequency electric welding, shows promising results by creating an immediate chorioretinal adhesion, which could make the usage of tamponade obsolete [6].
The data suggests that the type of retinopexy has little relevance for the surgical outcome of PPV for the primary RRD. The only risk factors that contribute to a higher re-detachment rate in our study were the primary PVR and the primary use of silicone oil tamponade, and these two risk factors are highly associated with each other. Further, patients with macula off RRD have a higher risk for re-detachment, which probably due to the more extensive and longer persistent retinal detachment [18].
In conclusion, we recommend using the type of retinopexy you are more familiar with, as both techniques, if properly applied, have no major disadvantages in terms of higher re-detachment rate.
Abbreviations
- PPV:
-
Pars plana vitrectomy
- PVR:
-
Proliferative vitreoretinopathy
- RRD:
-
Rhegmatogenous retinal detachment
References
Sodhi A, Leung LS, Do DV, Gower EW, Schein OD, Handa JT. Recent trends in the Management of Rhegmatogenous Retinal Detachment. Surv Ophthalmol. 2008;53(1):50–67.
Eibenberger K, Georgopoulos M, Rezar-Dreindl S, Schmidt-Erfurth U, Sacu S. Development of surgical Management in Primary Rhegmatogenous Retinal Detachment Treatment from 2009 to 2015. Curr Eye Res. 2018;00(00):1–9.
Nemet A, Moshiri A, Yiu G, Loewenstein A, Moisseiev E. A review of innovations in Rhegmatogenous retinal detachment surgical techniques. J Ophthalmol. 2017;2017:1–5.
Kuhn F, Aylward B. Rhegmatogenous retinal detachment: a reappraisal of its pathophysiology and treatment. Ophthalmic Res. 2014;51(1):15–31.
Campochiaro PA, Kaden IH, Vidaurri Leal J, Glaser BM. Cryotherapy enhances intravitreal dispersion of viable retinal pigment epithelial cells. Arch Ophthalmol. 1985;103(3):434–6.
Umanets N, Pasyechnikova NV, Naumenko VA, Henrich PB. High-frequency electric welding: a novel method for improved immediate chorioretinal adhesion in vitreoretinal surgery. Graefe’s. Arch Clin Exp Ophthalmol. 2014;252(11):1697–703.
Zauberman H. Tensile strength of chorioretinal lesions produced by photocoagulation, diathermy, and cryopexy. Br J Ophthalmol. 1969;53(11):749–52.
Yoon YH, Marmor MF. Rapid enhancement of retinal adhesion by laser photocoagulation. Ophthalmology. 1988;95(10):1385–8.
Bonnet M, Guenoun S. Surgical risk factors for severe postoperative proliferative vitreoretinopathy (PVR) in retinal detachment with grade B PVR. Graefes Arch Clin Exp Ophthalmol. 1995;233(12):789–91.
Lincoff H, Kreissig I. The mechanism of the cryosurgical adhesion. IV. Electron microscopy. Mod Probl Ophthalmol. 1972;10:99–106.
Bonnet M. Clinical factors predisposing to massive proliferative vitreoretinopathy in rhegmatogenous retinal detachment. Ophthalmologica. 1984;188(3):148–52.
Bonnet M, Fleury J, Guenoun S, Yaniali A, Dumas C, Hajjar C. Cryopexy in primary rhegmatogenous retinal detachment: a risk factor for postoperative proliferative vitreoretinopathy? Graefes Arch Clin Exp Ophthalmol. 1996;234(12):739–43.
Jaccoma EH, Conway BP, Campochiaro PA. Cryotherapy causes extensive breakdown of the blood-retinal barrier: a comparison with argon laser photocoagulation. Arch Ophthalmol. 1985;103(11):1728–30.
Chaudhary R, Dretzke J, Scott R, Logan A, Blanch R. Clinical and surgical risk factors in the development of proliferative vitreoretinopathy following retinal detachment surgery: a systematic review protocol. Syst Rev. 2016;5(1):1–5.
Ciprian D. The pathogeny of proliferative vitreoretinopathy. Rom J Ophthalmol. 2015;59(2):88–92.
Hillier RJ, Stappler T, Williams RL, Turner GS, Wong D. The impact of axial length on retinal tamponade for gas, silicone oil, and heavy silicone oil, using an in vitro model. Graefes Arch Clin Exp Ophthalmol. 2011;249(5):671–5.
Martínez-Castillo V, Zapata MA, Boixadera A, Fonollosa A, García-Arumí J. Pars Plana vitrectomy, laser Retinopexy, and aqueous tamponade for Pseudophakic Rhegmatogenous retinal detachment. Ophthalmology. 2007;114(2):297–303.
Wickham L, Ho-Yen GO, Bunce C, Wong D, Charteris DG. Surgical failure following primary retinal detachment surgery by vitrectomy: risk factors and functional outcomes. Br J Ophthalmol. 2011;95(9):1234–8. https://doi.org/10.1136/bjo.2010.190306 Epub 2010 Dec 13.
Acknowledgements
We thank Dr. sc. nat. Sabine Güsewell for her assistance in statistical analysis.
Funding
No financial support
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
MB has made substantial contributions to acquisition of data, analysis and interpretation of data; and has been involved in drafting the manuscript. CV has been involved in drafting the manuscript and revising it critically for important intellectual content. HS has been involved in drafting the manuscript and revising it critically for important intellectual content. JG has been involved in drafting the manuscript and revising it critically for important intellectual content; has given final approval of the version to be published. Each author should have participated sufficiently in the work to take public responsibility for appropriate portions of the content; and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the local ethic committee and was performed as a part of departmental quality control (EKOS (Ethikkommission Ostschweiz), BASEC (Business Administration System for Ethics Committees) number 2018–00104). Research adhered to the tenets of the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Bentivoglio, M., Valmaggia, C., Scholl, H.P.N. et al. Comparative study of endolaser versus cryocoagulation in vitrectomy for rhegmatogenous retinal detachment. BMC Ophthalmol 19, 96 (2019). https://doi.org/10.1186/s12886-019-1099-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12886-019-1099-9