Abstract
Purpose
To investigate the alterations of central choroidal thickness (CCT) and macular choroidal blood flow in patients with hypertensive chorioretinopathy treated with antihypertensive agents.
Methods
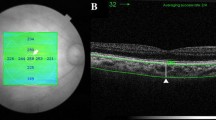
In retrospective observational case series, ten eyes of 9 patients with hypertensive chorioretinopathy were enrolled (5 men and 4 women; 43.1 ± 19.6 years of age). CCT and mean blur rate (MBR) had been observed during follow-up using enhanced depth imaging optical coherence tomography and laser speckle flowgraphy, respectively.
Results
With the medication for hypertension, serous retinal detachment (SRD) disappeared in all the eyes (mean period, 57.8 ± 50.4 days), and the mean blood pressure decreased (122.7 ± 13.0 mmHg and 93.4 ± 13.2 mmHg at the initial visit and at the day of subretinal fluid absorption, respectively; P < 0.01). The mean logMAR value of best corrected visual acuity showed a tendency toward improvement with the resolution of SRD (0.15 ± 0.30 and 0.08 ± 0.28, P = 0.15). The average MBR significantly decreased when SRD was absorbed (11.4 ± 4.5 and 7.7 ± 2.2, P < 0.01). Similarly, the mean values of CCT decreased (473.2 ± 218.0 μm and 325.7 ± 112.0 μm, P < 0.01). The changing rates of CCT and MBR showed a significant positive correlation (P < 0.01, R = 0.88).
Conclusion
The current study demonstrated a novel finding that choroidal blood flow velocity and thickness concurrently increased in the acute phase of hypertensive chorioretinopathy, suggesting the role of choroidal hyperperfusion in the pathogenesis of hypertensive chorioretinopathy.



Similar content being viewed by others
References
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr., Jones DW, Materson BJ, Oparil S, Wright JT, Jr., Roccella EJ, Joint National Committee on Prevention DE, Treatment of High Blood Pressure. National Heart L, Blood I, National High Blood Pressure Education Program Coordinating C (2003) Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension 42(6):1206–1252. https://doi.org/10.1161/01.HYP.0000107251.49515.c2
Dewilde E, Huygens M, Cools G, Van Calster J (2014) Hypertensive choroidopathy in pre-eclampsia: two consecutive cases. Ophthalmic Surg Lasers Imaging Retina 45(4):343–346. https://doi.org/10.3928/23258160-20140617-02
Bourke K, Patel MR, Prisant LM, Marcus DM (2004) Hypertensive choroidopathy. J Clin Hypertens (Greenwich) 6(8):471–472
Morse PH (1968) Elschnig’s spots and hypertensive choroidopathy. Am J Ophthalmol 66(5):844–852
Schmidt D, Loffer KU (1993) Elschnig’s spots as a sign of severe hypertension. Ophthalmologica 206(1):24–28. https://doi.org/10.1159/000310357
Pohl ML (1988) Siegrist’s streaks in hypertensive choroidopathy. J Am Optom Assoc 59(5):372–376
Puri P, Watson AP (2001) Siegrist’s streaks: a rare manifestation of hypertensive choroidopathy. Eye (Lond) 15(Pt 2):233–234. https://doi.org/10.1038/eye.2001.70
Saito W, Saito M, Hashimoto Y, Ishida S (2016) Occult hypertensive choroidopathy: novel finding of suprachoroidal fluid. Graefes Arch Clin Exp Ophthalmol 254(6):1229–1231. https://doi.org/10.1007/s00417-015-3222-9
Kawashima M, Nakajima M, Kawamura A (2008) Indocyanine green angiographic findings of hypertensive choroidopathy. Retin Cases Brief Rep 2(2):154–157. https://doi.org/10.1097/ICB.0b013e318030a98d
Hayreh SS, Servais GE, Virdi PS (1986) Fundus lesions in malignant hypertension: VI. Hypertensive choroidopathy. Ophthalmology 93(11):1383–1400
Kishi S, Tso MO, Hayreh SS (1985) Fundus lesions in malignant hypertension: I. A pathologic study of experimental hypertensive choroidopathy. Arch Ophthalmol 103(8):1189–1197
Ahn SJ, Woo SJ, Park KH (2014) Retinal and choroidal changes with severe hypertension and their association with visual outcome. Invest Ophthalmol Vis Sci 55(12):7775–7785. https://doi.org/10.1167/iovs.14-14915
Saito M, Saito W, Hirooka K, Hashimoto Y, Mori S, Noda K, Ishida S (2015) Pulse waveform changes in macular choroidal hemodynamics with regression of acute central serous chorioretinopathy. Invest Ophthalmol Vis Sci 56(11):6515–6522. https://doi.org/10.1167/iovs.15-17246
Fraser-Bell S, Symes R, Vaze A (2017) Hypertensive eye disease: a review. Clin Exp Ophthalmol 45(1):45–53. https://doi.org/10.1111/ceo.12905
Daruich A, Matet A, Dirani A, Bousquet E, Zhao M, Farman N, Jaisser F, Behar-Cohen F (2015) Central serous chorioretinopathy: recent findings and new physiopathology hypothesis. Prog Retin Eye Res 48:82–118. https://doi.org/10.1016/j.preteyeres.2015.05.003
Alwassia AA, Adhi M, Duker JS (2013) Bilateral simultaneous central serous chorioretinopathy in a teenage girl with systemic arterial hypertension. Int Ophthalmol 33(1):79–82. https://doi.org/10.1007/s10792-012-9624-3
Hirano Y, Yasukawa T, Ogura Y (2010) Bilateral serous retinal detachments associated with accelerated hypertensive choroidopathy. Int J Hypertens 2010:964513. https://doi.org/10.4061/2010/964513
Stacey AW, Sozener CB, Besirli CG (2015) Hypertensive emergency presenting as blurry vision in a patient with hypertensive chorioretinopathy. Int J Emerg Med 8:13. https://doi.org/10.1186/s12245-015-0063-6
Piccolino FC, Borgia L (1994) Central serous chorioretinopathy and indocyanine green angiography. Retina 14(3):231–242
Prunte C (1995) Indocyanine green angiographic findings in central serous chorioretinopathy. Int Ophthalmol 19(2):77–82
Saito M, Saito W, Hashimoto Y, Yoshizawa C, Fujiya A, Noda K, Ishida S (2013) Macular choroidal blood flow velocity decreases with regression of acute central serous chorioretinopathy. Br J Ophthalmol 97(6):775–780. https://doi.org/10.1136/bjophthalmol-2012-302349
Velazquez-Villoria D, Marti Rodrigo P, DeNicola ML, Zapata Vitori MA, Segura Garcia A, Garcia-Arumi J (2019) Swept source optical coherence tomography evaluation of chorioretinal changes in hypertensive choroidopathy related to HELLP syndrome. Retin Cases Brief Rep 13(1):30–33. https://doi.org/10.1097/ICB.0000000000000524
Mawatari Y, Hirata A, Fukushima M, Tanihara H (2006) Choroidal dye filling velocity in patients with Vogt-Koyanagi-Harada disease. Graefes Arch Clin Exp Ophthalmol 244(8):1056–1059. https://doi.org/10.1007/s00417-005-0238-6
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human and animal rights and informed consent
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Saito, M., Noda, K., Saito, W. et al. Increased choroidal blood flow and choroidal thickness in patients with hypertensive chorioretinopathy. Graefes Arch Clin Exp Ophthalmol 258, 233–240 (2020). https://doi.org/10.1007/s00417-019-04511-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-019-04511-y