Abstract
Purpose
The precise correction of refractive error is especially important in young adults. It is unclear whether cycloplegic refraction is necessary in this age group. The purpose of this study was to compare the non-cycloplegic and cycloplegic spherical equivalent (SE) refractive error measured in young adults.
Methods
This was a prospective study of 1400 eyes (n = 700) of enlisted soldiers aged 18 to 21 years who were consecutively evaluated in an outpatient army ophthalmology clinic. One drop of cyclopentolate 1 % was installed twice 10 min apart, and cycloplegic refraction was performed in both eyes 40 min later using an auto-refractor. The difference between non-cycloplegic and cycloplegic refractive measurements was analyzed.
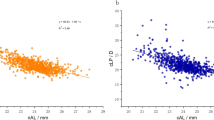
Results
The mean difference in SE between non-cycloplegic and cycloplegic measurements was 0.68 ± 0.83 D (95 % CI, 0.64–0.72). Significantly greater differences were observed in hypermetropes than myopes (1.30 ± 0.90 D versus 0.46 ± 0.68 D, p < 0.001). Moderate hypermetropes (2 to 5 D) demonstrated significantly greater refractive error than mild (0.5 to 2 D) or severe (>5 D) hypermetropes (1.71 ± 1.18 D versus 1.19 ± 0.74 D and 1.16 ± 1.08 D respectively, p < 0.001).
Conclusions
Young hypermetropic adults possessed +1 to +2 D of latent hypermetropia. In contrast, young myopic adults revealed pseudomyopia of −0.5 D. Cycloplegic refraction should be performed in young hypermetropic adults complaining of various signs of asthenopia.
Similar content being viewed by others
References
Savini G, Barboni P, Ducoli P, Borrelli E, Hoffer KJ (2014) Influence of intraocular lens haptic design on refractive error. J Cataract Refract Surg 40:1473–1478
Sales CS, Manche EE (2013) One-year outcomes from a prospective, randomized, eye-to-eye comparison of wavefront-guided and wavefront-optimized LASIK in myopes. Ophthalmology 120:2396–2402
Jin P, Zhu J, Zou H, Lu L, Zhao H, Li Q, He X (2015) Screening for significant refractive error using a combination of distance visual acuity and near visual acuity. PLoS One 10:e0117399
Leibowitz HM, Krueger DE, Maunder LR, Milton RC, Kini MM, Kahn HA, Nickerson RJ, Pool J, Colton TL, Ganley JP, Loewenstein JI, Dawber TR (1980) The Framingham Eye study monograph: an ophthalmological and epidemiological study of cataract, glaucoma, diabetic retinopathy, macular degeneration, and visual acuity in a general population of 2631 adults, 1973–1975. Surv Ophthalmol 24:335–610
Fotedar R, Rochtchina E, Morgan I, Wang JJ, Mitchell P, Rose KA (2007) Necessity of cycloplegia for assessing refractive error in 12-year-old children: a population-based study. Am J Ophthalmol 144:307–309
Chen J, Xie A, Hou L, Su Y, Lu F, Thorn F (2011) Cycloplegic and noncycloplegic refractions of Chinese neonatal infants. Invest Ophthalmol Vis Sci 52:2456–2461
Fotouhi A, Morgan IG, Iribarren R, Khabazkhoob M, Hashemi H (2012) Validity of noncycloplegic refraction in the assessment of refractive errors: the Tehran Eye Study. Acta Ophthalmol 90:380–386
Hashemi H, Fotouhi A, Mohammad K (2004) The age- and gender-specific prevalences of refractive errors in Tehran: the Tehran Eye Study. Ophthalmic Epidemiol 11:213–225
Krantz EM, Cruickshanks KJ, Klein BE, Klein R, Huang GH, Nieto FJ (2010) Measuring refraction in adults in epidemiological studies. Arch Ophthalmol 128:88–92
Sanfilippo PG, Chu BS, Bigault O, Kearns LS, Boon MY, Young TL, Hammond CJ, Hewitt AW, Mackey DA (2014) What is the appropriate age cut-off for cycloplegia in refraction? Acta Ophthalmol 92:e458–e462
American Optometric Association Consensus Panel (2006) Care of the Patient with Myopia http://www.aoa.org/documents/optometrists/CPG-15.pdf. Accessed 30 Oct 2015
American Optometric Association Consensus Panel (2008) Care of the Patient with Hyperopia http://www.aoa.org/documents/optometrists/CPG-16.pdf. Accessed 30 Oct 2015
Kleinstein RN, Mutti DO, Manny RE, Shin JA, Zadnik K (1999) Cycloplegia in African-American children. Optom Vis Sci 76:102–107
Fan DS, Rao SK, Ng JS, Yu CB, Lam DS (2004) Comparative study on the safety and efficacy of different cycloplegic agents in children with darkly pigmented irides. Clin Exp Ophthalmol 32:462–467
Morgan IG, Iribarren R, Fotouhi A, Grzybowski A (2015) Cycloplegic refraction is the gold standard for epidemiological studies. Acta Ophthalmol 93:581–585
Blehm C, Vishnu S, Khattak A, Mitra S, Yee RW (2005) Computer vision syndrome: a review. Surv Ophthalmol 50:253–262
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Funding
No grant support or funding was received for this research.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Informed consent
In the aforementioned clinics, all young soldiers under the age of 30 undergo both cycloplegic refraction and non-cycloplegic refraction, and therefore the study was exempt from collecting informed consent.
Rights and permissions
About this article
Cite this article
Mimouni, M., Zoller, L., Horowitz, J. et al. Cycloplegic autorefraction in young adults: is it mandatory?. Graefes Arch Clin Exp Ophthalmol 254, 395–398 (2016). https://doi.org/10.1007/s00417-015-3246-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-015-3246-1