Abstract
Background
To assess the prevalence and determinants of non-adherence to topical hypotensive treatment in glaucoma patients in order to support interventions targeting enhancement of patient adherence.
Methods
One-hundred and sixty-six glaucoma patients, recruited by nationwide multi-stage sampling, filled in an extensive and carefully developed questionnaire covering various theoretically relevant determinants of patient adherence which were categorized as psychosocial aspects, barriers and skills.
Results
Prevalence of self-reported non-adherence was 27.3%. Younger patients (<55 years of age) had a higher risk of being non-adherent. Forgetfulness, unavailability of eye drops and difficulties with holding the bottle above the eye when applying the eye drops were the most cited reasons for non-adherence. Fifty percent of the patients indicated that they required more information on the correct administration of eye drops. There was no association between non-adherence and sex, level of education, type of insurance, duration of disease or family history of glaucoma.
Conclusions
Non-adherence to topical glaucoma medication is fairly common. Aids that minimize forgetfulness and delivery systems facilitating the delivery of medications to the eye could be considered to enhance patient adherence before advancing to other therapies with additional risks and costs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Professionals agree upon the importance of adherence to ocular hypotensive medication in the treatment of glaucoma patients, to reduce the risk of visual impairment [1–5]. A systematic review of 63 studies assessing the relation between adherence and outcomes of medical treatments showed that non-adherent patients have a greater risk of a poor outcome than adherent patients [6]. Because poor adherence can result in ineffectiveness of treatments, improvement of adherence could prevent the need to advance to more aggressive therapies. However, despite the introduction of eye drops with fewer side effects and a simpler medication regimen during the last years, still 10% to 30% of glaucoma patients regularly omit prescribed doses [3, 7–11]. Few studies have yet been done that systematically assess the causes of deviation from medication regimen in glaucoma patients in order to improve patient care. Taylor et al. used a qualitative methodology to understand the motivation of 28 glaucoma patients not to comply. Forgetfulness was the most reported reason for non-adherence [12]. Tsai et al. developed a systematic classification of a wide range of potential obstacles to adherence to glaucoma medication. Seventy-one barriers to non-adherence were categorized into four groups: social/environmental factors, patient factors, provider factors and regimen factors [11]. Sleath et al. listed 13 problem areas, and asked patients if they experienced one or more problems with their glaucoma medications. Most reported problems included practical difficulty with drop administration, paying for medications and remembering to take the medication [13]. Interventions for enhancing adherence should be based on reasons for non-adherence, and should be applicable in regular, daily care [14]. Our aim was to quantitatively assess various relevant determinants of adherence to topical glaucoma medication that could later be addressed in an adherence-enhancing intervention.
Materials and methods
Patients
We conducted a cross-sectional multi-center study in the Netherlands, in which we enrolled 166 adult patients who were treated for primary open-angle glaucoma. Ethics committee approval was obtained, and all persons gave their informed consent before being included in the study. No selection was made based on duration of the disease or type of glaucoma medication used. Patients were recruited by multi-stage sampling. We took a random sample of 60 ophthalmologists from the directory of the Dutch Ophthalmological Society. They were asked to invite four consecutive glaucoma patients to fill in a self-administered questionnaire during their visit to the outpatient department. In case a patient was not willing or unable to participate in the study, the ophthalmologists were asked to select the next consecutive patient. Selection bias was minimized by asking four consecutive patients as, in this way, ophthalmologists could only select the first patient that they thought to be appropriate for participation. We expected that most ophthalmologists would be able to select a maximum of four patients during one outpatient clinic, and that workload was reduced by the selection of 60 ophthalmologists.
Based on a response rate of 50% and a target number of 100 patients, we planned to ask 200 patients to participate in the study. The 95% confidence interval of a frequency of one certain item would be: freq ± 1.96 × (freq × (1 – freq)/n)1/2. With 100 responding patients and a frequency of 10%, the 95% confidence interval would have been 4%-16%. With 100 responding patients and a frequency of 50%, the 95% confidence interval would have been 40%-60%.
Questionnaire
Non-adherence was defined as the failure to take topical hypotensive treatment as prescribed, i.e. the omission of prescribed doses. We aimed to include in the questionnaire all potential causes of non-adherence to glaucoma medication that were reported in the literature and that were put forward by patients and experts. To select appropriate items for the questionnaire, a systematic inventory of the relevant literature was conducted and four focus-group interviews with 21 glaucoma patients from four hospitals were held, one of which was a university hospital. In focus group patients, we made allowance for the duration of glaucoma and membership of the Glaucoma Patient Society. The duration of glaucoma in focus group patients ranged from 1 month to 22 years, and nine patients were members of the Glaucoma Patient Society. Members of the Glaucoma Patient Society were placed in one focus group, as well as patients with a short duration of glaucoma. Reasons for not mixing these patients with other patients included prevention of dominance of some patient groups and the different level of knowledge of members of the Glaucoma Patient Society and patients with short duration of glaucoma compared to other patients. In this way, we obtained a variety in patient characteristics in the focus groups.
Experts in ophthalmology, patient education and pharmacology reviewed the concept version of the questionnaire. In addition, we tested the questionnaire in a pilot study with ten patients. Based on key determinants from health education theory, we distinguished three clusters of causes: psychosocial determinants of behavior (including factors as for example attitude and social influence), barriers (e.g. co-morbidity and understanding) and skills [15]. We listed 34 possible determinants of non-adherence, consisting of 18 psychosocial reasons, six barriers and ten skills. Patients could fill in whether they had never missed an eye drop, whether they had missed an eye drop once or whether they had missed an eyedrop more than once because of the stated reason.
To discover any supplementary topics that could lead to better adherence if addressed in a patient education program, we examined patients’ subjective need for information. Therefore, we asked patients to indicate whether they preferred much, some or no information about 22 listed items concerning need for information.
Questions about the various causes of non-adherence were formulated in plain Dutch. Questions covered the past 4 weeks in order to minimize the risk of recall bias.
Statistical analysis
In order to minimize data-entry errors, experienced data typists entered the data twice and checked for discrepancies. If patients had not answered the question about how often they had missed an eye drop during the past 4 weeks (n = 11), we classified them as adherent or non-adherent according to the answers given to the questions concerning causes of non-adherence. Four patients who claimed not to have missed a single dose due to one of the reasons given were classified as adherent. Three patients who had missed an eye drop at least once due to one of the reasons given were classified as non-adherent. Four patients whose status of being adherent or non-adherent could not be determined and eight patients who did not use eye drops for glaucoma treatment at all were excluded from further analysis.
Statistical analyses were performed with 154 patients, using the software package SPSS 10.1. The χ2-test for independence of two nominal variables was employed to examine differences in frequency distributions of categorical variables between adherent and non-adherent patients. A p-value of < 0.05 was used to indicate statistical significance. Univariate logistic models were fitted per item to calculate the odds ratio of being non-adherent.
Results
Sociodemographic determinants
The response among the ophthalmologists was 73% (44/60). Of the 236 questionnaires we had handed out, 166 (70.3%) were returned. With respect to the patients, reasons not to participate in the study were cognitive dysfunction, language barriers and lack of time.
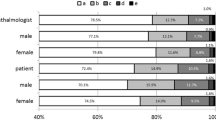
Table 1 shows the characteristics of the patients and the prevalence of the omission of doses. Twenty-six percent of the patients reported that they had missed an eye drop once or more than once during the past 4 weeks. After imputation, 27.3% of the patients were classified as non-adherent.
There was a statistically significant difference (p = 0.01) in the proportion of adherent and non-adherent patients between the different age groups (Table 2). The odds ratio of being non-adherent was less in the higher age categories compared to the lowest category (<54 years).
With respect to type of medication, differences in proportion of adherent and non-adherent patients did not reach statistical significance (p = 0.06). The unadjusted odds ratio for non-adherence in the patient group who received a combination therapy (≥ 2 different bottles) was 3.3 (95% CI [1.2; 9.6], p = 0.02) with patients prescribed a beta-blocker serving as reference group. There was no difference between patients prescribed a beta-blocker and patients prescribed latanoprost.
Patients who had undergone laser treatment seemed to be at greater risk for non-adherence than patients who had no history of surgical or laser treatment. However, this association was not statistically significant.
There were no statistically significant differences in proportion of adherent and non-adherent patients for sex, level of education, type of insurance, duration of disease or family history of glaucoma.
Psychosocial determinants, barriers and skills
The proportion of patients who admitted to having forgotten to administer their eye drops once or more was 26.7% (39/146). Other psychosocial reasons were reported by 0.7% to 4.2% of the patients (Table 3).
Twenty-three patients out of 145 (15.9%) reported that they had omitted their medication once or more than once because they did not have eye drops or gel with them (Table 4). All other barriers were reported as a reason for omission of eye drops by less than 5% of the patients.
Generally, difficulties with the correct administration of eye drops were reported by a greater proportion of patients as a reason for omission of doses than were psychosocial causes or barriers (Table 4). Difficulties with holding the bottle properly above their eye were most often reported (16% of the patients).
Finally, 50% of the patients indicated that they would like to receive more information on how to administer eye drops correctly (data not shown).
Discussion
Non-adherence to topical hypotensive treatment continues to be a considerable obstacle in the treatment of glaucoma patients, despite the recent development of drugs with relatively simpler treatments and fewer side-effects. In order to make a thorough inventory of the theoretically relevant determinants of non-adherence and their frequency distribution in glaucoma patients, we systematically developed an extensive questionnaire, including questions on psychosocial aspects, potential barriers and skills.
The systematically developed questionnaire, based on focus group interviews, opinions of experts and a pilot test, included various causes of non-adherence. As the questions were formulated in plain Dutch and 95% of non-adherent patients reported one or more causes of non-adherence, socially acceptable responses are not expected. The risk of recall bias was minimized by asking about the previous 4 weeks. Moreover, 29.7% of the questionnaires were not returned for analysis, and it is not known whether patients who refused to be included were adherent or non-adherent. Possible bias in the interpretation of the data from this ignorance cannot be excluded. Reasons suggested by patients for not participating were cognitive dysfunction, language barriers and lack of time. Incentives were included for both the ophthalmologists and the patients to improve participation, and all ophthalmologists were contacted by telephone after 2 to 3 weeks and by mail after 6 to 8 weeks. With regard to the selection of patients, it is difficult to assess case order. As described earlier, selection bias was minimized by asking ophthalmologists to invite four consecutive patients to participate. It was the best method for reducing selection bias when compared to the situation in which each ophthalmologist selects one patient, or when compared to alternative methods that select patients in non-randomly selected hospitals, during pharmacy visits or from members of the Glaucoma Patient Society.
In this study, adherence was defined quite strictly as missing an eye drop once or more. Different studies use varying definitions of adherence and different assessment methods. Several studies define adherence as strictly as we did [11, 16–21]. Our result of 27.3% non-adherent patients corresponds with those of other reports that used questionnaires [22, 23], pharmacy refill records [8, 24] or electronic medication monitors [25] to assess adherence. Based on a systematic review of 569 studies from 1948 to 1998, involving 17 disease conditions, an average non-adherence rate of 24.8% and a non-adherence rate of 27.4% was found for eye disorders [26]. Although self-reported adherence is a subjective measure of adherence, it has been shown to be a much better measure of adherence than one believed formerly. Adherence data assessed by electronic monitoring and a medication diary were comparable in cancer patients with pain [27]. In a comparison of various methods for measuring adherence to HIV protease inhibitors, patients’ self-reported adherence showed relatively high and significant correlations with results from medication event monitoring systems [28].
Our study shows that forgetfulness, unavailability of medication and insufficient skills for the most part contributed to the omission of doses. Side effects, social influence, inconvenience of therapy or a negative attitude towards the treatment only played a minor role. Furthermore, younger patients and those receiving a combination therapy (≥2 different bottles) were significantly more likely to be non-adherent.
Our findings are consistent with that of various studies which report forgetfulness as one of the major causes cited by glaucoma patients for the omission of prescribed doses [3, 12, 17, 21, 29]. An intuitively obvious and often-cited reason why glaucoma patients forget to take their eye drops is that there is no immediate disability from the disease and no direct advantage from the eye drops [5]. Non-acceptance of the disease as well as the necessity of chronic treatment may also be part of the cause. Tsai et al. categorized obstacles to medication adherence. Forty-nine percent of obstacles were categorized as social/environmental, 32% reflected regimen factors, and 16% involved individual patient factors. Only 3% of reported causes of non-adherence were of medical provider origin [11].
Insufficient skills or a lack of manual dexterity in many, especially older glaucoma patients or patients with co-morbidities have been recognized by different researchers [1, 3, 12, 13, 23, 30, 31]. Winfield et al. showed that about half of patients experienced technical difficulties with eye-drop administration, such as aiming, squeezing and blinking [23]. They reported that 72% of patients were never asked if they had any problems, and that 69% would not report any problems to their doctor even if asked [23]. Sleath et al. also showed that 44% of patients experienced difficulty with drop administration, and 14% of patients had trouble squeezing the bottle [13]. Our study agrees with these findings, as it shows that many patients are having difficulties in correctly administering eye drops, and that many patients require information on this issue.
Our result (that patients receiving a combination therapy were less adherent) corresponds to findings of Robin et al., who reported a significant increase in refill intervals after the addition of a second drug [32]. Moreover, Sleath et al. found that patients using more glaucoma medications experienced problems with the application of their therapy more often than patients taking fewer glaucoma medications [13]. Being treated with various topical medications at the same time might be confusing for some, especially older, patients, and seems an obvious reason for non-adherence. A recently undertaken study has objectively measured adherence by the use of electronic monitoring, and found that poorer adherence was associated with more complex regimens, although once-daily drugs in a complex dosing regimen resulted in good adherence [33]. They found a higher percentage of adherence than in our findings, which could be explained by the fact that patients in the study of Robin et al. were informed that their dosing behavior was being monitored [33]. While some studies suggest that reducing dose frequency will enhance adherence [9, 34–36], it has also been reported that many patients say that it would not make it easier to adhere to the regimen, although it would be more convenient, and patients prefer one drop once a day in terms of lifestyle [11, 37, 38]. Stewart et al. reported that 74% of physicians believed their patients would prefer once a day dosing, and 92% of physicians believed it would improve adherence. However, only 20% of patients believed they would be more adherent if they had a once a day dosing regimen [37]. The same association seems to exist for side-effects. Taylor et al. showed that only a few patients report non-adherence because of side-effects, while a lot of patients complain about them [12]. Jampel et al. show in a willingness-to-pay analysis that patients place differing value on certain eye-drop characteristics. Patients were especially willing to pay more for eye drops that did not produce blurring of vision, drowsiness or inhibition of sexual performance. Patients were least willing to pay more for reduction of dose frequency, and for a combination of two medications in one bottle rather than two bottles [39]. We think that a drug regimen with lower dosing frequency and fewer side-effects probably will not be the only solution for the adherence problem.
In our study, patients younger than 55 years of age were significantly less adherent than older patients. The working situation of this younger group, which does not allow the regular use of eye drops, or inconvenient effects such as blurred vision that hinder people in doing their work, might provide an explanation for this difference [29]. However, this study was not designed to discover why younger patients would be less adherent and no cause-effect relationship can be concluded because of the cross-sectional design of the study. An evidence-based review reported nine studies that had investigated the relation between age and non-adherence, and found that none of them reported significant results [9].
The finding that patients who had undergone laser therapy tended to be at higher risk of being non-adherent has to be interpreted with caution. Since the underlying study was cross-sectional, a cause-effect relationship cannot be concluded. Patients who had undergone laser therapy might be a selected group of non-adherent patients who had undergone laser therapy because topical hypotensive treatment was ineffective.
Several intervention studies have already tested the effect of a memory aid [18, 19, 40] or an education and tailoring program [41] on the prevalence of omission of doses. These studies lacked different aspects of trial quality, yet they all reported a small, but significant improvement of patient adherence. However, there are no data available on the effects of the different interventions in the long run, or on the feasibility or cost-effectiveness of their implementation in daily clinical routine. Newer dosing aids combine alarm features with a dosing lever, and register adherence data [42, 43]. Others suggest written instructions as a simple and inexpensive intervention, as written instructions improved the accuracy of self-reporting medication regimen [44]. Medication reviews are also seen as a tool for improving adherence [45]. Systematic reviews have shown that several types of intervention, such as technical, educational, behavioral and combined interventions, are effective in improving medication adherence in chronic medical disorders, but the effect on clinical outcomes was small [35, 36]. However, DiMatteo et al. and Hugen et al. have shown that non-adherence increases the risk of poor outcome of medical treatments [6, 28]. In general, the most powerful intervention is believed to consist of a combination of educational, behavioural and affective components [46]. No single intervention appears to be superior [47].
Although the present study has not proved it, we expect that adherence-enhancing interventions should pay special attention to the reduction of patient forgetfulness as well as the improvement of medication administration skills. An intervention focusing on other psychosocial determinants or barriers seems unnecessary. In patients in whom the intraocular pressure continues to be high, or progression of visual field loss occurs despite the prescription of a potent anti-glaucoma drug, patients’ skills in administering eye drops should be checked, and the use of a dosing aid or memory aid should be considered before turning to laser or surgical therapy.
References
Busche S, Gramer E (1997) Verbesserung der Augentropfenapplikation und Compliance bei Glaukompatienten; eine klinische Studie. Klin Monatsbl Augenheilkd 211:257–262
Forsman E, Kivel T, Vesti E (2007) Lifetime visual disability in open-angle glaucoma and ocular hypertension. J Glaucoma 16:313–319
Konstas AGP, Maskaleris G, Gratsonidis S, Sardelli C (2000) Compliance and viewpoint of glaucoma patients in Greece. Eye 14:752–756
Lee DA, Fechtner RD, Fiscella RG, Singh K, Stewart WC (2000) Emerging perspectives on glaucoma: highlights of a roundtable discussion. Am J Ophthalmol 130:S1–S11
Zimmerman TJ, Zalta AH (1983) Facilitating patient compliance in glaucoma therapy. Surv Ophthalmol 28:252–257
DiMatteo MR, Giordani PJ, Lepper HS, Croghan TW (2002) Patient adherence and medical treatment outcomes; a meta-analysis. Med Care 40:794–811
Deokule S, Sadiq S, Shah S (2004) Chronic open angle glaucoma: patient awareness of the nature of the disease, topical medication, compliance and the prevalence of systemic symptoms. Ophthal Physiol Opt 24:9–15
Gurwitz JH, Yeomans SM, Glynn RJ, Lewis BE, Levin R, Avorn J (1998) Patient noncompliance in the managed care setting; the case of medical therapy for glaucoma. Med Care 36:357–369
Olthoff CMG, Schouten JSAG, Van de Borne BW, Webers CAB (2005) Noncompliance with ocular hypotensive treatment in patients with glaucoma or ocular hypertension. Ophthalmology 112:953–961
Rotchford AP, Murphy KM (1998) Compliance with timolol treatment in glaucoma. Eye 12:234–236
Tsai JC, McClure CA, Ramos SE, Schlundt DG, Pichert JW (2003) Compliance barriers in glaucoma: a systematic classification. J Glaucoma 12:393–398
Taylor S, Galbraith S, Mills R (2002) Causes of non-compliance with drug regimens in glaucoma patients: a qualitative study. J Ocul Pharmacol Ther 18:401–409
Sleath B, Robin AL, Covert D, Byrd JE, Tudor G, Svarstad B (2006) Patient-reported behavior and problems in using glaucoma medications. Ophthalmology 113:431–436
Elliot R, Barber N, Horne R (2005) Cost-effectiveness of adherence-enhancing interventions: a quality assessment of the evidence. Ann Pharmacother 39:508–515
Meertens RM, Schaalma H, Brug J, De Vries N (2000) Determinanten van gedrag [Determinants of behavior]. In: Brug J, Schaalma H, Kok G, Meertens RM, Van der Molen HT (Eds) Gezondheidsvoorlichting en Gedragsverandering; een Planmatige Aanpak [Health promotion and behavior change: a systematic approach]. Van Gorcum, Assen Netherlands, pp 55–72
Amon M, Menapace R, Wedrich A, Radax U (1990) Aspekte der Betreuung von Glaukompatienten und deren Auswirkung auf die Compliance. Spektrum Augenheilkd 4:5–8
Bour T, Blanchard F, Segal A (1993) [Therapeutic observance and life of patients with primary open-angle glaucoma. Apropos of 341 cases in the department of Marne]. J Fr Ophtalmol 16:380–391(in French)
Chang J, Lee D, Petursson G, Spaeth G, Zimmerman T, Hoskins H, Mills R, Brown R, Kass M, Lue J (1991) The effect of a glaucoma medication reminder cap on patient compliance and intraocular pressure. J Ocul Pharmacol 7:117–124
Laster S, Martin J, Fleming J (1996) The effect of a medication alarm device on patient compliance with topical pilocarpine. J Am Optom Assoc 67:654–658
MacKean JM, Elkington AR (1983) Compliance with treatment of patients with chronic open-angle glaucoma. Br J Ophthalmol 67:46–49
Patel SC, Spaeth GL (1995) Compliance in patients prescribed eyedrops for glaucoma. Ophthalmic Surg 26:233–236
Bloch S, Rosenthal AR, Friedman DS, Caldarolla P (1977) Patient compliance in glaucoma. Br J Ophthalmol 61:531–534
Winfield AJ, Jessiman D, Esakowitz L (1990) A study of the causes of non-compliance by patients prescribed eyedrops. Br J Ophthalmol 74:477–480
Gurwitz JH, Glynn RJ, Monane M, Everitt DE, Gilden D, Smith N, Avorn J (1993) Treatment for glaucoma: adherence by the elderly. Am J Public Health 83:711–716
Kass MA, Meltzer DW, Gordon M, Cooper D, Goldberg J (1986) Compliance with topical pilocarpine treatment. Am J Ophthalmol 101:515–523
DiMatteo MR (2004) Variations in patients’ adherence to medical recommendations; a quantitative review of 50 years of research. Med Care 42:200–209
Oldenmenger W, Echteld M, Wit de R, Sillevis Smit P, Stronks D, Stoter G, Rijt van der C (2007) Analgesic adherence measurement in cancer patients: comparison between electronic monitoring and diary. J Pain Symptom Manage 34:639–647
Hugen P, Langebeek N, Burger D, Zomer B, Leusen van R, Schuurman R, Koopmans P, Hekster Y (2002) Assessment of adherence to HIV protease inhibitors: comparison and combination of various methods, including MEMS (electronic monitoring), patient and nurse report, and therapeutic drug monitoring. J Acquir Immune Defic Syndr 30:324–334
Kosoko O, Quigley HA, Vitale S, Enger C, Kerrigan L, Tielsch JM (1998) Risk factors for noncompliance with glaucoma follow-up visits in a residents's eye clinic. Ophthalmology 105:2105–2111
Brown M, Brown G, Spaeth G (1984) Improper topical self-administration of ocular medication among patients with glaucoma. Can J Ophthalmol 19:2–5
Dietlein TS (2006) Glaukom im Alter; Barrieren fur Aufklaerung und Compliance. Ophthalmologe 103:755–758
Robin AL, Covert D (2005) Does adjunctive glaucoma therapy affect adherence to the initial primary therapy? Ophthalmology 112:863–868
Robin A, Novack G, Covert D, Crockett R, Marcic T (2007) Adherence in glaucoma: objective measurements of once-daily and adjunctive medication use. Am J Ophthalmol 144:533–540
Mansukani SS (2002) Improving adherence to drug-treatment regimens for glaucoma. Manag Care 11:49–53
Kripalani S, Yao X, Haynes B (2007) Interventions to enhance medication adherence in chronic medical conditions; a systematic review. Arch Intern Med 167:540–550
Dulmen van S, Sluijs E, Dijk van L, Ridder de D, Heerdink R, Bensing J (2007) Patient adherence to medical treatment: a review of reviews. BMC Health Serv Res 7:55
Stewart WC, Konstas AGP, Pfeiffer N (2004) Patient and ophthalmologist attitudes concerning compliance and dosing in glaucoma treatment. J Ocul Pharmacol Ther 20:461–469
Buller AJ, Morgan LH, Hercules BL (2007) Patients prefer one-daily glaucoma drops. Graefes Arch Clin Exp Ophthalmol 245:293–294
Jampel HD, Schwartz GF, Robin AL, Abrams DA, Johnson E, Miller RB (2003) Patient preferences for eye drop characteristics. Arch Ophthalmol 121:540–546
Sclar D, Skaer T, Chin A (1991) Effectiveness of the C Cap in promoting prescription refill compliance among patients with glaucoma. Clin Ther 13:396–400
Norell SE (1979) Improving medication compliance: a randomised clinical trial. Br Med J 2:1031–1033
Flowers B, Wand M, Piltz-Seymour J, Berke S, Day D, Teague J, Smoot T, Landry T, Bergamini M, Mallick S (2006) Patients’ and physicians’ perceptions of the Travoprost dosing aid: an open-label, multicenter study of adherence with prostaglandin analogue therapy for open-angle glaucoma or ocular hypertension. Clin Ther 28:1803–1811
Boden C, Sit A, Weinreb RN (2006) Accuracy of an electronic monitoring and reminder device for use with travoprost eye drops. J Glaucoma 15:30–34
Kharod BV, Johnson PB, Nesti HA, Rhee DJ (2006) Effect of written instructions on accuracy of self-reporting medication regimen in glaucoma patients. J Glaucoma 15:244–247
Lefante JJ, Harmon GN, Roy W, Fontenot S, Brown K, Webber L (2005) The effect of medication reviews in a rural community pharmacy assistance program: the cenla medication access program. J Pharm Pract 18:486–492
Roter DL, Hall JA, Merisca R, Nordstrom B, Cretin D, Svarstad B (1998) Effectiveness of interventions to improve patient compliance; a meta-analysis. Med Care 36:1138–1161
Peterson A, Takiya L, Finley R (2003) Meta-analysis of trials of interventions to improve medication adherence. Am J Health Syst Pharm 60:657–665
Acknowledgements
This study was supported by a grant of the national “Health Care Insurance Board”, Amstelveen, The Netherlands.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was supported by a grant of the national “Health Care Insurance Board”, Amstelveen, The Netherlands. The authors do not have any financial relationship with this organization. The authors have full control of all primary data, and allow Graefe’s Archive for Clinical and Experimental Ophthalmology to review the data if requested.
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Olthoff, C.M.G., Hoevenaars, J.G.M.M., van den Borne, B.W. et al. Prevalence and determinants of non-adherence to topical hypotensive treatment in Dutch glaucoma patients. Graefes Arch Clin Exp Ophthalmol 247, 235–243 (2009). https://doi.org/10.1007/s00417-008-0944-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-008-0944-y