Abstract
Purpose
To determine the effect of distraction on posterior segment surgical performance using a virtual reality simulator in expert and novice ophthalmic surgeons.
Methods
Twenty subjects were given 6 min to read an unpublished research paper and then were randomized into two groups. Group 1 subjects were allowed 3 min to complete a standardized vitreoretinal simulated task undistracted. Group 2 subjects were asked six questions on the research paper whilst completing the same task. Each subject then performed the alternate scenario. Finally, all participants were asked six questions on the research paper whilst not operating.
Results
There was no evidence of a difference in the odometer values (p = 0.127), cognitive task score (p = 0.390) or overall surgical task scores (p = 0.113) between the two groups. The time taken by the distracted group was significantly greater (95% CI −26.03 to −1.67, t-test p = 0.028).
Conclusion
Distraction significantly increases the time taken to perform a simulated vitreoretinal surgical task for all grades of surgeon. More studies are required to understand the impact on different types of distraction on surgical performance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The effect of distraction on performance has been the subject of extensive research in fields such as driving and aviation, as it affects public safety. Cognitive distraction can adversely affect driving behavior – e.g. drivers spend less time looking to the periphery, checking instruments, mirrors or traffic lights, and also apply hard braking more frequently when distracted [1].
In the presence of two simultaneous stimuli, ‘dual task’ interference occurs, resulting in a delayed response to the second stimulus. One cannot process central operations for two tasks simultaneously and therefore cannot perform both tasks simultaneously to an equally high standard [2].
The effect of distraction on surgical performance and outcome has also attracted interest. Up to 1 in 10 patients admitted to hospital experience an adverse event, almost half of which are preventable and many of which are associated with surgical care [3]. Operating conditions can involve frequent disruptions and interruptions. These can be varied, such as unwanted background noise or music, bleeps or phone calls, the surgeon’s emotional state, doors opening, or being directly asked a relatively complex question about a subject unrelated to the operation being done. In one observational study, up to 39 events (distractions or interruptions, such as doors opening, phones/bleeps going off, irrelevant communication, etc.) were observed in a single case [4].
The objective of this study was to determine whether distraction has an effect on the performance of cognitive and simulated posterior segment surgical tasks, in surgeons of different levels of experience. We hypothesized that both cognitive and simulated surgical performance would be adversely affected in the distracted group.
Method
This was a randomized cross-over trial involving three levels of operator under two randomly assigned operating conditions (distracted and not distracted). As method of distraction, we chose to test recall of an unpublished research paper, which all subjects were given 6 min to read at the beginning of the task. We felt that this type of cognitive task would be less influenced by potential differences in vocabulary, arithmetic and reasoning skills among the candidates, which could otherwise influence the results. The candidates were then randomized into two groups and given two attempts to complete a standardized simulated vitreoretinal surgical task on a virtual reality simulator (posterior segment navigation module, EyeSi VRMagic, Germany). Everyone was allowed one practice run. The surgical task requires the operator to place a needle inside a series of balls arranged in a helix above the retina.
The task could be performed either with or without distraction, with a maximum of 3 min allowed. The distraction involved being asked a series of six questions on the research paper (chosen at random from a bank of twelve) whilst completing the surgical task. Candidates were randomly allocated to one of 2 groups in which the surgical tasks were performed repeatedly in alternate sequences. In Group 1, candidates first performed the task undistracted then while being distracted, while in Group 2 the candidates were distracted during the first attempt and undistracted in their second attempt.
Finally, all participants were asked the six remaining questions on the research paper whilst not operating. At the end of the task they were given scores for their performance at the cognitive task, and at the simulated surgical task (calculated from odometer value (mm), time taken (s), instrument slippage, injured lens/macular area (mm2), number of completed objects and overall score). The odometer value refers to the distance traveled by the instrument tip, and is a measure of efficiency. Instrument slippage refers to the number of times the instrument slipped out of the sphere during the task.
Between treatment comparisons were done for all subjects using paired statistical tests. An Anderson-Darling normality test was performed on the differences between results on each outcome. Where differences could be assumed to follow an underlying normal distribution, paired t-tests were performed, otherwise Wilcoxon tests were used. All analyses were done using Minitab (version 16) at a 5% significance level.
Results
Eight consultant ophthalmologists (including 2 vitreoretinal surgeons), seven trainee ophthalmologists at different levels of their training and with varying levels of exposure to vitreoretinal surgery, and five medical students were recruited into the study.
Table 1 shows the mean scores with standard deviation for the tasks for each grade of participant in the distracted and undistracted states.
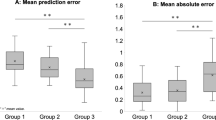
Figures 1, 2 and 3 show boxplots of the overall and the breakdown scores, comparing the ‘distracted’ and ‘undistracted’ scores for each grade of participant.
Overall surgical task score (Fig. 1)
There was no evidence of a difference in the overall surgical task scores between the two groups (Wilcoxon p = 0.113), and estimated median difference (undistracted – distracted) was 5 with a 95% CI of −0.5 to 14.0.
Time (Fig. 2)
The time taken by the distracted group was significantly greater than the undistracted group (paired t-test p = 0.028, 95% CI of 26.03 to −1.67).
Odometer values & rate of instrument slippage
There was no evidence of a difference in the odometer values between the two groups (paired t-test p = 0.127; 95% CI of −44.6 to 6.0 for undistracted – distracted).
There was some evidence to suggest that the rate of instrument slippage was higher in the distracted group – 95% CI for undistracted – distracted was −7.35 to 0.65 – but this difference did not reach statistical significance at the 5% level (paired t-test p = 0.096).
Cognitive task score (Fig. 3)
There was no evidence of a difference in cognitive task scores between the two groups: paired t-test p = 0.390, estimated mean difference (distracted – undistracted) was −0.59, with a 95% CI of −1.99 to 0.81.
Discussion
Observational studies [4, 5] have tried to determine the effect of distraction on surgical outcomes. In an analysis of events reported via Pennsylvania Patient Report System in the period between January 2011 and May 2013 [6], 304 procedure problems were found in which distraction had played a contributing part. These included events such as inadequate preparation of equipment, incorrect count of needles, and also ‘never events’ such as operations on the wrong body side.
With the advent of virtual reality simulators it is now possible to study the effects of different conditions on surgical outcomes without compromising patient safety [7,8,9,10]. Simulators have been used to study how distractions can influence surgical outcomes [11], including during intraocular procedures involving the anterior segment by Park et al. [7].
To our knowledge, this is the first study examining the effect of cognitive distraction on the performance of a simulated posterior segment surgical task.
For this study, we chose a crossover design whereby candidates were randomized to either of two different task orders (undistracted then distracted, or distracted then undistracted). This minimized the learning effect of repetition on the surgical outcome, which might have been a confounding factor had the same task order been applied to every participant.
Our study found no significant difference in the overall surgical task scores between the distracted and undistracted groups. This is in contrast to previous studies that have demonstrated a poorer performance with distractions [11,12,13]. For example, in their 2010 study involving 12 medical interns, Pluyter et al. [11] found that being distracted while performing a virtual laparoscopic cholecystectomy procedure not only adversely affected the task performance but also increased the levels of irritation of the interns (as measured by the blood pressure and heart rate). Similar findings were made in another study involving 18 surgical residents performing a laparoscopic cholecystectomy on a simulator, which showed an increase in the number of major surgical errors in the group randomized to distractions and interruptions [12].
It was interesting to note that there was no significant difference between the cognitive task scores, whether the candidate was operating or not. This differs from the 2010 study by Park [7], where performance in the cognitive task declined significantly when the candidates were dual-tasking – studies with larger sample sizes, or more challenging tasks, would be helpful to investigate this further.
The effect of surgical experience on the ability to cope with intraoperative distractions is debatable. In our study, we included different grades, as we thought it possible that consultants would be performing the task instinctively, and so would be less vulnerable to distraction, whereas less experienced staff would have to concentrate more fully on the allotted task, possibly leading to greater sensitivity to distraction. Some studies have shown a dramatic decrease in the psychological refractive period (delay in response to a second stimulus) following extended practice, which has been echoed in surgical literature, while others show little evidence of this improvement [2, 14]. In our study, distractions affected the time taken for the performance of the task for experts just as much as for the novices. It has been pointed out that performance on the EyeSi surgical stimulator varies widely among novices and therefore is not an appropriate criterion for recruitment into ophthalmology specialty training [15]. It is to be expected that experienced surgeons who have not used the EyeSi may initially get scores similar to novices. Although we might expect differences to emerge between different grades with longer and more complex tasks, getting volunteers to commit to a longer and more complex task presented practical difficulties.
Our method of distraction involved being tested on recall of a recently read paper. This might not have the same effect on surgical performance as other types of distraction such as background noise, or answering clinical or technical questions from theater staff or trainees. Furthermore, not all distractions are unwelcome. A randomized crossover trial by Shelby et al. [16] showed that residents took less time to complete a surgical task and produced a better quality of work while listening to their preferred genre of music than when they had the music off. However, the distraction in this study was chosen by the surgeon, which is not typical of most distractions encountered in the operating room. While some distractions are actively welcome or initiated by the surgeon (e.g. music, certain conversation topics), others can represent a cognitive distraction which is likely to have a more disruptive effect.
One of the limitations of our study was the small number of subjects involved. While this is comparable to previous studies looking at the effect of distraction on surgical performance, a larger number might produce more useful data.
Our participants were aware that the purpose of the study was to examine the effects of distraction on simulated surgical performance, and the nature of the experiment meant that it was not possible to mask them as to whether or not they were being distracted. This might have influenced them to take extra care with their performance on both the surgical and cognitive tasks, which is a possible explanation for the longer time taken and the similar outcomes between the distracted and undistracted groups for both tasks.
Can our results in a simulated setting be extrapolated to a real life operating theater? In real life, both the questions and the surgery would matter much more, and the consequences of an error would be much more serious. Under these circumstances it is possible that distraction may have an even greater effect than in our benign simulated environment. However, in addition to the ethical objections to deliberately distracting a surgeon during a real operation, measurements of surgical performance would be much more challenging.
Conclusion
In this study distraction led to significantly slower surgery for all grades of surgeons. However, we did not show any reduction in the surgical score. This provides some reassurance with regards to operative success and patient safety. More studies are required to understand how surgeons respond to different types of distraction. Until there is a better understanding of the effects of distraction on surgery, we recommend that theater staff minimize communication with the surgeon that is unrelated to the case in progress.
References
Harbluk JL, Noy YI, Trbovich PL et al (2007) An on-road assessment of cognitive distraction: impacts on drivers' visual behavior and braking performance. Accid Anal Prev 39(2):372–379
Van Selts M (1999) Can practice eliminate the psychological refractory period effect? J Exp Psychol 25:1268–1283
de Vries E, Ramrattan MA, Smorenburg SM et al (2008) The incidence and nature of in-hospital adverse events: a systematic review. Qual Saf Health Care 17:216–223
Sevdalis N, Undre S, McDermott J (2014) Impact of Intraoperative distractions on patient safety: a prospective descriptive study using validated instruments. World J Surg 38(4):751–758
Healey AN, Sevdalis N, Vincent CA (2006) Measuring intra-operative interference from distraction and interruption observed in the operating theatre. Ergonomics 49:589–604
Feil M (2014) Distractions in the operating room. PA-PSRS Patient Saf Advis 11:45–52
Park J, Waqar S, Kersey T et al (2011) Effect of distraction on simulated anterior segment surgical performance. J Cataract Refract Surg 37(8):1517–1522
Waqar S, Park J, Kersey TL, Modi N, Ong C, Sleep TJ (2011) Assessment of fatigue in intraocular surgery: analysis using a virtual reality simulator. Graefes Arch Clin Exp Ophthalmol 249:77–81
Waqar S, Williams O, Park J et al (2012) Can virtual reality simulation help to determine the importance of stereopsis in intraocular surgery? Br J Ophthalmol 96:742–746
Park J, Williams O, Waqar S et al (2012) Safety of nondominant-hand ophthalmic surgery. J Cataract Refract Surg 38:2112–2116
Pluyter JR, Buzink SN, Rutkowski AF (2010) Do absorption and realistic distraction influence performance of component task surgical procedure? Surg Endosc 24:902–907
Feuerbacher RL, Funk KH II, Spight DH et al (2012) Realistic distractions and interruptions that impair simulated surgical performance by novice surgeons. Arch Surg 147(11):1026–1030
Suh IH, Chien JH, Mukherjee M et al (2010) The negative effect of distraction on performance of robot-assisted surgical skills in medical students and residents. Int J Med Robotics Comput Assis Surg 6(4):377–381
Hsu KE, Man FY, Gizicki RA et al (2008) Experienced surgeons can do more than one thing at a time: effect of distraction on performance of a simple laparoscopic and cognitive task by experienced and novice surgeons. Surg Endosc 22(1):196–201
Gillian SN, Okravi N, O’Sullivan F et al (2016) Influence of medical student career aims on ophthalmic surgical simulator performance (part of the international forum for ophthalmic simulation studies). BJO 100:411–414
Lies SR, Zhang AY (2015) Prospective randomized study of the effect of music on the efficiency of surgical closures. Aesthet Surg J 35(7):858–863
Funding
The authors have no proprietary interests or research funding to declare. This work has previously been presented at the British and Eire Vitreoretinal Society Annual Meeting in Dublin, 2012.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
Informed consent was obtained from all individual participants included in the study. Approval by the National Health Service Research Ethics Committee was not required for this study, according to guidelines by the Medical Research Council Health Research Authority.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
McGowan, G., Jawaheer, L., Young, D. et al. QUIET PLEASE! Effect of distraction on simulated posterior segment surgical performance. Graefes Arch Clin Exp Ophthalmol 256, 519–523 (2018). https://doi.org/10.1007/s00417-017-3891-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-017-3891-7