Abstract
Background
Accumulating evidence suggests that spontaneous intracerebral hemorrhage (ICH) is associated with a reactive neuroinflammatory response. However, it remains unclear if circulating inflammatory biomarkers are associated with adverse outcomes in ICH. To address this knowledge gap, we conducted a cohort study using a prospectively maintained stroke register in the United Kingdom to assess the prognostic value of admission inflammatory biomarkers in ICH.
Methods
The Norfolk and Norwich Stroke and TIA Register recorded consecutive ICH cases. The primary exposures of interest were elevation of white cell count (WCC; > 10 × 109/L), elevation of c-reactive protein (CRP; > 10 mg/L), and co-elevation of both biomarkers, at the time of admission. Modified Poisson and Cox regressions were conducted to investigate the relationship between co-elevation of WCC and CRP at admission and outcomes following ICH. Functional outcome, multiple mortality timepoints, and length of stay were assessed.
Results
In total, 1714 ICH cases were identified from the register. After adjusting for covariates, including stroke-associated pneumonia, co-elevation of WCC and CRP at admission was independently associated with significantly increased risk of poor functional outcome (RR 1.08 [95% CI 1.01–1.15]) and inpatient mortality (RR 1.21 [95% CI 1.06–1.39]); and increased 90-day (HR 1.22 [95% CI 1.03–1.45]), and 1-year mortality (HR 1.20 [95% CI 1.02–1.41]). Individual elevation of WCC or CRP was also associated with poor outcomes.
Conclusions
Elevated inflammatory biomarkers were associated with poor outcomes in ICH. This study indicates that these readily available biomarkers may be valuable for prognostication and underscore the importance of inflammation in ICH.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Spontaneous intracerebral hemorrhage (ICH) continues to be associated with high rates of morbidity and mortality, and there remains no definitive treatment beyond supportive care[1, 2]. Accumulating experimental evidence demonstrates that intracerebral hemorrhage drives a microglia and T-cell-mediated inflammatory reaction in the brain[3]. This inflammatory response is associated with perihematomal oedema, cytokine release, and breakdown of the blood–brain barrier with resultant leukocyte influx[4], and may contribute to poor outcomes following ICH.
The extent of inflammation has been shown to correlate with ICH severity experimentally [5, 6], suggesting that clinical markers of inflammation may be associated with adverse outcomes after ICH. However, studies on this topic remain limited to date and, critically, have not accounted for the potential confounding arising from stroke-associated pneumonia (SAP) [7, 8]. Additionally, targeting post-hemorrhagic inflammation is an appealing avenue for the development of future treatments. Such treatments may require selection of appropriate candidates for intervention: inflammatory biomarkers may therefore provide a rapid and readily accessible means of triage.
There is, therefore, a need to understand the relationship between clinically identifiable inflammation and subsequent outcomes in ICH populations. To address this, we performed a cohort study using a prospectively maintained stroke register of consecutive admissions in the United Kingdom to investigate the relationship between elevated inflammatory blood biomarkers at the time of admission and outcomes in ICH.
Methods
Database and patient identification
The Norfolk and Norwich Stroke and TIA register is a prospectively maintained stroke register in the United Kingdom that records all stroke admissions to the Norfolk and Norwich University Hospital, which had a catchment of approximately 900,000 in 2017. The Newcastle and Tyneside National Health Service and Research Ethics Committee provided ethical approval for this database (17/NE/0277), providing approval for anonymized research studies, and waiving the requirement for individual patient consent. There are no other tertiary care centers in Norfolk County, ensuring a high percentage capture of stroke cases. Full data collection methods have been previously published in detail [9]. Data from multiple sources are combined for each patient to provide a wide range of variables for each ICH case; specialist nurses determine the pre-stroke modified Rankin Score (mRS) for each patient. Patients were included if they were admitted with a diagnosis of spontaneous non-traumatic ICH and had complete follow-up data between inclusion in the study and the end of the follow-up period in June 2017.
Data extraction and exposures
Baseline patient demographics were extracted from the database, along with relevant covariates and comorbidities. Data extracted were as follows: age, sex, pre-ICH mRS, Oxford Community Stroke Project classification (OCSP), prescriptions at admission (anticoagulants and antiplatelets), and stroke-associated pneumonia during admission (SAP; defined as any pneumonia within 7 days of admission[10]). All pre-ICH comorbidities recorded in the database were extracted using the International Classification of Disease-tenth edition (ICD-10): asthma (J45), atrial fibrillation (I48), previous cerebral infarction (I63), coronary heart disease (I20–I25), congestive heart failure (I50), chronic kidney disease (N18), chronic obstructive pulmonary disorder—COPD (J40–J44, J47), dementia (F01–F05), diabetes mellitus (E10–E14), hyperlipidemia (E78), hypertension (I10–I15), liver disease (K70–K77), malignancy (C00–C97), peptic ulcer disease (K25–K28), peripheral vascular disease (I73.9), previous subarachnoid (SAH) or intracerebral hemorrhage (I60–I61), and rheumatoid arthritis/connective tissue disease (M32, M34, M332, M053, M058, M059, M060, M063, M069, M050, M052, M051, M353).
Admission values for undifferentiated white cell count (WCC), and C-reactive protein (CRP) blood tests were extracted. The primary exposure of interest was co-elevation of WCC (> 10 × 109/L) and CRP (> 10 mg/L) at the time of admission. These thresholds were selected as they have been validated for clinical purposes at the study center, defined as the upper bound for the normal range [11, 12]. A combined exposure using both biomarkers was used to provide a more comprehensive assay of the inflammatory state when compared with a single biomarker in isolation. Analyses of the associations of isolated elevated WCC (> 10 × 109/L) and elevated CRP (> 10 mg/L) were also performed.
Outcomes
The following outcomes were recorded: mortality, functional outcome, and length of stay. Mortality was assessed at multiple timepoints: inpatient mortality, 90-day mortality, and 1-year mortality. Functional outcome was assessed at discharge and recorded using the modified Rankin Scale. Functional outcome was dichotomized into good functional outcome (mRS 0–2 at discharge) and poor functional outcome (mRS 3–6 at discharge). Prolonged length of stay was defined as hospitalization > 14 days. Prolonged hospitalization is an important outcome to ascertain, as it provides useful information for service provision including economic considerations. This is particularly important in the UK NHS setting of universal healthcare in which the ability to estimate the length of hospitalization based on clinical characteristics is essential for to ensure equitable allocation of resources.
Missing data and exclusions
Figure 1 summarizes identification of patients from the register. Missing data were handled in a predefined manner. Variables with < 5% missing data (WCC, LoS) were analyzed on a complete-case-analysis basis, while variables with ≥ 5% (mRS before ICH, mRS at discharge, CRP on admission, OCSP classification, and NIHSS) were imputed. Out of 1897 ICH admissions extracted from the register, the following patients were excluded: those with missing WCC (n = 45) or LoS (n = 3) data, those for whom the first measurement of WCC (n = 85) or CRP (n = 111) recorded in the registry occurred after discharge, and those with extreme or implausible WBC > 30 × 109/L (n = 8), resulting in an included population of 1714 patients. Figure 1 also summarizes key variables with missing data after the application of the selection criteria: mRS before incident ICH (7.29% missing), CRP on admission (17.68% missing), mRS at discharge (20.95% missing), OCSP classification (21.53% missing), and NIHSS (86.35% missing). Missing data analysis revealed that patients with missing data on these variables were more significantly likely to have higher WCC, less likely to have pre-existing comorbidities on admission, and more likely to die after stroke (Tables S1.1–1.5). Data missingness was therefore likely to depend on observed factors, and therefore deemed likely to be missing-at-random[13]. A multiple imputation by chained equation (MICE) algorithm with 20 iterations was therefore implemented to impute the missing data. All variables were imputed using predictive mean matching drawing from five nearest neighbors. Conditional imputation was employed for mRS at discharge, only imputing this variable for patients discharged alive and restricting the imputation values to 0–5. Age, sex, prevalent comorbidities, SAP, admission anticoagulant and antiplatelet medications were used as predictors. A separate MICE algorithm was employed for the variables utilized for the long-term mortality analyses, replicating the methodology above, but also including the Nelson–Aalen estimator as a predictor.
As the NIHSS score was only routinely recorded in the register from 2015, there was a high degree of missingness for this variable. Therefore, sensitivity analyses replicating all the main regression models additionally adjusting for the imputed NIHSS were conducted. These did not show any meaningful differences in results (Tables 2, 3).
Statistical analyses
Statistical analyses were performed using STATA 14.1 (STATA Corporation, 2015). As CRP was one of the imputed variables and was also used to define the combined exposure variable, descriptive statistics comparing the patient population characteristics by defined exposure were performed on the 20 imputed datasets obtained after MICE. Table 1 in the main manuscript details the descriptive statistics performed for one of the imputed datasets, while the other 19 are presented in Supplementary Tables (Tables S2.1–S2.20). For all 20 imputed datasets, the Pearson’s Chi-square test was used to compare categorical variables. The independent t-test was used to compare normally distributed continuous variables (age), and the Mann–Whitney U test to compare non-normally distributed continuous variables (NIHSS score, white cell count, C-reactive protein, and length of stay). A significance threshold of P < 0.05 was used.
Poisson regression models with a robust variance estimator were used to determine risk ratios for the in-hospital outcomes: functional outcome, mortality, and prolonged length of stay. The use of the robust variance estimator allows the relaxation of the assumption that the outcome follows a Poisson distribution and therefore allows the derivation of risk ratios with appropriate standard errors for an outcome following a binomial distribution [14, 15]. This method was chosen as an alternative to the traditional logistic regressions to yield risk ratios that are directly comparable to the hazard ratios for long-term mortality yielded by the Cox regressions [14]. Additional analyses of the in-hospital outcomes employing logistic regressions were performed to yield odds ratios directly comparable to previous and future literature employing logistic regressions (Table S3). Cox regressions were performed for 90-day, and 1-year mortality. Satisfaction of the proportional hazards assumption was confirmed in all models by visual inspection of log-negative-log survival curves. Risk ratios (RR), hazard ratios (HR), and odds ratios (OR) are reported alongside corresponding 95% confidence intervals (CI).
Three sequentially adjusted regression models were constructed for each model described above: a primary model that adjusted for all covariates and comorbidities except SAP and NIHSS score, an SAP-adjusted model, and an NIHSS score-adjusted model (also adjusted for SAP). Dedicated sensitivity analyses excluding all cases of SAP were also performed. A Kaplan–Meier survival analysis was performed to compare death between groups using a log-rank test.
Finally, a further Cox model was constructed to evaluate the relationship between WCC and CRP as continuous variables and the selected adverse outcomes. This adjusted for all the confounders listed above including SAP and NIHSS. The Akaike Information Criterion (AIC) was calculated for the linear model and for nonlinear models parametrized using restricted cubic spline (RCS) with varying degrees of freedom (df = 2 to df = 7) to determine the best fitting model delineating the association between WCC/CRP and long-term mortality. RCS were constructed using the Stata command rcsgen [16]. Where an RCS model had a lower AIC than the linear model, the likelihood-ratio test was used to confirm that this RCS model provides a better fit for the data than the linear model. WCC was therefore parametrized using RCS with 2 degrees of freedom (1 internal knot), while CRP was parametrized using a linear model. The reference point (HR = 1) for the WCC HR function was chosen as the minimum value of this function, corresponding to a WCC value of 7.0 × 109/L in the main analyses and 5.8 × 109/L in the sensitivity analyses excluding SAP patients. The satisfaction of the proportional hazards assumption for these models was verified using Schoenfeld residuals. The resulting hazard ratios characterizing the association between WCC/CRP and long-term mortality were therefore assumed to remain constant throughout the follow-up period.
As the interval from admission to measurement of inflammatory biomarkers varied, we performed sensitivity analyses replicating the main analyses, but excluding those patients whose biomarkers were sampled > 48 h after admission. These did not show any meaningful differences in results (Supplementary Tables S6 and S7).
Results
Cohort characteristics
A total of 1714 patients with ICH were identified following exclusions (Fig. 1). Table 1 displays the cohort characteristics and outcomes of included cases, performed on one of the imputed datasets resulting from the MICE algorithm. Descriptive statistics of the other 19 imputed datasets are presented in the Supplementary Tables (Tables S2.1–S2.20). The mean age (± SD) of patients was 76.05 (± 12.25); 49.82% of patients were male. The distribution of OCSP classifications varied between groups, with a higher proportion of TACS in the inflammatory biomarker group (p < 0.001). There was a lower proportion of male patients in the elevated inflammatory biomarkers cohort than in the control cohort (44.92% vs 51.69.7%, P = 0.012). Patients with elevated inflammatory biomarkers were more likely to have coronary heart disease (22.88% vs 17.63%, P = 0.013), and congestive heart failure (10.38% vs 6.92%, P = 0.018). Patients in the elevated inflammatory biomarkers cohort were more likely to be diagnosed with stroke associated pneumonia during admission than controls (15.89% vs 9.58%, P < 0.001).
Of the included patients, 472 (27.54%) had elevated inflammatory biomarkers at admission. The median WCC and CRP in the non-inflammatory group were 8.70 × 109/L and 7.00 mg/L respectively; in the inflammatory cohort, they were 12.95 × 109/L and 27.00 mg/L, respectively.
Functional outcome
After adjusting for confounders, modified Poisson regression revealed that elevated inflammatory biomarkers at admission were associated with poor functional outcome (RR 1.09 [95% CI 1.02–1.16]) (Table 2, Fig. 2). This association was observed in the SAP-adjusted regression model (RR 1.08 [95% CI 1.01–1.15]) and in the NIHSS-adjusted regression model (RR 1.08 [95%CI 1.01–1.15]). In the sensitivity analyses excluding all cases of stroke associated pneumonia, as well as those excluding all patients whose biomarkers were sampled > 48 h after admission, elevated inflammatory biomarkers continued to be associated with poor functional outcomes (Tables S4 and S6).
Mortality
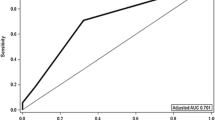
After adjusting for all confounders including SAP and NIHSS, elevated inflammatory biomarkers were associated with death during admission (RR 1.21 [95% CI 1.06–1,39]), death at 90 days (HR 1.22 [95% CI 1.03–1.45]), and death at 1 year (HR 1.20 [95% CI 1.02–1.41]) (Tables 2, 3). In a sensitivity analysis excluding all SAP cases, elevated inflammatory biomarkers continued to be associated with death during admission (Table S4). In contrast, sensitivity analyses excluding all SAP cases did not show an association between co-elevation of inflammatory biomarkers on admission and post-discharge mortality at 90 days or 365 days (Table S5). Kaplan–Meier survival analysis revealed that patients with elevated inflammatory biomarkers died earlier and more frequently than their counterparts (P < 0.001 by log rank test; Fig. 3).
Figure 4 shows the results of the Cox proportional hazards model detailing the association between WCC and CRP as continuous variables and long-term mortality. Relative to a WCC of a 7.0 × 109/L, there was no association between WCC ranging between 0 and 13.2 × 109/L and long-term mortality. Nevertheless, compared to a WCC of a 7.0 × 109/L, WCC values ranging between 13.3 (HR 1.16 [95% CI 1.00–1.35]) and 25.0 × 109/L (HR 2.90 [95% CI 1.95–4.31]) were associated with statistically significant excess risk of long-term mortality. Increasing CRP was significantly associated with a linear increase in excess long-term mortality (HR for 1-point increase 1.0019 [95% CI 1.0003–1.0035]; HR for 10-point increase 1.0194 [1.0034–1.0358]; HR for 50-point increase 1.1013 [1.017–1.1923]). In sensitivity analyses excluding all patients whose biomarkers were sampled > 48 h after admission, elevated inflammatory biomarkers continued to be associated with mortality at all timepoints assessed (Supplementary Tables S6 and S7).
Results of multivariable Cox regressions assessing the association of white blood cell count (WCC) and C-reactive protein (CRP) as continuous variables, and long-term mortality after intracerebral hemorrhage. As the relationship between WCC and mortality did not follow a linear pattern, this was parametrized using restricted cubic splines with 1 internal knot. The reference point (HR = 1) for the HR function was chosen as the minimum value of the function, corresponding to a WCC value of 7.0 × 109/L. The relationship between CRP and mortality followed a linear pattern and was modelled accordingly: HR (95% confidence interval) for 50-point increase in CRP = 1.10 (1.02–1.19). Hazard ratios and respective 95% confidence intervals are represented by the blue line with grey shadowing. The dotted red line represents the reference line (HR = 1). The overlaying blue bar chart displays the distribution of each inflammatory marker in the included cohort. Model adjusted for age, sex, Oxfordshire Community Stroke Project classification, pre-morbid modified Rankin Scale, prevalent comorbidities on admission, stroke-associated pneumonia, admission antiplatelet and anticoagulant medication, and the National Institute of Health Stroke Scale
Length of stay
After adjusting for all confounders in the modified Poisson regression model, elevated inflammatory biomarkers were not associated with an increased length of stay (RR 1.11 [95% CI 0.96–1.28]). Sensitivity analyses excluding all SAP cases showed similar results (Table S4).
Discussion
In this large cohort study using a prospectively maintained stroke register, co-elevation of WCC and CRP at admission predicted poor outcomes in ICH: patients were more likely to have a poor functional outcome, die during admission, be dead at 90 days, and be dead at 1 year. Critically, these associations were maintained after adjusting for stroke-associated pneumonia. This study therefore indicates that these readily available inflammatory biomarkers may be useful prognosticators in the context of ICH and underscore the importance of reactive inflammation in the pathophysiology of this disease.
A growing body of evidence reveals there is a reactive inflammatory process following ICH [3, 17], with experimental studies demonstrating that a wide variety of inflammatory processes occur, including infiltration of white cells [18], activation of microglia [19], and the release of inflammatory cytokines [6]. Notably, elevation of interleukin-6- the primary inducer of CRP [20]—has been found in animal and human studies [21]. These studies are consistent with the findings of this study: that there is considerable inflammation immediately following ICH. More specifically, given that experimental data demonstrate the local infiltration of leukocytes and activation of inflammatory cytokines in ICH, it is logical that such phenomena could be detected peripherally and be used for prognostication, as suggested by our results. This study further emphasizes the important role that inflammation plays in ICH.
Studies have previously reported that the extent of inflammation correlates with various measures of stroke magnitude [6, 22, 23], suggesting that inflammatory biomarkers may in turn correlate with clinical outcomes. This was the case in this study: patients with elevated inflammatory biomarkers had a higher risk of poor functional outcome and death at multiple timepoints. Accordingly, these inflammatory biomarkers may be useful for outcome prognostication. To date, however, the prognostic value of inflammatory biomarkers has been incompletely investigated, with small samples sizes and varying study thresholds limiting generalizability. A number of studies investigating a variety of white blood cell measurements in ICH have reported linear associations between increasing white cells and poor outcomes [7, 8], while three studies have reported that rising CRP is linearly associated with poor outcomes: these studies do not use discrete thresholds for denoting limiting the clinical applicability of these findings [24,25,26]. Notably, the present study cohort is larger than those of these previous analyses combined, providing greater statistical power to support these results. Notably, elevated inflammatory biomarkers were not associated with prolonged length of stay in this analysis after adjusting for covariates in regression models: it may be that the myriad factors that determine discharge are independent of the effects of post-ICH inflammation.
This study has several strengths. The protocol of the stroke register used for this study provides near-complete follow-up data capture and is prospectively maintained for research purposes, ensuring that data are systematically recorded. By adjusting for many covariates, including stroke-associated pneumonia, the risk of confounding is further reduced: incident pneumonia will not only cause an inflammatory marker increase that is independent of ICH-driven inflammation, but is also more likely to be associated with death and prolonged hospitalization. As biomarkers were sampled at varying timepoints after admission, this is particularly important. Additionally, this study uses clinically validated biomarker thresholds for determining study groups and considers both the combined and independent roles of WCC and CRP. Significantly, this study demonstrates that these inflammatory biomarkers are associated with poor outcomes independent of the effects of stroke-associated pneumonia, a key confounder unadjusted for in previous analyses [7, 8, 24,25,26].
This study is subject to a number of limitations. ICH volume and Graeb Score are not recorded in the register, and thus were not adjusted for in this analysis. Hematoma volume is a strong predictor of outcome in ICH and is likely associated with elevation of inflammatory biomarkers. We were, however, able to adjust for NIHSS and OCSP, providing an index of ICH severity. While there was a large proportion of missing data for NIHSS, we utilized MICE to impute missing values in order to reduce bias secondary to data missingness. Furthermore, it has been previously shown that this remains statistically robust even with a high proportion of data missingness when the data are likely missing-at-random, as was the case in our study [27]. Previous work has found that NIHSS score is correlated with ICH volume, suggesting that adjusting for NIHSS may account for much of the confounding effects of ICH volume [28]. While the OCSP classification is not a marker of stroke severity per se, there is a strong association between stroke severity and OCSP, with total anterior circulation stroke syndromes being likely more severe than partial anterior circulation stroke syndromes which are likely more severe than lacunar stroke syndromes. Having much lower proportion of missing OCSP than NIHSS data, we included this as an adjustment in all our analyses to reduce residual confounding from stroke severity. While we adjusted for the effect of stroke-associated pneumonia in multivariate regressions, we were not able to adjust for other infections such as urinary tract infections, and patients with pre-existing infections could not be excluded. Other infections may, in part, account for the worse outcomes experienced by patients with elevated inflammatory biomarkers in this cohort, and further work adjusting for a wider range of infections would be insightful. However, the large proportion of patients with elevated inflammatory biomarkers, and a meta-analysis of 137,817 patients reporting that post-stroke urinary tract infections are not associated with mortality [29], suggest that other infections would only partially account for these worse outcomes. As time from stroke onset to admission is not recorded in the register, we were unable to adjust for this in our analyses, and the interval between admission and biomarker measurement varied. We nevertheless performed a sensitivity analysis including only those patients whose biomarkers were measured within 48 h of admission in order to ascertain whether the temporal relationship between hospital admission and biomarker measurement may influence these associations. The results of this sensitivity analysis were not meaningfully different from the primary analyses, suggesting that, in this study, the exact timing of inflammatory marker quantification may not influence the association between inflammation and adverse ICH outcomes as long as they are measured during the acute phase. Nevertheless, it is important to highlight that most of our included cohort had undergone blood parameter measurement within 48 h of admission and therefore our sensitivity analyses may be underpowered to determine such temporal associations accurately. Further research into the role of inflammatory biomarkers across both the acute and post-acute periods is warranted.
The results of this study have several potential implications. In patients with ICH, inflammatory biomarkers at admission were associated with poor outcomes: this suggests that they may be useful for prognostication in the context of ICH. These biomarkers have been previously used for prognostication in a variety of other contexts, including ischemic stroke, myocardial infarction, and intensive care unit mortality [30,31,32,33,34]. Incorporating these inflammatory biomarkers into existing severity scores may further improve their ability to stratify ICH severity. Additionally, the findings of this study emphasize the importance of conducting a prospective cohort study investigating inflammatory biomarkers in ICH to investigate these hypotheses further. This study also underscores the importance of inflammation in the context of ICH, and as a potential target for the development of novel treatments. Such future treatments may require an index of inflammation for determining patient eligibility, for which WCC and CRP may be promising candidates.
Conclusions
Co-elevation of WCC and CRP at admission was associated with an increased risk of poor functional outcome and death following ICH. These results underscore the importance of inflammation in ICH and suggest that these biomarkers may be valuable for prognostication in the context of ICH.
Abbreviations
- CI:
-
Confidence interval
- COPD:
-
Chronic obstructive pulmonary disorder
- CRP:
-
C-reactive protein
- HR:
-
Hazard ratio
- ICH:
-
Intracerebral hemorrhage
- LACS:
-
Lacunar stroke syndrome
- MICE:
-
Multiple imputation by chained equation
- mRS:
-
Modified Rankin Scale
- NIHSS:
-
National Institute of Health Stroke Scale
- OCSP:
-
Oxford Community Stroke Project
- OR:
-
Odds ratio
- PACS:
-
Partial anterior circulation stroke syndrome
- POCS:
-
Posterior circulation stroke syndrome
- RCS:
-
Restricted cubic spline
- RR:
-
Risk ratio
- SAH:
-
Subarachnoid hemorrhage
- SAP:
-
Stroke-associated pneumonia
- SD:
-
Standard deviation
- SIRS:
-
Systemic inflammatory response syndrome
- TACS:
-
Total anterior circulation stroke syndrome
- UTI:
-
Urinary tract infection
- WCC:
-
White cell count
References
Hemphill JC, Greenberg SM, Anderson CS, Becker K, Bendok BR, Cushman M et al (2015) Guidelines for the management of spontaneous intracerebral hemorrhage. Stroke 46:2032–2060. https://doi.org/10.1161/STR.0000000000000069
van Asch CJ, Luitse MJ, Rinkel GJ, van der Tweel I, Algra A, Klijn CJ (2010) Incidence, case fatality, and functional outcome of intracerebral haemorrhage over time, according to age, sex, and ethnic origin: a systematic review and meta-analysis. Lancet Neurol 9:167–176. https://doi.org/10.1016/S1474-4422(09)70340-0
Fu Y, Liu Q, Anrather J, Shi F-D (2015) Immune interventions in stroke. Nat Rev Neurol 11:524–535. https://doi.org/10.1038/nrneurol.2015.144
Gelderblom M, Leypoldt F, Steinbach K, Behrens D, Choe C-U, Siler DA et al (2009) Temporal and spatial dynamics of cerebral immune cell accumulation in stroke. Stroke 40:1849–1857. https://doi.org/10.1161/STROKEAHA.108.534503
Dziedzic T, Bartus S, Klimkowicz A, Motyl M, Slowik A, Szczudlik A (2002) Intracerebral hemorrhage triggers interleukin-6 and interleukin-10 release in blood. Stroke 33:2334–2335. https://doi.org/10.1161/01.STR.0000027211.73567.FA
Castillo J, Davalos A, Alvarez-Sabin J, Pumar JM, Leira R, Silva Y et al (2002) Molecular signatures of brain injury after intracerebral hemorrhage. Neurology 58:624–629. https://doi.org/10.1212/WNL.58.4.624
Mackey J, Blatsioris AD, Saha C, Moser EAS, Carter RJL, Cohen-Gadol AA et al (2020) Higher monocyte count is associated with 30-day case fatality in intracerebral hemorrhage. Neurocrit Care. https://doi.org/10.1007/s12028-020-01040-z
Walsh KB, Sekar P, Langefeld CD, Moomaw CJ, Elkind MSV, Boehme AK et al (2015) Monocyte count and 30-day case fatality in intracerebral hemorrhage. Stroke 46:2302–2304. https://doi.org/10.1161/STROKEAHA.115.009880
Bettencourt-Silva J, De La Iglesia B, Donell S, Rayward-Smith V (2012) On creating a patient-centric database from multiple hospital information systems. Methods Inf Med 51:210–220. https://doi.org/10.3414/ME10-01-0069
Smith CJ, Kishore AK, Vail A, Chamorro A, Garau J, Hopkins SJ et al (2015) Diagnosis of stroke-associated pneumonia. Stroke 46:2335–2340. https://doi.org/10.1161/STROKEAHA.115.009617
Macartney A (2020) Haematology NNUH user manual 2020
Del Rosario M (2020) NNUH clinical biochemistry user manual 2020
White IR, Royston P, Wood AM (2011) Multiple imputation using chained equations: issues and guidance for practice. Stat Med 30:377–399. https://doi.org/10.1002/sim.4067
Holmberg MJ, Andersen LW (2020) Estimating risk ratios and risk differences: alternatives to odds ratios. JAMA 324:1098–1099. https://doi.org/10.1001/jama.2020.12698
Cummings P (2009) Methods for estimating adjusted risk ratios. Stata J 9:175–196. https://doi.org/10.1177/1536867X0900900201
Lambert P (2015) RCSGEN: stata module to generate restricted cubic splines and their derivatives. Boston College Department of Economics
Wang J, Doré S (2007) Inflammation after intracerebral hemorrhage. J Cereb Blood Flow Metab 27:894–908. https://doi.org/10.1038/sj.jcbfm.9600403
Bigio MRD, Yan H-J, Buist R, Peeling J (1996) Experimental intracerebral hemorrhage in rats. Stroke 27:2312–2320. https://doi.org/10.1161/01.STR.27.12.2312
Gong C, Hoff JT, Keep RF (2000) Acute inflammatory reaction following experimental intracerebral hemorrhage in rat. Brain Res 871:57–65. https://doi.org/10.1016/S0006-8993(00)02427-6
Del Giudice M, Gangestad SW (2018) Rethinking IL-6 and CRP: why they are more than inflammatory biomarkers, and why it matters. Brain Behav Immun 70:61–75. https://doi.org/10.1016/j.bbi.2018.02.013
Silva Y, Leira R, Tejada J, Lainez JM, Castillo J, Dávalos A et al (2005) Molecular signatures of vascular injury are associated with early growth of intracerebral hemorrhage. Stroke 36:86–91. https://doi.org/10.1161/01.STR.0000149615.51204.0b
Suzuki S, Kelley RE, Dandapani BK, Reyes-Iglesias Y, Dietrich WD, Duncan RC (1995) Acute leukocyte and temperature response in hypertensive intracerebral hemorrhage. Stroke 26:1020–1023. https://doi.org/10.1161/01.STR.26.6.1020
Bestué-Cardiel M, Martín-Martínez J, Iturriaga-Heras C, Ara-Callizo JR, Oliveros-Juste A (1999) Leukocytes and primary intracerebral hemorrhage. Rev Neurol 29:968–971
Di Napoli M, Godoy DA, Campi V, del Valle M, Piñero G, Mirofsky M et al (2011) C-reactive protein level measurement improves mortality prediction when added to the spontaneous intracerebral hemorrhage score. Stroke 42:1230–1236. https://doi.org/10.1161/STROKEAHA.110.604983
Napoli MD, Godoy DA, Campi V, Masotti L, Smith CJ, Jones ARP et al (2012) C-reactive protein in intracerebral hemorrhage: time course, tissue localization, and prognosis. Neurology 79:690–699. https://doi.org/10.1212/WNL.0b013e318264e3be
Diedler J, Sykora M, Hahn P, Rupp A, Rocco A, Herweh C et al (2009) C-reactive-protein levels associated with infection predict short- and long-term outcome after supratentorial intracerebral hemorrhage. Cerebrovasc Dis 27:272–279. https://doi.org/10.1159/000199465
Madley-Dowd P, Hughes R, Tilling K, Heron J (2019) The proportion of missing data should not be used to guide decisions on multiple imputation. J Clin Epidemiol 110:63–73. https://doi.org/10.1016/j.jclinepi.2019.02.016
Nag C, Das K, Ghosh M, Khandakar MR (2012) Prediction of clinical outcome in acute hemorrhagic stroke from a single CT scan on admission. N A J Med Sci 4:463–467. https://doi.org/10.4103/1947-2714.101986
Westendorp WF, Nederkoorn PJ, Vermeij J-D, Dijkgraaf MG, de van Beek D (2011) Post-stroke infection: a systematic review and meta-analysis. BMC Neurol 11:110. https://doi.org/10.1186/1471-2377-11-110
Furlan JC, Vergouwen MDI, Fang J, Silver FL (2014) White blood cell count is an independent predictor of outcomes after acute ischaemic stroke. Eur J Neurol 21:215–222. https://doi.org/10.1111/ene.12233
Kaur M (2017) C-reactive protein: a prognostic indicator. Int J Appl Basic Med Res 7:83–84. https://doi.org/10.4103/ijabmr.IJABMR_63_17
Yoshinaga R, Doi Y, Ayukawa K, Ishikawa S (2017) High-sensitivity C reactive protein as a predictor of inhospital mortality in patients with cardiovascular disease at an emergency department: a retrospective cohort study. BMJ Open 7:e015112. https://doi.org/10.1136/bmjopen-2016-015112
Grzybowski M, Welch RD, Parsons L, Ndumele CE, Chen E, Zalenski R et al (2004) The association between white blood cell count and acute myocardial infarction in-hospital mortality: findings from the national registry of myocardial infarction. Acad Emerg Med 11:1049–1060. https://doi.org/10.1197/j.aem.2004.06.005
Larvin M, Mcmahon MJ (1989) APACHE-II score for assessment and monitoring of acute pancreatitis. Lancet 334:201–205. https://doi.org/10.1016/S0140-6736(89)90381-4
Acknowledgements
The authors gratefully acknowledge the Stroke Data Team at the Norfolk and Norwich University Hospital for data collection and maintenance of the NNUH database.
Funding
No funding was provided for the completion of this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no competing interests associated with this work.
Ethical approval
The Newcastle and Tyneside National Health Service and Research Ethics Committee provided ethical approval for this database, providing approval for anonymized research studies. This study was conducted in accordance with the principles of the Declaration of Helsinki (1964) and its later amendments.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bader, E.R., Pana, T.A., Barlas, R.S. et al. Elevated inflammatory biomarkers and poor outcomes in intracerebral hemorrhage. J Neurol 269, 6330–6341 (2022). https://doi.org/10.1007/s00415-022-11284-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-022-11284-8