Abstract
Purpose
To investigate foveal morphologic parameters related to visual acuity and the stages classified in this study reflect the severity of the macular pseudohole (MPH).
Methods
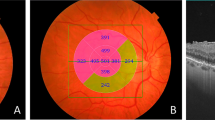
Seventy-eight eyes of 78 consecutive patients diagnosed with MPH were studied. Quantitative optical coherence tomography (OCT) parameters including central foveal thickness, parafoveal thickness, parafoveal inner and outer retinal thickness (PIRT and PORT), pseudohole depth, pseudohole diameter, and inner nuclear layer (INL) angulation were measured and the morphologic features of the inner retina (disorganization of retinal inner layers (DRIL)) and the photoreceptor layer (external limiting membrane (ELM), ellipsoid zone (EZ), interdigitation zone (IZ), and cotton ball sign) were determined. Associations between OCT parameters and best-corrected visual acuity (BCVA) were analyzed. Based on the location of the inner margin of INL, all patients were divided into three stages and the mean comparison between the three stages was analyzed.
Results
PIRT (r = 0.6489; p < 0.0001) and pseudohole depth (r = 0.5266; p < 0.0001) had a statistically significant correlation with BCVA. Statistically significant visual acuity differences were found in eyes with DRIL (p < 0.001) and IZ disruption (p = 0.018), but not in ELM disruption (p = 0.916), EZ disruption (p = 0.581), and cotton ball sign (p = 0.075). According to the univariate and multivariate regression analyses, PIRT was associated with BCVA in both univariate (p < 0.001) and multivariate (p = 0.002) regression analyses. Defect diameters of both ELM (p = 0.025) and IZ (p = 0.006) were associated with BCVA in univariate regression analysis, but not in multivariate regression analysis.
INL angulation and the ratio of the IZ disruption was significantly different in the three groups. Stage 3 (95.8%) had significantly higher disrupted IZ ratio than stage 1 (40%) and stage 2 (65.5%). The BCVA of stages 1, 2, and 3 were identified as 0.06 ± 0.07 (20/23 Snellen equivalent), 0.23 ± 0.17 (20/34 Snellen equivalent), and 0.48 ± 0.23 (20/60 Snellen equivalent), respectively, and the differences in BCVA between the three groups were significant (p < 0.0001).
Conclusion
The parameters related to visual acuity were PIRT, pseudohole depth, DRIL, and IZ. The stage classification proposed in this study included morphologic changes of the inner retina and photoreceptor layer and is likely to be clinically useful for showing the severity of the MPH.





Similar content being viewed by others
References
Allen AW Jr, Gass JD (1976) Contraction of a perifoveal epiretinal membrane simulating a macular hole. Am J Ophthalmol 82:684–691. https://doi.org/10.1016/0002-9394(76)90002-7
Haouchine B, Massin P, Tadayoni R, Erginay A, Gaudric A (2004) Diagnosis of macular pseudoholes and lamellar macular holes by optical coherence tomography. Am J Ophthalmol 138:732–739. https://doi.org/10.1016/j.ajo.2004.06.088
Wilkins JR, Puliafito CA, Hee MR, Duker JS, Reichel E, Coker JG, Schuman JS, Swanson EA, Fujimoto JG (1996) Characterization of epiretinal membranes using optical coherence tomography. Ophthalmology 103:2142–2151. https://doi.org/10.1016/s0161-6420(96)30377-1
Massin P, Allouch C, Haouchine B, Metge F, Paques M, Tangui L, Erginay A, Gaudric A (2000) Optical coherence tomography of idiopathic macular epiretinal membranes before and after surgery. Am J Ophthalmol 130:732–739. https://doi.org/10.1016/s0002-9394(00)00574-2
Gaudric A, Aloulou Y, Tadayoni R, Massin P (2013) Macular pseudoholes with lamellar cleavage of their edge remain pseudoholes. Am J Ophthalmol 155:733–742. https://doi.org/10.1016/j.ajo.2012.10.021
Duker JS, Kaiser PK, Binder S, de Smet MD, Gaudric A, Reichel E, Sadda SR, Sebag J, Spaide RF, Stalmans P (2013) The International Vitreomacular Traction Study Group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology 120:2611–2619. https://doi.org/10.1016/j.ophtha.2013.07.042
Michalewska Z, Michalewski J, Odrobina D, Nawrocki J (2012) Non-full-thickness macular holes reassessed with spectral domain optical coherence tomography. Retina 32:922–929. https://doi.org/10.1097/IAE.0b013e318227a9ef
Chen JC, Lee LR (2008) Clinical spectrum of lamellar macular defects including pseudoholes and pseudocysts defined by optical coherence tomography. Br J Ophthalmol 92:1342–1346. https://doi.org/10.1136/bjo.2007.133041
Hirota K, Itoh Y, Rii T, Inoue M, Hirakata A (2015) Correlation between foveal interdigitation zone band defect and visual acuity after surgery for macular pseudohole. Retina 35:908–914. https://doi.org/10.1097/IAE.0000000000000414
Fish RH, Anand R, Izbrand DJ (1992) Macular pseudoholes. Clinical features and accuracy of diagnosis. Ophthalmology 99:1665–1670. https://doi.org/10.1016/S0161-6420(92)31747-6
Greven CM, Slusher MM, Czyz CN (1998) The natural history of macular pseudoholes. Am J Ophthalmol 125:360–366. https://doi.org/10.1016/s0002-9394(99)80147-0
Zur D, Iglicki M, Feldinger L, Schwartz S, Goldstein M, Loewenstein A, Barak A (2018) Disorganization of retinal inner layers as a biomarker for idiopathic epiretinal membrane after macular surgery-the DREAM study. Am J Ophthalmol 196:129–135. https://doi.org/10.1016/j.ajo.2018.08.037
Tsunoda K, Watanabe K, Akiyama K, Usui T, Noda T (2012) Highly reflective foveal region in optical coherence tomography in eyes with vitreomacular traction or epiretinal membrane. Ophthalmology 119:581–587. https://doi.org/10.1016/j.ophtha.2011.08.026
Mori K, Gehlbach PL, Sano A, Deguchi T, Yoneya S (2004) Comparison of epiretinal membranes of differing pathogenesis using optical coherence tomography. Retina 24:57–62. https://doi.org/10.1097/00006982-200402000-00009
Michalewski J, Michalewska Z, Cisiecki S, Nawrocki J (2007) Morphologically functional correlations of macular pathology connected with epiretinal membrane formation in spectral optical coherence tomography (SOCT). Graefes Arch Clin Exp Ophthalmol 245:1623–1631. https://doi.org/10.1007/s00417-007-0579-4
Treumer F, Wacker N, Junge O, Hedderich J, Roider J, Hillenkamp J (2011) Foveal structure and thickness of retinal layers long-term after surgical peeling of idiopathic epiretinal membrane. Invest Ophthalmol Vis Sci 52:744–750. https://doi.org/10.1167/iovs.10-6310
Bu SC, Kuijer R, Li XR, Hooymans JM, Los LI (2014) Idiopathic epiretinal membrane. Retina 34:2317–2335. https://doi.org/10.1097/IAE.0000000000000349
Suzuki T, Terasaki H, Niwa T, Mori M, Kondo M, Miyake Y (2003) Optical coherence tomography and focal macular electroretinogram in eyes with epiretinal membrane and macular pseudohole. Am J Ophthalmol 136:62–67. https://doi.org/10.1016/s0002-9394(03)00149-1
Witkin AJ, Ko TH, Fujimoto JG, Schuman JS, Baumal CR, Rogers AH, Reichel E, Duker JS (2006) Redefining lamellar holes and the vitreomacular interface: an ultrahigh-resolution optical coherence tomography study. Ophthalmology 113:388–397. https://doi.org/10.1016/j.ophtha.2005.10.047
Yang HS, Kim JT, Joe SG, Lee JY, Yoon YH (2015) Postoperative restoration of foveal inner retinal configuration in patients with epiretinal membrane and abnormally thick inner retina. Retina 35:111–119. https://doi.org/10.1097/IAE.0000000000000276
Govetto A, Lalane RA 3rd, Sarraf D, Figueroa MS, Hubschman JP (2017) Insights into epiretinal membranes: presence of ectopic inner foveal layers and a new optical coherence tomography staging scheme. Am J Ophthalmol 175:99–113. https://doi.org/10.1016/j.ajo.2016.12.006
Varano M, Scassa C, Capaldo N, Sciamanna M, Parisi V (2002) Development of macular pseudoholes: a 36-month period of follow-up. Retina 22:435–442. https://doi.org/10.1097/00006982-200208000-00007
Purtskhvanidze K, Balken L, Hamann T, Wöster L, von der Burchard C, Roider J, Treumer F (2018) Long-term follow-up of lamellar macular holes and pseudoholes over at least 5 years. Graefes Arch Clin Exp Ophthalmol 256:1067–1078. https://doi.org/10.1007/s00417-018-3972-2
Funding
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF), funded by the Ministry of Education (2016R1A6A1A03010528).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclaimer
All authors have not published or submitted any related papers of the present study.
Conflict of interest
Young-Hoon Park was supported by grants from the Basic Science Research Program through the National Research Foundation of Korea (NRF), funded by the Ministry of Education (2016R1A6A1A03010528). The following authors have no financial disclosures: Hee Chan Ku, Eun Hyung Cho, Jeong Mo Han, and Eun Koo Lee.
Ethical approval
This study was approved by the Institutional Review Board of Kong Eye Hospital, and the research protocol adhered to the tenets of the 1964 Declaration of Helsinki and its later amendments. For this type of study, formal consent not was required.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ku, H.C., Cho, E.H., Han, J.M. et al. Angulation of the inner nuclear layer as an indicator of the severity of macular pseudohole. Graefes Arch Clin Exp Ophthalmol 259, 69–79 (2021). https://doi.org/10.1007/s00417-020-04822-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-020-04822-5