Abstract
Background
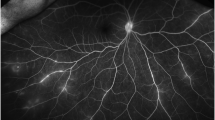
Fluorescein (FA) and indocyanine-green angiography (ICGA) may offer valuable information concerning disease severity and prognosis in ocular syphilis. The aim of the present study is to describe angiographic patterns encountered in the context of ocular syphilis, and to explore the associations between specific angiographic manifestations and severity of disease presentation, as well as disease evolution after treatment.
Methods
We performed a retrospective institutional study with the inclusion of 23 patients with ocular syphilis presenting to the uveitis clinic of the Jules-Gonin Eye Hospital in a 10-year period. FA and ICGA were performed following a standard protocol for posterior uveitis. Patterns of fluorescence were noted, and statistical associations between each angiographic pattern and any demographic, clinical, or laboratory parameter at baseline and after treatment were sought.
Results
The presence of any dark dots in ICGA was significantly associated with anterior uveitis (p = 0.031). The presence of hot spots in ICGA was significantly associated with longer duration of symptoms prior to initial visit (p = 0.032) and with male gender (p = 0.012). Weak non-significant trends were found associating vascular staining in FA with anterior uveitis (p = 0.066), vitritis (p = 0.069), and younger age (p = 0.061), as well as disc hyperfluorescence in FA with seropositivity for HIV (p = 0.089) and macular edema in FA with longer disease duration (p = 0.061). The presence of any dark dots in ICGA exhibited a weak trend of association with anterior uveitis and/or vitritis (p = 0.079).
Conclusions
Out of the several associations identified implicating specific angiographic features, we underline the possible role of the presence of dark dots in ICGA for identifying active inflammation, and the role of hot spots in ICGA as markers of long-standing disease. Vascular staining in FA appears to be more common in patients with severe ocular inflammation with presence of anterior uveitis and/or vitritis.



Similar content being viewed by others
References
Workowski KA, Berman S (2006) Sexually transmitted disease treatment guidelines. MMWR Morb Mortal Wkly Rep 55:22–26
Browning DJ (2000) Posterior segment manifestations of active ocular syphilis, their response to a neurosyphilis regimen of penicillin therapy, and the influence of human immunodeficiency virus status on response. Ophthalmology 107:2015–2023
Sudharshan S, Ganesh SK, Biswas J (2010) Current approach in the diagnosis and management of posterior uveitis. Indian J Ophthalmol 58:29–43
Tan-Yaycioglu R, Akova YA, Akca S, Yilmaz G (2006) Inflammation of the posterior uvea: findings on fundus fluorescein and indocyanine green angiography. Ocul Immunol Inflamm 14:171–179
De Laey JJ (1995) Fluorescein angiography in posterior uveitis. Int Ophthalmol Clin 35:33–58
Patz A (1977) Principles of fluorescein angiography. Int Ophthalmol Clin 17:1–19
Herbort CP, Bodaghi B, Lehoang P (2001) Indocyanine green angiography in ocular inflammatory diseases: principles, schematic interpretation, semiology and clinical value. J Fr Ophtalmol 24:423–447
Desmettre T, Devoisselle JM, Mordon S (2000) Fluorescence properties and metabolic features of indocyanine green (ICG) as related to angiography. Surv Ophthalmol 45:15–27
Mordon S, Devoisselle JM, Soulie-Begu S, Desmettre T (1998) Indocyanine green: physicochemical factors affecting its fluorescence in vivo. Microvasc Res 55:146–152
Gass JD, Braunstein RA, Chenoweth RG (1990) Acute syphilitic posterior placoid chorioretinitis. Ophthalmology 97:1288–1297
Mora P, Borruat FX, Guex-Crosier Y (2005) Indocyanine green angiography anomalies in ocular syphilis. Retina 25:171–181
Balaskas K, Sergentanis NT, Giulieri S, Guex-Crosier Y (2011) Analysis of significant factors influencing visual acuity in ocular syphilis. Br J Ophthalmol 96(11):1568–1572
Herbort CP, Lehoang P, Guex-Crosier Y (1998) Schematic interpretation of indocyanine green angiography in posterior uveitis using a standard angiographic protocol. Ophthalmology 105:432–440
Castellano CG, Stinnett SS, Mettu PS, McCallum RM, Jaffe GJ (2009) Retinal thickening in iridocyclitis. Am J Ophthalmol 148(3):341–349
Wolfensberger TJ, Herbort CP (1999) Indocyanine green angiographic features in ocular sarcoidosis. Ophthalmology 106:285–289
Wolfensberger TJ, Piguet B, Herbort CP (1999) Indocyanine green angiographic features in tuberculous chorioretinitis. Am J Ophthalmol 127:350–353
Kocak N, Saatci AO, Cingil G, Cimrin A, Ucar ES (2006) Miliary tuberculosis and bilateral multifocal choroidal involvement: place of indocyanine green angiography. Bull Soc Belge Ophtalmol 301:59–65
Acknowledgments
This article was the object of an oral presentation entitled “Angiographic patterns in ocular syphilis” at the EVER 2010 Congress held in Crete, Greece between 6 and 9 October 2010
We particularly thank Catherine Guex-Crosier for her valuable contribution to data collection and management.
Author information
Authors and Affiliations
Corresponding author
Additional information
No financial support or funding was received in support of this study
None of the authors have any financial or property interest in any product, method or material presented in this paper. No conflicting relationship exists for any author. The authors have full control of all primary data, and agree to allow Graefe’s Archive for Clinical and Experimental Ophthalmology to review their data if requested. Ethics Committee approval of the University of Lausanne was obtained
Appendix
Appendix
An eye-based analysis of registered data was performed in the service of comprehensiveness and in an attempt to exploit all available data. Angiographic manifestations encountered in FA and ICGA on an eye basis are presented in Table 7. With regard to associations implicating specific angiographic features, vascular staining in FA exhibited a statistically significant association with vitritis (8/19 eyes with vitritis also exhibited vascular staining in FA, whereas only 1/17 eyes without vitritis exhibited vascular staining, p = 0.020), anterior uveitis (7/15 eyes with anterior uveitis presented with vascular staining vs 2/21 eyes without anterior uveitis, p = 0.019) and a weak trend implicating macular edema (4/8 eyes with macular oedema vs 5/28 eyes without macular edema exhibited vascular staining, p = 0.086), with p-values derived from Fisher’s exact test. The association between vascular staining in fluorescein angiography with worse visual acuity at baseline did not reach formal statistical significance (p = 0.072, MWW), though there was a significant association with improvement in visual acuity after treatment (p = 0.005), as exhaustively described in a previous publication [12]. Disc hyperfluorescence in FA was significantly associated with seropositivity for HIV infection (3/3 eyes with HIV also exhibited disc hyperfluorescence vs only 6/33 eyes without HIV infection, p = 0.012, Fisher’s exact test).
Associations between the presence of any dark dots in ICGA and any other parameter are presented in Table 8. The presence of any dark dots was significantly associated with anterior uveitis (p = 0.013), vitritis (p = 0.034), while dark dots were observed in all seven eyes with relapse of inflammation after proper antibiotic treatment (p = 0.066). The presence of any hot spots in ICGA was associated with male gender (p < 0.001) and longer duration of symptoms prior to initial visit (p = 0.007), as can be seen in Table 9. There was, however, no association with relapse of inflammation after treatment (p = 0.201).
Rights and permissions
About this article
Cite this article
Balaskas, K., Sergentanis, T.N., Giulieri, S. et al. Fluorescein and indocyanine-green angiography in ocular syphilis: an exploratory study. Graefes Arch Clin Exp Ophthalmol 250, 721–730 (2012). https://doi.org/10.1007/s00417-011-1893-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-011-1893-4