Abstract
Background
Sleep abnormalities have been reported in Charcot–Marie–Tooth disease (CMT), but data are scanty. We investigated their presence and correlation in a large CMT patients’ series.
Methods
Epworth Sleepiness Scale (ESS) and Pittsburgh Sleep Quality Index (PSQI) were administered to CMT patients of the Italian registry and controls. ESS score > 10 indicated abnormal daytime somnolence, PSQI score > 5 bad sleep quality. We analyzed correlation with disease severity and characteristics, Hospital Anxiety and Depression Scale (HADS), Modified Fatigue Impact Scale (MFIS), Body Mass Index, drug use.
Results
ESS and PSQI questionnaires were filled by 257 and 253 CMT patients, respectively, and 58 controls. Median PSQI score was higher in CMT patients than controls (6 vs 4, p = 0.006), with no difference for ESS score. Abnormal somnolence and poor sleep quality occurred in 23% and 56% of patients; such patients had more frequently anxiety/depression, abnormal fatigue, and positive sensory symptoms than those with normal ESS/PSQI. Moreover, patients with PSQI score > 5 had more severe disease (median CMT Examination Score, CMTES, 8 vs 6, p = 0.006) and more frequent use of anxiolytic/antidepressant drugs (29% vs 7%, p < 0.001).
Conclusions
Bad sleep quality and daytime sleepiness are frequent in CMT and correlated with anxiety, depression and fatigue, confirming that different components affect sleep. Sleep disorders, such as sleep apnea and restless leg syndrome, not specifically investigated here, are other factors known to impact on sleep quality and somnolence. CMT patients’ management must include sleep behavior assessment and evaluation of its correlated factors, including general distress and fatigue.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Charcot–Marie–Tooth disease (CMT) collects a genetically heterogeneous group of hereditary peripheral neuropathies with a common phenotype usually characterized by predominantly distal sensory and motor involvement, with muscle weakness and atrophy, frequent sensory loss, and foot deformities [1].
Sleep abnormalities significantly impact on quality of life and may have different causes. A few reports focusing on sleep abnormalities in CMT patients have been published [2,3,4,5,6], but data about daytime sleepiness and sleep quality in CMT patients are scanty.
Boentert and colleagues performed a web-based survey in 227 CMT patients and they found excessive daytime sleepiness in 31.7% of them as assessed with the Epworth Sleepiness Scale (ESS), while 79.3% of subjects were bad sleepers according to the Pittsburgh Sleep Quality Index (PSQI) [4]. Souza and coauthors administered the same scales to 16 CMT patients from a four-generation family with axonal CMT2 and found that 31% of them had abnormal sleepiness and 75% reported poor sleep quality [5].
Sleep behavior has been poorly investigated in other neuromuscular disorders with the exception of Myotonic Dystrophy (MD), where hypersomnolence was reported by 39% of 36 MD patients by Rubinsztein and colleagues, but by none of the 13 CMT patients used as diseased controls, as assessed by The Maudsley Hospital Sleep Questionnaire, which analyses sleep patterns and includes the ESS [7]. Philips et al., by employing the ESS and a sleep diary, found that both MD (n = 35) and CMT (n = 13) patients had significantly more daytime somnolence and reduced sleep quality as compared to healthy controls, as well as a higher rate of mood disorders [8]. Tielemann and coauthors reported the same percentage (44.8%) of hypersomnolence (abnormal ESS) and poor sleep quality (abnormal PSQI) in 29 MD patients [9].
ESS [10], assessing daytime sleepiness, and PSQI [11], evaluating sleep quality, are questionnaires widely used across different clinical populations, not only for the assessment of sleep disorders, but also to investigate sleep disruption in neurological disorders, such as epilepsy and Parkinson disease [12,13,14].
Previous studies on CMT were conducted on limited numbers of patients (with only one large series investigated) and correlations with clinical scales and features were only partial. Therefore, we aimed at verifying whether daytime sleepiness and bad sleep quality are really an issue in CMT and if so which are the factors that may be related to such abnormalities, including disease severity and CMT type. Specifically, we assessed sleep behavior using the ESS and PSQI questionnaires in a large series of CMT patients and analyzed correlations with disease severity, clinical characteristics, general distress, fatigue, body weight, and drug use.
Methods
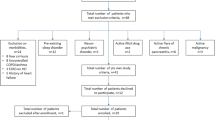
CMT patients were recruited among those adhering to the Italian National CMT registry, as recently described [15,16,17,18]. All the patients recruited in the registry were invited by an email to participate in the study and complete the online questionnaires (10 overall): 257 out of 850 filled the sleep questionnaires. The Registry collects a minimal data set of information and values of the CMT Neuropathy Score/Examination Score, CMTES/CMTNS) [19]. Data on Body Mass Index (BMI) and co-occurrence of diabetes are also gathered. Healthy controls were recruited among patients’ friends and relatives, matched as much as possible for gender and age.
This study was approved by the Ethics Committees of the Fondazione IRCCS Istituto Neurologico Carlo Besta, Milan (no. 52/2016 Date: April 2, 2014) and of the other participating centers, and has, therefore, been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Recruitment was conducted before the COVID-19 pandemic and lasted 3 years (2015–2017).
Both patients and controls were asked to complete online the Italian validated versions of the ESS and PSQI [10, 11]. A written informed consent was signed by all participants to the Registry, while an online informed consent was signed by those who completed the online questionnaires.
The ESS is a self-assessed questionnaire composed of eight items investigating somnolence. Each item is rated by a four-point (0–3) system (range 0–24, were 0 is absence of somnolence and 24 the worst score) [10]. A total score > 10 indicates abnormal somnolence, according to Johns et al. [20].
The PSQI is a self-assessed questionnaire which retrospectively measures sleep quality over a 1-month period. It contains nineteen items measuring seven different aspects of sleep (subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medications, and daytime dysfunction). Each item is rated by a four-point (0–3) system, while the global PSQI score is calculated by totaling the seven component scores with a range from 0 to 21, where lowest scores denote good sleep quality [11, 21]. A total score > 5 indicates bad sleep quality [11, 21].
Both patients and controls were asked to fill in also questionnaires concerning the presence of anxiety, depression, and general distress (Hospital Anxiety and Depression Scale, HADS, Italian version) [22] and the perception of fatigue (Modified Fatigue Impact Scale, MFIS, Italian version) [23] to explore the relation of neuropsychiatric status and fatigue with sleepiness and sleep quality. As previously described in our recent researches [15, 16], we used as cutoff scores ≥ 11 for both the HADS-A and HADS-D to define the presence of anxiety and depression, respectively, and ≥ 22 for the whole scale (HADS-T) to indicate the presence of general distress [24], while the cutoff > 38 for the MFIS scale was adopted to indicate the presence of fatigue [25]. The MFIS scale is divided into physical (PH), cognitive (C), and psychosocial (PS) subscales [23].
The questionnaire investigated also the use of antidepressants/anxiolytics and analgesics/anti-inflammatories. We considered medication users the patients taking the drugs ≥ once per week.
Statistical analysis
Participant characteristics at baseline were described in terms of absolute numbers and percentages for categorical data and means with standard deviations (SDs) and medians for continuous data. The t test, Mann–Whitney U test, Fisher’s exact test, and Spearman’s Rank-Order Correlation, were used to analyze associations between ESS and PSQI scores and type of participants (CMT patients vs controls), gender, age, disease duration, disease severity (CMTES), walking ability and/or use of orthotics, hand disability, sensory symptoms, BMI, HADS scores, MFIS score, and medication use (antidepressant/anxiolytic and analgesic/anti-inflammatory drugs). Bonferroni correction was performed, as appropriate. Throughout the statistical analysis, the significance level was set at 0.05 (significant: < 0.05).
Results
The ESS and PSQI questionnaires were filled in by 257 and 253 CMT patients, respectively, and by 58 controls. Demographic and clinical data, ESS and PSQI scores of CMT patients and controls are reported in Table 1. There was no significant difference in age and gender distribution between patients and controls for both ESS and PSQI score. Among the 257 CMT patients, 119 (46.3%) had a diagnosis of CMT1A; the other most frequent CMT types were CMTX1 (n = 21, 8.2%), CMT1B (n = 19, 7.4%), CMT2I/CMT2J (n = 14, 5.4%), CMT2A (n = 8, 3.1%), CMT4C (n = 5, 2.0%); 2 CMT1A, 1 CMT2A, and 1 CMT1B patient did not fill the PSQI questionnaire.
ESS scores
The mean and median values of ESS scores of CMT patients did not significantly differ either from controls (p = 0.252), or between CMT patients’ genders (p = 0.081) (Table 1).
Among CMT patients, 23% (60/257) had abnormal levels of daytime somnolence (ESS > 10), a rate similar to controls (21%, p = 0.732) (Table 1). Patients with abnormal daytime somnolence were more frequently females (70% vs 50%, p = 0.007), and more often reported hand disability (difficulties with buttons 68% vs 49%, p = 0.008) and positive sensory symptoms (40% vs 28%, p = 0.009) (Table 2).
As compared to CMT subjects with normal daytime somnolence (ESS score ≤ 10), they also more frequently reported anxiety/depression/general distress according to the HADS (median HADS-A 9 vs 5, median HADS-D 6 vs 3, median HADS-T 14 vs 8, p < 0.001, p = 0.007 and p < 0.001, respectively) and abnormal fatigue, according to the MFIS (median 41 vs 30, p < 0.001) (Table 2).
On the other hand, we found no difference for age, disease duration, disease severity (as assessed by the CMTES), lower limb disability, BMI, use of antidepressants/anxiolytics, and anti-inflammatory/analgesic drugs consumption (Table 2). There was no difference in daytime sleepiness according to CMT type (median ESS score: CMT1A = 7 vs other CMT types = 7, p = 0.260).
We then examined the correlations between daytime sleepiness scores and disease severity (CMTES), general distress, fatigue, BMI, sleep quality (Supplementary Table 1), and diabetes presence (n = 10). We found a slight correlation between somnolence and anxiety/depression/general distress (HADS-A, HADS-D, HADS-T, r = 0.36, r = 0.32, r = 0.37, respectively), while a stronger correlation was found between somnolence and general/physical/cognitive fatigue (r = 0.40, r = 0.49, r = 0.49, respectively).
PSQI scores
Median PSQI scores were significantly higher in CMT patients in comparison with controls (p = 0.006) (Table 1), and abnormal sleep quality (PSQI > 5) was more frequently reported by CMT patients (56%, 141/253) than controls (36%, 21/58, p = 0.008). We found no significant difference between friends and relatives in the control group, suggesting that the same environmental factors and genetic background between patients and relatives did not influence the analyses.
As compared to CMT subjects with normal sleep quality (PSQI ≤ 5), patients with abnormal sleep quality were more frequently females (p = 0.016), were significantly older (mean 49.1 vs 44.3 years of age, p = 0.002), had more severe disease as assessed by the CMTES (median 8 vs 6, p = 0.006), and more frequently reported abnormal fatigue as defined by MFIS (median 40 vs 20, p < 0.001), anxiety/depression/general distress as defined by HADS (median value: HADS-A 8 vs 4, HADS-D 5 vs 2, HADS-T 14 vs 6, respectively, p < 0.001 for all comparisons), positive sensory symptoms (45% vs 29%, p = 0.009) and anxiolytic/antidepressant drugs consumption (29% vs 7%, p < 0.001) (Table 2).
We found no difference in PSQI scores for disease duration, use of orthotics, walking and hand disability, CMT type (Supplementary Table 2), BMI, and co-occurrence of diabetes.
Notably, the component of the PSQI score, where there was a significant difference between CMT patients and healthy controls (median 2 vs 1, p < 0.001) was the fifth component, which investigates sleep disturbances. Component five of PSQI score is made up of ten sub-items, each analyzing different symptoms: cannot get to sleep within 30 min, wake up in the middle of the night or early morning, have to get up to use the bathroom, cannot breathe comfortably, cough or snore loudly, feel too cold or too hot, have bad dreams, have pain, other reasons. CMT patients more frequently reported that they could not comfortably breathe (32% vs 10%, p = 0.010), felt too cold (49% vs 22%, p = 0.002) or too hot (59% vs 20%, p = 0.007), and had nocturnal pain (70% vs 43%, p = 0.003) (Table 3).
As compared to males, female patients more frequently complained of feeling too cold (59% vs 38%, p = 0.001) and of nocturnal pain (80% vs 58%, p < 0.001).
No difference was found for the other PSQI components between patients and control.
We also examined the correlations between sleep quality and disease severity (CMTES), general distress, fatigue, sleepiness, BMI (Supplementary Table 1), and diabetes. We found a moderate correlation with PSQI for age, anxiety/depression/general distress (HADS-A, HADS-D, HADS-T, r = 0.41, r = 0.46, r = 0.47, respectively), physical/cognitive/general fatigue (MFIS-PH, MFIS-C, MFIS-T, r = 0.53, r = 0.44, r = 0.55, respectively), and daytime somnolence.
Discussion
We investigated sleep in a large series of 257 CMT patients and 58 healthy controls using the ESS and PSQI, two questionnaires widely used to investigate daytime sleepiness and sleep quality, respectively. There are only a few studies [2,3,4,5,6] investigating sleep in CMT and only one involved a large series of patients (n = 227) [4]. We found excessive daytime somnolence (ESS > 10) in 23% of CMT patients, a percentage comparable to controls and slightly lower than that found by Boentert and colleagues (31.7%) and Souza and coauthors (31% of 16 patients) [4,5,6]. Bad sleep quality (PSQI > 5) was reported by 56% of our patients, a rate higher than controls, but lower than previously reported (75.9–85.2%) [4, 5, 26]. Our CMT patients showed less daytime sleepiness in comparison with subjects with myotonic dystrophy (mean ESS score 7.3 vs 9.6, reported by Tieleman et al., and 11 by Phillips et al.), while sleep quality was comparable (mean PSQI score 6.2 vs 6.3 found by Tieleman et al.), and the percentage of bad sleepers was similar (56% vs 45% in MD patients) [8, 9].
Daytime somnolence, therefore, is an issue for almost one quarter of CMT patients and sleep quality is bad for most of them. However, which are the causes of these findings, and which are the correlations with the disease characteristics?
Sleepiness does not seem to be related to overall disease severity, though hand disability and positive sensory symptoms including pain were more frequent among CMT patients with somnolence. Female gender, anxiety and depression, and fatigue, but not age and BMI, were factors associated with daytime sleepiness.
Bad sleep quality was associated with overall disease severity and positive sensory symptoms, older age, female gender, presence of fatigue, anxiety and depression, and use of anxiolytics/antidepressants. The PSQI component 5 was the most abnormal one in CMT subjects and its analysis revealed that, with respect to controls, they more frequently could not breathe comfortably (32%), felt too cold (49%) or too hot (59%), and had nocturnal pain (70%); women reported more frequently than males feeling too cold and nocturnal pain. Notably, sleepiness and bad sleep quality were independent from CMT type.
These findings suggest that sleep abnormalities are partly related to the CMT disease itself, particularly because of pain and subjective sensory abnormalities, partly to mood disorders and fatigue, which are also frequent in CMT and linked to the condition of chronic disease as previously shown by us [16, 17] and others [4, 5, 7, 26], and likely also by the occurrence of specific sleep disorders in the CMT population as reported in previous studies [4, 5, 7, 26].
Indeed, an increased prevalence of sleep apneas, Restless Leg Syndrome (RLS), Periodic Limb Movements in Sleep (PMLS), have been reported in CMT [26]. Nocturnal cramps are another reported reason for bad quality of sleep [6].
Gemignani and coauthors were the first to report a high rate of RLS in patients with the axonal CMT2 type [27]. The study by Boentert et al. confirmed an increased prevalence of RLS in CMT (18.1%) and found that its severity was correlated with worse sleep quality [4].
Dematteis and colleagues first reported the occurrence of sleep apneas in 11 members of a large family with CMT1 [2]. In a first case–control study on 12 CMT patients and 24 disease controls, Dziewas et al. found at polysomnography an increased prevalence of obstructive sleep apneas (OSA) in CMT subjects, with a mean apnea–hypopnea index (AHI) of 10.5 (normal below 10, disease controls = 1.5) [3]. In a second larger case–control study on 61 CMT subjects and 61 matched insomniac controls, the same group confirmed an increased rate of OSA in the CMT group (37.7% vs 4.9% in controls) and a mean AHI of 9.1 (vs 1.2 in controls, normal ≤ 5), positively correlated with age and disease severity [26]. They also found a higher prevalence of RLS (40.9% vs 16.4% in controls) and PMLS (41% vs 22.9%) [26]. Sleep apneas in CMT are mainly obstructive in nature and believed to be related to involvement of pharyngeal nerves increasing the collapsibility of the upper airways; vocal cord palsy and diaphragmatic weakness are rare predisposing conditions [4, 26, 28].
An important limitation of our study is that we did not investigate the presence of OSA, RLS and PLMS, mainly because the patients had already to fill many questionnaires online (n = 11) and we feared that others would have reduced responders’ rate. Therefore, we cannot draw conclusions about the role of sleep disorders on sleepiness and bad sleep quality in our series.
In summary, we found a higher rate of bad sleepers among CMT patients, while daytime sleepiness was not increased but still was reported by 23% of the patients. We propose that there are different contributing factors, including disease severity, sensory abnormalities, nocturnal pain and cramps, mood disorders, fatigue, and, based on the literature, sleep disorders, such as OSA and RLS. Therefore, CMT patients’ management must include sleep abnormalities' assessment and evaluation of their different associated factors. Proper management of such factors may alleviate disease burden, ameliorate sleep quality, and reduce daytime sleepiness. A large multicenter international study is warranted to firmly establish a correlation between specific sleep disorders and CMT.
Data availability statement
Data relevant to the study are included in the article or uploaded as online supplemental information. Data supporting study results are deposited in an ad hoc repository and are available from the Principal Investigator (DP) to be shared anonymously on request from any qualified investigator.
Change history
21 September 2023
A Correction to this paper has been published: https://doi.org/10.1007/s00415-023-11989-4
References
Pisciotta C, Saveri P, Pareyson D (2021) Updated review of therapeutic strategies for Charcot–Marie–Tooth disease and related neuropathies. Expert Rev Neurother 21:701–713. https://doi.org/10.1080/14737175.2021.1935242
Dematteis M, Pépin JL, Jeanmart M, Deschaux C, Labarre-Vila A, Lévy P (2001) Charcot–Marie–Tooth disease and sleep apnoea syndrome: a family study. Lancet 357:267–272. https://doi.org/10.1016/S0140-6736(00)03614-X
Dziewas R, Waldmann N, Böntert M, Hor H, Müller T, Okegwo A, Ringelstein EB, Young P (2008) Increased prevalence of obstructive sleep apnoea in patients with Charcot–Marie–Tooth disease: a case control study. J Neurol Neurosurg Psychiatry 79:829–831. https://doi.org/10.1136/jnnp.2007.137679
Boentert M, Dziewas R, Heidbreder A, Happe S, Kleffner I, Evers S, Young P (2010) Fatigue, reduced sleep quality and restless legs syndrome in Charcot–Marie–Tooth disease: a web-based survey. J Neurol 257:646–652. https://doi.org/10.1007/s00415-009-5390-1
Souza CC, Hirotsu C, Neves EL, Santos LC, Costa IM, Garcez CA, Nunes PS, Antunes A (2015) Sleep pattern in Charcot–Marie–Tooth disease type 2: report of family case series. J Clin Sleep Med 11:205–211. https://doi.org/10.5664/jcsm.4526
Souza CC, Vallim JRDS, Neves ELA, Nunes PS, Costa IMPF, Barreto LCLS, Garcez CA, Araujo AAS (2022) The impact of pain and nocturnal cramps on sleep quality in Charcot–Marie–Tooth disease: a case-control study. Sleep Sci 15:41–46. https://doi.org/10.5935/1984-0063.20210025
Rubinsztein JS, Rubinsztein DC, Goodburn S, Holland AJ (1998) Apathy and hypersomnia are common features of myotonic dystrophy. J Neurol Neurosurg Psychiatry 64:510–515. https://doi.org/10.1136/jnnp.64.4.510
Phillips MF, Steer HM, Soldan JR, Wiles CM, Harper PS (1999) Daytime somnolence in myotonic dystrophy. J Neurol 246:275–282. https://doi.org/10.1007/s004150050346
Tieleman AA, Knoop H, van de Logt AE, Bleijenberg G, van Engelen BG, Overeem S (2010) Poor sleep quality and fatigue but no excessive daytime sleepiness in myotonic dystrophy type 2. J Neurol Neurosurg Psychiatry 81:963–967. https://doi.org/10.1136/jnnp.2009.192591
Vignatelli L, Plazzi G, Barbato A, Ferini-Strambi L, Manni R, Pompei F, D’Alessandro R, GINSEN (Gruppo Italiano Narcolessia Studio Epidemiologico Nazionale (2003) Italian version of the Epworth sleepiness scale: external validity. Neurol Sci 23:295–300. https://doi.org/10.1007/s100720300004
Curcio G, Tempesta D, Scarlata S, Marzano C, Moroni F, Rossini PM, Ferrara M, De Gennaro L (2013) Validity of the Italian version of the Pittsburgh Sleep Quality Index (PSQI). Neurol Sci 34:511–519. https://doi.org/10.1007/s10072-012-1085-y
Uemura Y, Nomura T, Inoue Y, Yamawaki M, Yasui K, Nakashima K (2009) Validation of the Parkinson’s disease sleep scale in Japanese patients: a comparison study using the Pittsburgh Sleep Quality Index, the Epworth Sleepiness Scale and Polysomnography. J Neurol Sci 287:36–40. https://doi.org/10.1016/j.jns.2009.09.015
Pilcher JJ, Switzer FS 3rd, Munc A, Donnelly J, Jellen JC, Lamm C (2018) Psychometric properties of the Epworth Sleepiness Scale: a factor analysis and item-response theory approach. Chronobiol Int 35:533–545. https://doi.org/10.1080/07420528.2017.1420075
Sap-Anan N, Pascoe M, Wang L, Grigg-Damberger MM, Andrews ND, Foldvary-Schaefer N (2021) The Epworth Sleepiness Scale in epilepsy: internal consistency and disease-related associations. Epilepsy Behav 121:108099. https://doi.org/10.1016/j.yebeh.2021.108099
Ambrosini A, Calabrese D, Avato FM, Catania F, Cavaletti G, Pera MC, Toscano A, Vita G, Monaco L, Pareyson D (2018) The Italian neuromuscular registry: a coordinated platform where patient organizations and clinicians collaborate for data collection and multiple usage. Orphanet J Rare Dis 13:176. https://doi.org/10.1186/s13023-018-0918-z
Bellofatto M, Bertini A, Tramacere I et al (2023) Anxiety and depression in Charcot–Marie–Tooth disease: data from the Italian CMT national registry. J Neurol 270:394–401. https://doi.org/10.1007/s00415-022-11365-8
Bellofatto M, Bertini A, Tramacere I et al (2023) Frequency, entity and determinants of fatigue in Charcot–Marie–Tooth disease. Eur J Neurol 30:710–718. https://doi.org/10.1111/ene.15643
Pisciotta C, Bertini A, Tramacere I et al (2023) Clinical spectrum and frequency of Charcot–Marie–Tooth disease in Italy: data from the national CMT registry. Eur J Neurol 30:2461–2470. https://doi.org/10.1111/ene.15860
Murphy SM, Herrmann DN, McDermott MP, Scherer SS, Shy ME, Reilly MM, Pareyson D (2011) Reliability of the CMT neuropathy score (second version) in Charcot–Marie–Tooth disease. J Peripher Nerv Syst 16:191–198. https://doi.org/10.1111/j.1529-8027.2011.00350.x
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14:540–545. https://doi.org/10.1093/sleep/14.6.540
Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28:193–213. https://doi.org/10.1016/0165-1781(89)90047-4
Costantini M, Musso M, Viterbori P, Bonci F, Del Mastro L, Garrone O, Venturini M, Morasso G (1999) Detecting psychological distress in cancer patients: validity of the Italian version of the Hospital Anxiety and Depression Scale. Support Care Cancer 7:121–127. https://doi.org/10.1007/s005200050241
Kos D, Kerckhofs E, Carrea I, Verza R, Ramos M, Jansa J (2005) Evaluation of the Modified Fatigue Impact Scale in four different European countries. Mult Scler 11:76–80. https://doi.org/10.1191/1352458505ms1117oa
Singer S, Kuhnt S, Götze H, Hauss J, Hinz A, Liebmann A, Krauss O, Lehmann A, Schwarz R (2009) Hospital anxiety and depression scale cutoff scores for cancer patients in acute care. Br J Cancer 100:908–912. https://doi.org/10.1038/sj.bjc.6604952
Flachenecker P, Kümpfel T, Kallmann B, Gottschalk M, Grauer O, Rieckmann P, Trenkwalder C, Toyka KV (2002) Fatigue in multiple sclerosis: a comparison of different rating scales and correlation to clinical parameters. Mult Scler 8:523–526. https://doi.org/10.1191/1352458502ms839oa
Boentert M, Knop K, Schuhmacher C, Gess B, Okegwo A, Young P (2014) Sleep disorders in Charcot–Marie–Tooth disease type 1. J Neurol Neurosurg Psychiatry 85:319–325. https://doi.org/10.1136/jnnp-2013-305296
Gemignani F, Marbini A, Di Giovanni G, Salih S, Terzano MG (1999) Charcot–Marie–Tooth disease type 2 with restless legs syndrome. Neurology 52:1064–1066. https://doi.org/10.1212/wnl.52.5.1064
Shy ME (2008) Obstructive sleep apnoea and CMT1A: answers and more questions. J Neurol Neurosurg Psychiatry 79:743–744. https://doi.org/10.1136/jnnp.2008.145797
Acknowledgements
We are gratefully indebted with all the patients and their families and with controls for their active participation in the study and to ACMT-Rete, Associazione del Registro, and Telethon-Italy Foundation for supporting the research and the Registry. We also thank the other members of the Italian CMT Network listed in the Appendix.
MB, AB, EC, PS, CPi, and DP are members of the Inherited Neuropathy Consortium RDCRN.
LG, FM, AS, MG, SCP, LP, EC, PS, ST, MR, AM, CPi, and DP are members of the European Reference Network for Rare Neuromuscular Diseases (ERN EURO-NMD).
Italian CMT Network, other members: Giulia Schirinzi: Fondazione IRCCS Istituto Neurologico Carlo Besta, Milan: Clinical assessor Physiotherapist: Data collection. Maria Montesano: Fondazione IRCCS Istituto Neurologico Carlo Besta, Milan: Clinical assessor Physiotherapist: Data collection. Sara Nuzzo: Fondazione IRCCS Istituto Neurologico Carlo Besta, Milan: Administrative person: Study organization. Francesca Oggiano: Fondazione IRCCS Istituto Neurologico Carlo Besta, Milan: Administrative person: Study organization. Daniela Calabrese: Fondazione IRCCS Istituto Neurologico Carlo Besta, Milan: Pharmacist: Study organization Data management. Chiara Gemelli: University of Genoa: Clinical assessor: Data collection. Yuri Falzone: IRCCS Ospedale San Raffaele, Milan: Clinical assessor: Acquisition of data. Emanuele Spina: University Federico II of Naples: Clinical assessor: Data collection. Maria Longo: University of Messina: Psychologist: Data collection. Giuseppe Occhipinti: Università di Messina: Clinical assessor: Data collection. Giacomo Iabichella: Università di Messina: Clinical assessor: Data collection. Stefania Barone: Università Magna Grecia: Clinical assessor: Data collection.
Funding
Study funded by Telethon-Italy Foundation Grant GUP13006 and partially by Italian Ministry of Health (RRC).
Author information
Authors and Affiliations
Consortia
Contributions
All authors reported in this manuscript had contributed to data collection and had revised the manuscript. DP had designed and conceptualized this study. IT and AB had provided statistical analyses and data management. MB and DP wrote the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
GMF acknowledges donations from Pfizer to support research activities of his Research Unit, financial support from Akcea, Kedrion, Pfizer for participation in national and international meetings and from Akcea, Alnylam and Pharnext for participation in Advisory Boards; MG acknowledges donations from Sanofi Genzyme to support research activities of her Research Unit, financial support from Alnylam and Sanofi Genzyme for participation in national and international Meetings, participation in Advisory Board of Pfizer, speaker honorarium from Sanofi Genzyme; AM acknowledges financial support from Pfizer, Alnylam and Akcea for participation in national and international meetings, participation in Advisory Board of Pfizer, Alnylam and Akcea; GV acknowledges donations from Pfizer and PTC to support research activities and participation in Advisory Board of Pfizer, Alnylam, Akcea and Pharnext; DP acknowledges donations from Pfizer, LAM Therapeutics and Acceleron to support research activities of his Research Unit, financial support from Pfizer, Alnylam and Kedrion for participation in national and international meetings, participation in Advisory Board of Inflectis, Alnylam, Akcea, Arvinas, Augustine Tx, DTx, speaker honorarium from Alnylam. MB, AB, IT, FM. AS, LS, TC, SCP, MS, IA, LP, CP. DC, PS, AQ, PV, ST, LG, MR, AM, SP, GDD, CP report no disclosure.
Additional information
The original online version of this article was revised due to a retrospective Open Access order.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Bellofatto, M., Gentile, L., Bertini, A. et al. Daytime sleepiness and sleep quality in Charcot–Marie–Tooth disease. J Neurol 270, 5561–5568 (2023). https://doi.org/10.1007/s00415-023-11911-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-023-11911-y