Abstract
Background
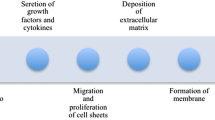
The cytokine transforming growth factor-ß (TGF-ß) is a pivotal contributor to tissue fibrosis and a key cytokine in the pathogenesis of cellular transdifferentiation, epithelial-mesenchymal transition (EMT), and cell adhesion. This study evaluates the effect of decorin, a naturally occurring TGF-ß inhibitor, in an experimental rabbit model for proliferative vitreoretinopathy (PVR).
Methods
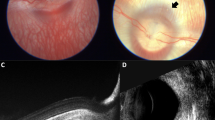
Traumatic PVR was induced in 50 rabbits divided into ten groups (n = 5). One group (GI) reveals a control with no treatment after trauma. Groups (GII–GIV) consisted of subgroups receiving phacovitrectomy at three different time points; (a) at the time of trauma, (b) 1 week following trauma, and (c) 2 weeks following trauma. GIII and GIV received 100 μg or 200 μg decorin, respectively. PVR severity was scored from 0 to 4. The amount of fibrosis was quantified using JMicroVision© software.
Results
The control group GI developed severe PVR with tractional retinal detachment (TRD); (PVR score ≥2) in four rabbits out of five. Vitrectomy had a positive effect (p < 0.05) on PVR development when preformed immediately, however the developed fibrosis was high. The best results were obtained when surgery was used in conjunction with decorin that reduced both the PVR score and fibrosis development significantly (p < 0.05). Depending on dosage and time of vitrectomy, PVR could be completely avoided (PVR score = 0) in 16 rabbits out of 30. TRD was prevented in 13 rabbits out of 15 in GIII to 14 rabbits out of 15 in GIV. In decorin-treated eyes, vitrectomy outcome was best when preformed at 1 week after trauma. There were no drug-related toxic effects evident on clinical and histopathological examination.
Conclusions
In conclusion, in this rabbit model of PVR, adjuvant decorin application during vitrectomy effectively reduces fibrosis and TRD development. In conjunction with no obvious histopathological toxicity signs, decorin represents a promising substance to inhibit PVR reactions.




Similar content being viewed by others
References
Tanihara H, Inatani M, Koga T, Yano T, Kimura A (2002) Proteoglycans in the eye. Cornea 21:S62–S69
Hagedorn M, Esser P, Wiedemann P, Heimann K (1993) Tenascin and decorin in epiretinal membranes of proliferative vitreoretinopathy and proliferative diabetic retinopathy. Ger J Ophthalmol 2:28–31
Iozzo R (1999) The biology of the small leucine-rich proteoglycan. J Biol Chem 27:18843–18846
Vogel KG, Paulsson M, Heinegard D (1984) Specific inhibition of type I and type II collagen fibrillogenesis by the small proteoglycan of tendon. Biochem J 223:587–597
Fleischmajer R, Fisher LW, MacDonald ED, Jacobs L Jr, Perlish JS, Termine JD (1991) Decorin interacts with fibrillar collagen of embryonic and adult human skin. J Struct Biol 106:82–90
Bidanset DJ, Guidry C, Rosenberg LC, Choi HU, Timpl R, Hook M (1992) Binding of the proteoglycan decorin to collagen type VI. J Biol Chem 267:5250–5256
Winnemoller M, Schon P, Vischer P, Kresse H (1992) Interactions between thrombospondin and the small proteoglycan decorin: interference with cell attachment. Eur J Cell Biol 59:47–55
Lewandowska K, Choi HU, Rosenberg LC, Zardi L, Culp LA (1987) Fibronectin-mediated adhesion of fibroblasts: inhibition by dermatan sulfate proteoglycan and evidence for a cryptic glycosaminoglycan-binding domain. J Cell Biol 105:1443–1454
Schmidt G, Robenek H, Harrach B, Glössl J, Nolte V, Hörmann H, Richter H, Kresse H (1987) Interaction of small dermatan sulfate proteoglycan from fibroblasts with fibronectin. J Cell Biol 104:1683–1691
Vogel KG, Trotter JA (1987) The effect of proteoglycans on the morphology of collagen fibrils formed in vitro. Coll Relat Res 7:105–114
Yamaguchi Y, Mann DM, Ruoslahti E (1990) Negative regulation of transforming growth factor- by the proteoglycan decorin. Nature 346:281–284
Takeuchi Y, Kodama Y, Matsumoto T (1994) Bone matrix decorin binds transforming growth factor- and enhances its bioactivity. J Biol Chem 269:32634–32638
Vial C, Gutierrez J, Santander C, Cabrera D, Brandan E (2011) Decorin interacts with CTGF/CCN2 through LRR12 inhibiting its biological activity. J Biol Chem 2011 Mar 23. [Epub ahead of print]
Nili N, Cheema AN, Giordano FJ, Barolet AW, Babaei S, Hickey R, Eskandarian MR, Smeets M, Butany J, Pasterkamp G, Strauss BH (2003) Decorin inhibition of PDGF-stimulated vascular smooth muscle cell function. Am J Pathol 163:869–878
Moscatello DK, Santra M, Mann DM, McQuillan DJ, Wong AJ, Iozzo RV (1998) Decorin suppresses tumor cell growth by activating the epidermal growth factor receptor. J Clin Invest 101:406–412
Iozzo RV, Moscatello DK, McQuillan DJ, Eichstetter I (1999) Decorin is a biological ligand for the epidermal growth factor receptor. J Biol Chem 274:4489–4493
Patel S, Santra M, McQuillan DJ, Iozzo RV, Thomas AP (1998) Decorin activates the epidermal growth factor receptor and elevates cytosolic Ca2+ in A431 carcinoma cells. J Biol Chem 273:3121–3124
Hausser H, Wedekind P, Sperber T, Peters R, Hasilik A, Kresse H (1996) Isolation and cellular localization of the decorin endocytosis receptor. Eur J Cell Biol 71:325–331
Rachal WF, Burton TC (1979) Changing concepts of failure after retinal detachment surgery. Arch Ophthalmol 97:480–483
Kauffmann DJ, van Meurs JC, Mertens DA, Peperkamp E, Master C, Gerritsen ME (1994) Cytokines in vitreous humor: interleukin-6 is elevated in proliferative vitreoretinopathy. Invest Ophthalmol Vis Sic 35:900–906
Limb GA, Little BC, Meager A, Ogilvie JA, Wolstencroft RA, Franks WA, Chignell AH, Dumonde DC (1991) Cytokines in proliferative vitreoretinopathy. Eye 5:686–693
Casaroli-Marano RP, Pagan R, Vilaró S (1999) Epithelial-mesenchymal transition in proliferative vitreoretinopathy: intermediate filament protein expression in retinal pigment epithelial cells. Invest Ophthalmol Vis Sci 40:2062–2072
Kalluri R, Neilson EG (2003) Epithelial-mesenchymal transition and its implications for fibrosis. J Clin Invest 112:1776–1784
Bornstein P (2001) Thrombospondins as matricellular modulators of cell function. J Clin Invest 107:929–934
Shah M, Foreman DM, Ferguson MW (1995) Neutralisation of TGF-beta 1 and TGF-beta 2 or exogenous addition of TGF-beta 3 to cutaneous rat wounds reduces scarring. J Cell Sic 108:985–1002
Cordeiro MF, Gay JA, Khaw PT (1999) Human anti-transforming growth factor-2 antibody: a new glaucoma anti-scarring agent. Invest Ophthalmol Vis Sci 40:2225–2234
Siriwardena D, Khaw PT, King AJ (2002) Human antitransforming growth factor beta (2) monoclonal antibody, a new modulator of wound healing in trabeculectomy: a randomized placebo controlled clinical study. Ophthalmology 190:427–431
Grisanti S, Szurman P, Warga M, Kaczmarek R, Ziemssen F, Tatar O, Bartz-Schmidt KU (2005) Decorin modulates wound healing in experimental glaucoma filtration surgery: a pilot study. Invest Ophthalmol Vis Sci 46:191–196
Cleary PE, Ryan SJ (1979) Experimental posterior penetrating eye injury in the rabbit I. Method of production and natural history. Br J Ophthalmol 63:306–311
Hsu HT, Ryan SJ (1986) Natural history of penetrating ocular injury with retinal laceration in the monkey. Graefes Arch Clin Exp Ophthalmol 224:1–6
Agrawal RN, He S, Spee C, Cui JZ, Ryan SJ, Hinton DR (2007) In vivo models of proliferative vitreoretinopathy. Nat Protoc 2:67–77
Vergara O, Ogden T, Ryan SJ (1989) Posterior penetrating injury to the rabbit eye: effect of blood and ferrous ions. Exp Eye Res 49:1115–1126
Cardillo JA, Stout JT, LaBree L, Azen SP, Omphroy L, Cui JZ, Kimura H, Hinton DR, Ryan SJ (1997) Post-traumatic proliferative vitreoretinopathy. The epidemiologic profile, onset, risk factors, and visual outcome. Ophthalmology 104:1166–1173
Sehu W, Lee W (2005) Ophthalmic pathology: an illustrated guide for clinicians. Blackwell Publishing Ltd, Massachusetts
Cardillo JA, Farah ME, Mitre J, Morales PH, Costa RA, Melo LA, Kuppermann B, Jorge R, Ashton P (2004) An intravitreal biodegradable sustained release naproxen and 5-fluorouracil system for the treatment of experimental post-traumatic proliferative vitreoretinopathy. Br J Ophthalmol 88:1201–1205
Roduit N (2010) JMicroVision: Image analysis toolbox for measuring and quantifying components of high-definition images. Version 1.2.2. http://www.jmicrovision.com. Access on 8 January 2010
Charteris DG (1995) Proliferative vitreoretinopathy: pathobiology, surgical management, and adjunctive treatment. Br J Ophthalmol 79:953–960
Ryan SJ (1985) The pathophysiology of proliferative vitreoretinopathy in its management. Am J Ophthalmol 100:188–193
Kolb M, Margetts PJ, Sime PJ, Gauldie J (2001) Proteoglycans decorin and biglycan differentially modulate TGF-beta-mediated fibrotic responses in the lung. Am J Physiol Lung Cell Mol Physiol 280:L1327–L1334
Ständer M, Naumann U, Wick W, Weller M (1999) Transforming growth factor-beta and p-21: multiple molecular targets of decorin-mediated suppression of neoplastic growth. Cell Tissue Res 296:221–227
Merle B, Malaval L, Lawler J, Delmas P, Clezadin P (1997) Decorin inhibits cell attachment to thrombospondin-1 by binding to a KKTR-dependent cell adhesive site present within the N-terminal domain of thrombospondin-1. J Cell Biochem 67:75–83
Merle B, Durussel L, Delmas PD, Clezardin P (1999) Decorin inhibits cell migration through a process requiring its glycosaminoglycan side chain. J Cell Biochem 75:538–546
Yamaguchi Y, Ruoslahti E (1988) Expression of human proteoglycan in Chinese hamster ovary cells inhibits cell proliferation. Nature 336:244–246
De Luca A, Santra M, Baldi A, Giordano A, Iozzo RV (1996) Decorin-induced growth suppression is associated with up-regulation of p21, an inhibitor of cyclin-dependent kinases. J Biol Chem 271:18961–18965
Isaka Y, Brees D, Ikegaya K, Kaneda Y, Imai E, Noble N (1996) Gene therapy by skeletal muscle expression of decorin prevents fibrotic disease in rat kidney. Nat Med 2:418–423
Giri S, Hyde D, Braun R, Gaarde W (1997) Antifibrotic effect of decorin in a bleomycin hamster model of lung fibrosis. Biochem Pharmacol 54:1205–1217
Logan A, Baird A, Berry M (1999) Decorin attenuates gliotic scar formation in the rat cerebral hemisphere. Exp Neurol 159:504–510
Fukushima K, Badlani N, Usas A, Riano F, Fu F, Huard J (2001) The use of an antifibrosis agent to improve muscle recovery after laceration. Am J Sports Med 29:394–402
Mohan RR, Gupta R, Mehan MK, Cowden JW, Sinha S (2010) Decorin transfection suppresses profibrogenic genes and myofibroblast formation in human corneal fibroblasts. Exp Eye Re 91:238–245
Cleary PE, Larus G, Ryan SJ (1979) Experimental posterior penetrating eye injury in the rhesus monkey: vitreous-lens admixture. Br J Ophthalmol 64:801–808
Cleary PE, Ryan SJ (1981) Vitrectomy in penetrating eye injury. Results of a controlled trial of vitrectomy in an experimental posterior penetrating eye injury in the rhesus monkey. Arch Ophthalmol 99:287–292
Cleary PE, Ryan SJ (1979) Experimental posterior penetrating eye injury in the rabbit II. Histology of wound, vitreous, and retina. Br J Ophthalmol 63:312–321
Hsu HT, Ryan SJ (1986) Experimental retinal detachment in the rabbit. Penetrating ocular injury with retinal laceration. Retina 6:66–69
Margo CE, Lee A (1995) Fixation of whole eyes: the role of fixative osmolarity in the production of tissue artifact. Graefe's Arch Clin Exp Ophthalmol 233:366–370
Blumenkranz MS, Ophir A, Clafiin AJ, Kajek A (1982) Fluorouracil for the treatment of massive preretinal proliferation. Am J Ophthalmol 94:458–467
Fastenberg DM, Diddie KR, Sorgente N, Ryan SJ (1982) A comparison of different cellular innocula in an experimental model of massive periretinal proliferation. Am J Ophthalmol 93:559–564
Fastenberg DM, Diddie KR, Dorey K, Ryan SJ (1982) The role of cellular proliferation in an experimental model of massive periretinal proliferation. Am J Ophthalmol 93:565–572
Hida T, Chandler DB, Sheta SM (1987) Classification of the stages of proliferative vitreoretinopathy in a refined experimental model in the rabbit eye. Graefes Arch Clin Exp Ophthalmol 225:303–307
Au Eong KG, Kent D, Pieramici DJ (2002) Section III Mechanical globe injuries, chapter 23 vitreous and retina. In: Kuhn F, Pieramici DJ (eds) Ocular trauma principles and practice. Thieme Medical Publishers, New York, p 224
Mittra RA, Mieler WF (1999) Controversies in the management of open-globe injuries involving the posterior segment. Surv Ophthalmol 44:215–225
Spalding SC, Sternberg P Jr (1990) Controversies in the management of posterior segment ocular trauma. Retina 10(Suppl 1):S76–S82
Wang NK, Chen YP, Yeung L, Chen KJ, Chao AN, Kuo YH, Lee JS, Lai CC (2007) Traumatic pediatric retinal detachment following open globe injury. Ophthalmologica 221:255–263
Ashton P (2006) Retinal Drug Delivery. In: Jaffe JG, Ashton P, Pearson PA (eds) Intraocular drug delivery. Taylor and Francis Group, New York, pp 11–12
Girard P, Mimoun G, Karpouzas I, Montefiore G (1994) Clinical risk factors for proliferative vitreoretinopathy after retinal detachment surgery. Retina 14:417–424
Nagasaki H, Shinagawa K (1995) Risk factors for proliferative vitreoretinopathy. Curr Opin Ophthalmol 6:70–75
Mohan RR, Tovey JC, Gupta R, Sharma A, Tandon A (2011) Decorin biology, expression, function and therapy in the cornea. Curr Mol Med 11:110–128
Meenakshi J, Vidyameenakshi S, Ananthram D, Ramakrishnan KM, Jayaraman V, Babu M (2009) Low decorin expression along with inherent activation of ERK1, 2 in ear lobe keloids. Burns 5:519–526
Acknowledgements
This study was supported in part by Herbert Funke Foundation, Germany and by the ministry of high education of the Egyptian government. We thank Mrs. Christine Örün for her technical assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have no financial relationship with the sponsoring foundation. The authors have full control of all primary data and they agree to allow Graefes Archive for Clinical and Experimental Ophthalmology to review their data upon request.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Nassar, K., Lüke, J., Lüke, M. et al. The novel use of decorin in prevention of the development of proliferative vitreoretinopathy (PVR). Graefes Arch Clin Exp Ophthalmol 249, 1649–1660 (2011). https://doi.org/10.1007/s00417-011-1730-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-011-1730-9