Abstract
Objectives
To separate posterior-circulation stroke (PCS) and vestibular-neuritis (VN) using quantitative vestibular tests.
Methods
Patients were prospectively recruited from the emergency room within 72 h of presentation. Video-nystagmography (VNG), three-dimensional video head-impulse testing (vHIT), vestibular-evoked myogenic potentials (VEMPs), and subjective visual-horizontal (SVH) were performed.
Results
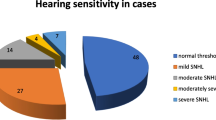
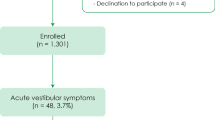
There were 128 PCS and 134 VN patients. Common stroke-territories were: posterior–inferior cerebellar artery, basilar-perforators, multi-territory and anterior–inferior cerebellar artery (41.4%, 21.1%, 14.1%, 7.8%). VN included superior, inferior and pan-neuritis (53.3%, 4.2%, and 41.5%). Most VN and stroke patients presented with acute vestibular syndrome (96.6%, 61.7%). In VN, we recorded horizontal (98.5%) or vertical/torsional spontaneous nystagmus (1.5%) and in PCS, absent-nystagmus (53.9%), horizontal (32%) or vertical/torsional (14.1%) nystagmus. The mean slow-phase velocity of horizontal nystagmus was faster in VN than PCS (11.8 ± 7.2 and 5.2 ± 3.0°/s, p < 0.01). Ipsilesional horizontal-canal (HC) vHIT-gain was lower in VN than in stroke (0.47 ± 0.24, 0.92 ± 0.20, p < 0.001). Ipsilesional catch-up saccades occurred earlier, and their amplitude, prevalence, and velocity were greater in VN than PCS (p < 0.01). Ipsilesional SVH deviation > 2.5° occurred more often in VN than in stroke (97.6% and 24.3%, p < 0.01). Abnormal bone-conducted ocular-VEMP asymmetry ratio was more common in VN than PCS (50% and 14.4%, p < 0.01). Using the ten best discriminators (VNG, vHIT, SVH, and oVEMP metrics), VN was separated from PCS with a sensitivity of 92.9% and specificity of 89.8%. Adding VNG and vHIT to the bedside head-impulse-nystagmus-and-test-of-skew (HINTS) test enhanced sensitivity and specificity from 95.3% and 63.4% to 96.5% and 80.6%.
Conclusion
Quantitative vestibular testing helps separate stroke from vestibular neuritis and, when used, could improve diagnostic accuracy in the emergency room.




Similar content being viewed by others
Data availability
Anonymized data will be shared by request from any qualified investigator.
References
Kerber KA (2020) Acute vestibular syndrome. Semin Neurol 40:59–66
Baloh RW (2003) Clinical practice. Vestibular neuritis. N Engl J Med 348(11):1027–1032
Thömke F, Hopf HC (1999) Pontine lesions mimicking acute peripheral vestibulopathy. J Neurol Neurosurg Psychiatry 66(3):340–349
Machner B, Choi JH, Neumann A, Trillenberg P, Helmchen C (2021) What guides decision-making on intravenous thrombolysis in acute vestibular syndrome and suspected ischemic stroke in the posterior circulation? J Neurol 268(1):249–264
Kattah JC, Talkad AV, Wang DZ, Hsieh YH, Newman-Toker DE (2009) HINTS to diagnose stroke in the acute vestibular syndrome: three-step bedside oculomotor examination more sensitive than early MRI diffusion-weighted imaging. Stroke 40(11):3504–3510
Vanni S, Pecci R, Casati C, Moroni F, Risso M, Ottaviani M et al (2014) STANDING, a four-step bedside algorithm for differential diagnosis of acute vertigo in the emergency department. Acta Otorhinolaryngol Ital 34(6):419–426
Gerlier C, Hoarau M, Fels A, Vitaux H, Mousset C, Farhat W et al (2021) Differentiating central from peripheral causes of acute vertigo in an emergency setting with the HINTS, STANDING, and ABCD2 tests: a diagnostic cohort study. Acad Emerg Med 2:2
Nham B, Reid N, Bein K, Bradshaw AP, McGarvie LA, Argaet EC et al (2021) Capturing vertigo in the emergency room: three tools to double the rate of diagnosis. J Neurol 2:2
Calic Z, Nham B, Bradshaw AP, Young AS, Bhaskar S, D’Souza M et al (2020) Separating posterior-circulation stroke from vestibular neuritis with quantitative vestibular testing. Clin Neurophysiol 2:2
Halmagyi GMCL, MacDougall HG, Weber KP, McGarvie LA, Curthoys IS (2017) The video head impulse test. Front Neurol 8:258
MacDougall HG, Weber KP, McGarvie LA, Halmagyi GM, Curthoys IS (2009) The video head impulse test: diagnostic accuracy in peripheral vestibulopathy. Neurology 73(14):1134–1141
Fife TDCJ, Kerber KA, Brantberg K, Strupp M, Lee H, Walker MF, Ashman E, Fletcher J, Callaghan B, Gloss DS (2017) 2nd practice guideline: cervical and ocular vestibular evoked myogenic potential testing report of the guideline development, dissemination, and implementation subcommittee of the American academy of neurology. Neurology 89(22):2288–2296
Karlberg M, Aw ST, Halmagyi GM, Black RA (2002) Vibration-induced shift of the subjective visual horizontal: a sign of unilateral vestibular deficit. Arch Otolaryngol Head Neck Surg 128(1):21–27
Furman JM. Vestibular laboratory testing. Aminoff's electrodiagnosis in clinical neurology, 6th edn. ScienceDirect; 2012.
Taylor RL, McGarvie LA, Reid N, Young AS, Halmagyi GM, Welgampola MS (2016) Vestibular neuritis affects both superior and inferior vestibular nerves. Neurology 87(16):1704–1712
Mantokoudis GSTA, Wozniak A, Eibenberger K, Kattah JC, Guede CI et al (2015) VOR gain by head impulse video-oculography differentiates acute vestibular neuritis from stroke. Otol Neurotol 36:457–465
Pollak L, Kushnir M, Stryjer R (2006) Diagnostic value of vestibular evoked myogenic potentials in cerebellar and lower-brainstem strokes. Clin Neurophysiol 36(4):227–233
Choi SY, Lee SH, Kim HJ, Kim JS (2014) Impaired modulation of the otolithic function in acute unilateral cerebellar infarction. Cerebellum 13(3):362–371
Pogson JMTR, McGarvie L, Bradshaw AP, D’Souza M, Halmagyi GM, Welgampola MS (2019) The human vestibulo-ocular reflex and saccades: normal subjects and the effect of age. J Neurophysiol 2:2
Young ASLC, Bradshaw AP, MacDougall HG, Black DA, Halmagyi GM, Welgampola MS (2019) Capturing acute vertigo: a vestibular event monitor. Neurology 92:e1–e11
Yeung JC, Heley S, Beauregard Y, Champagne S, Bromwich MA (2015) Self-administered hearing loss screening using an interactive, tablet play audiometer with ear bud headphones. Int J Pediatr Otorhinolaryngol 79(8):1248–1252
Choi JY, Kim HJ, Kim JS (2018) Recent advances in head impulse test findings in central vestibular disorders. Neurology 90(13):602–612
Magliulo G, Iannella G, Gagliardi S, Re M (2015) A 1-year follow-up study with C-VEMPs, O-VEMPs and video head impulse testing in vestibular neuritis. Eur Arch Otorhinolaryngol 272(11):3277–3281
Chen L, Todd M, Halmagyi GM, Aw S (2014) Head impulse gain and saccade analysis in pontine-cerebellar stroke and vestibular neuritis. Neurology 83(17):1513–1522
Janky KL, Patterson J, Shepard N, Thomas M, Barin K, Creutz T et al (2018) Video head impulse test (vHIT): the role of corrective saccades in identifying patients with vestibular loss. Otol Neurotol 39(4):467–473
Choi JYKH, Kim JS (2018) Recent advances in head impulse test fi ndings in central vestibular disorders. Neurology 2:2
Ohle R, Montpellier RA, Marchadier V, Wharton A, McIsaac S, Anderson M et al (2020) Can emergency physicians accurately rule out a central cause of vertigo using the HINTS exam? A systematic review and meta-analysis. Acad Emerg Med 2:2
Korda A, Carey JP, Zamaro E, Caversaccio MD, Mantokoudis G (2020) How good are we in evaluating a bedside head impulse test? Ear Hear 41(6):1747–1751
Korda A, Zamaro E, Wagner F, Morrison M, Caversaccio MD, Sauter TC et al (2021) Acute vestibular syndrome: is skew deviation a central sign? J Neurol 2:2
Cnyrim CD, Newman-Toker D, Karch C, Brandt T, Strupp M (2008) Bedside differentiation of vestibular neuritis from central “vestibular pseudoneuritis.” J Neurol Neurosurg Psychiatry 79(4):458–460
Kremmyda O, Kirchner H, Glasauer S, Brandt T, Jahn K, Strupp M (2012) False-positive head-impulse test in cerebellar ataxia. Front Neurol 3:162
Riera-Tur L, Caballero-Garcia A, Martin-Mateos AJ, Lechuga-Sancho AM (2022) Efficacy of the subjective visual vertical test performed using a mobile application to detect vestibular pathology. J Vestib Res 32(1):21–27
Halmagyi GM, McGarvie LA, Strupp M (2020) Nystagmus goggles: how to use them, what you find and what it means. Pract Neurol 20(6):446–450
Korda A, Wimmer W, Zamaro E, Wagner F, Sauter TC, Caversaccio MD et al (2022) Videooculography “HINTS” in acute vestibular syndrome: a prospective study. Front Neurol 13:920357
Morrison M, Korda A, Zamaro E, Wagner F, Caversaccio MD, Sauter TC et al (2021) Paradigm shift in acute dizziness: is caloric testing obsolete? J Neurol 2:2
Funding
This research was supported by the Garnett Passe and Rodney Williams Memorial Foundation and the National Health and Medical Research Council of Australia.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
B. Nham, C. Wang, N. Reid, Z. Calic, BYC Kwok, D. A. Black, and A. P. Bradshaw have no disclosures relevant to this manuscript. G.M. Halmagyi is an unpaid consultant for Otometrics. M. S. Welgampola have no disclosures relevant to this manuscript.
Ethics and consent
This study received local ethics committee approval for human participants, and written informed consent was obtained from all participants as per the Helsinki Declaration of 1964.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Nham, B., Wang, C., Reid, N. et al. Modern vestibular tests can accurately separate stroke and vestibular neuritis. J Neurol 270, 2031–2041 (2023). https://doi.org/10.1007/s00415-022-11473-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-022-11473-5