Abstract
Background
A quarter of people with Intellectual Disability (ID) in the UK have epilepsy compared to 0.6% in the general population and die much younger. Epilepsy is associated with two-fifths of all deaths with related polypharmacy and multi-morbidity. Epilepsy research on this population has been poor. This study describes real-world clinical and risk characteristics of a large cohort across England and Wales.
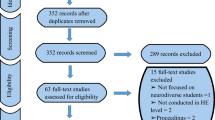
Methods
A retrospective multi-centre cohort study was conducted. Information on seizure characteristics, ID severity, relevant co-morbidities, psychotropic and antiseizure drugs (ASDs), SUDEP and other risk factors was collected across a year.
Results
Of 904 adults across 10 centres (male:female, 1.5:1), 320 (35%) had mild ID and 584 (65%) moderate-profound (M/P) ID. The mean age was 39.9 years (SD 15.0). Seizures were more frequent in M/P ID (p < 0.001). Over 50% had physical health co-morbidities, more in mild ID (p < 0.01). A third had psychiatric co-morbidity and a fifth had an underlying genetic disorder. Autism Spectrum Disorder was seen in over a third (37%). Participants were on median two ASDs and overall, five medications. Over quarter were on anti-psychotics. Over 90% had an epilepsy review in the past year but 25% did not have an epilepsy care plan, particularly those with mild ID (p < 0.001). Only 61% had a documented discussion of SUDEP, again less likely with mild ID or their care stakeholders (p < 0.001).
Conclusions
Significant levels of multi-morbidity, polypharmacy and a lack of systemised approach to treatment and risk exist. Addressing these concerns is essential to reduce premature mortality.
Similar content being viewed by others
Data statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Change history
05 March 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00415-022-11012-2
References
World Health Organisation (2004) ICD-10: international statistical classification of diseases and related health problems, 2nd edn. WHO, Geneva
Robertson J, Hatton C, Emerson E, Baines S (2015) Prevalence of epilepsy among people with intellectual disabilities: a systematic review. Seizure 29:46–62. https://doi.org/10.1016/j.seizure.2015.03.016
Fiest KM, Sauro KM, Wiebe S et al (2017) Prevalence and incidence of epilepsy: a systematic review and meta-analysis of international studies. Neurology 88(3):296–303. https://doi.org/10.1212/WNL.0000000000003509
Kinnear D, Morrison J, Allan L, Henderson A, Smiley E, Cooper S-A (2018) Prevalence of physical conditions and multimorbidity in a cohort of adults with intellectual disabilities with and without Down syndrome: cross-sectional study. BMJ Open 8(2):e018292. https://doi.org/10.1136/bmjopen-2017-018292
Devinsky O, Nashef L (2015) SUDEP. Neurology 85(18):1534. https://doi.org/10.1212/WNL.0000000000001948
The Learning Disability Mortality Review (LeDeR) Programme (2021) Annual Report 2020. University of Bristol Norah Fry Centre for Disability Studies. http://www.bristol.ac.uk/medialibrary/sites/sps/leder/LeDeR%20programme%20annual%20report%2013.05.2021%20FINAL.pdf. Accessed 18 Sept 2021
Young C, Shankar R, Palmer J et al (2015) Does intellectual disability increase sudden unexpected death in epilepsy (SUDEP) risk? Seizure 25:112–116. https://doi.org/10.1016/j.seizure.2014.10.001
McGrother CW, Bhaumik S, Thorp CF, Hauck A, Branford D, Watson JM (2006) Epilepsy in adults with intellectual disabilities: prevalence, associations and service implications. Seizure 15(6):376–386. https://doi.org/10.1016/j.seizure.2006.04.002
Glover G (2013) Hospital admissions that should not happen: admissions for ambulatory care sensitive conditions for people with learning disability in England. https://www.ndti.org.uk/assets/files/IHAL-2013-02_Hospital_admissions_that_should_not_happen_ii.pdf. Accessed 20 Sept 2021
Balogh R, Brownell M, Ouellette-Kuntz H, Colantonio A (2010) Hospitalisation rates for ambulatory care sensitive conditions for persons with and without an intellectual disability–a population perspective. J Intellect Disabil Res 54(9):820–832. https://doi.org/10.1111/j.1365-2788.2010.01311.x
Watkins L, O’Dwyer M, Kerr M, Scheepers M, Courtenay K, Shankar R (2020) Quality improvement in the management of people with epilepsy and intellectual disability: the development of clinical guidance. Expert Opin Pharmacother 21(2):173–181. https://doi.org/10.1080/14656566.2019.1695780
Shankar R, Scheepers M, Liew A et al (2020) Step together integrating care for people with epilepsy and a learning disability. https://www.bild.org.uk/wp-content/uploads/2020/11/Step-Together-17-November-2020-Download-Link-.pdf. Accessed 20 Sept 2021
Lines G, Henley W, Winterhalder R, Shankar R (2018) Awareness, attitudes, skills and training needs of psychiatrists working with adults with intellectual disability in managing epilepsy. Seizure 63:105–112. https://doi.org/10.1016/j.seizure.2018.11.001
Snoeijen-Schouwenaars F, Young C, Rowe C, van Ool J, Schelhaas H, Shankar R (2021) People with epilepsy and intellectual disability: more than a sum of two conditions. Epilepsy Behav. https://doi.org/10.1016/j.yebeh.2021.108355
Sun JJ, Perera B, Henley W, Ashby S, Shankar R (2020) Seizure and Sudden Unexpected Death in Epilepsy (SUDEP) characteristics in an urban UK intellectual disability service. Seizure 80:18–23. https://doi.org/10.1016/j.seizure.2020.05.004
Kinney MO, Chester V, Tromans S et al (2020) Epilepsy, anti-seizure medication, intellectual disability and challenging behavior: everyone’s business, no one’s priority. Seizure 81:111–116. https://doi.org/10.1016/j.seizure.2020.07.018
Allard J, Henley W, Snoeijen-Schouwenaars F et al (2020) European perspective of perampanel response in people with intellectual disability. Acta Neurol Scand 142(3):255–259. https://doi.org/10.1111/ane.13261
Shankar R, Rowe C, Van Hoorn A et al (2018) Under representation of people with epilepsy and intellectual disability in research. PLoS ONE 13(6):e0198261. https://doi.org/10.1371/journal.pone.0198261
Shankar R, Ashby S, McLean B, Newman C (2020) Bridging the gap of risk communication and management using the SUDEP and seizure safety checklist. Epilepsy Behav 103:106419. https://doi.org/10.1016/j.yebeh.2019.07.020
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42(2):377–381. https://doi.org/10.1016/j.jbi.2008.08.010
NHS Health Research Authority (2021) Is my study research? http://www.hra-decisiontools.org.uk/research/index.html. Accessed 29 Sept 2021
Trinka E, Cock H, Hesdorffer D et al (2015) A definition and classification of status epilepticus–report of the ILAE task force on classification of status epilepticus. Epilepsia 56(10):1515–1523. https://doi.org/10.1111/epi.13121
Royal College of Psychiatrists (2020) College Report 226 – Mental health services for adults with mild intellectual disability. https://www.rcpsych.ac.uk/improving-care/campaigning-for-better-mental-health-policy/college-reports/2020-college-reports/cr226. Accessed 29 Sept 2021
Chan AWK (1985) Alcoholism and epilepsy. Epilepsia 26(4):323–333. https://doi.org/10.1111/j.1528-1157.1985.tb05658.x
Shankar R, Donner EJ, McLean B, Nashef L, Tomson T (2017) Sudden unexpected death in epilepsy (SUDEP): what every neurologist should know. Epileptic Disord 19(1):1–9. https://doi.org/10.1684/epd.2017.0891
National Institute of Health and Care Excellence (NICE) (2012) Epilepsies: diagnosis and management. Clinical guideline [CG137]. https://www.nice.org.uk/guidance/cg137. Accessed 29 Sept 2021
Kerr MP, Watkins LV, Angus-Leppan H et al (2018) The provision of care to adults with an intellectual disability in the UK. A Special report from the intellectual disability UK chapter ILAE. Seizure 56:41–46. https://doi.org/10.1016/j.seizure.2018.01.026
Shankar R, Perera B, Thomas RH (2020) Epilepsy, an orphan disorder within the neurodevelopmental family. J Neurol Neurosurg Psychiatry 91(12):1245–1247. https://doi.org/10.1136/jnnp-2020-324660
King B, Toth K, Hodapp RM, Dykens E (2009) Intellectual disability. Compr Textb Psychiatry 01(01):3444–3474
Acknowledgements
Ms Gina Matthews for information governance support. Dr Adaobi Ikwueze for assisting data collection.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors satisfy the ICMJE guidance by substantially contributing to the design, analysis and interpretation of the work, drafting of the manuscript, final approval of the manuscript and all agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work is appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflicts of interest
Rohit Shankar has received institutional and research support from LivaNova, UCB, Eisai, Veriton Pharma, Bial, Averelle, UnEEG and GW pharma outside the submitted work. He holds grants from NIHR AI, SBRI and other funding bodies all outside this work. No other author has any declared conflict of interest related to this paper.
Ethics statement
We confirm that we have read the journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix 1: Rationale for examining mild and moderate-profound ID as two groups [14, 29]:
Appendix 1: Rationale for examining mild and moderate-profound ID as two groups [14, 29]:
-
1.
Each of the 3 sub-groups of moderate, severe, and profound ID have a low prevalence (9% moderate, 4% severe, and approximately 2% profound) and together they would combine to form 15% of the total ID population. Taken individually it would be difficult to achieve satisfactory power to deliver meaningful conclusions.
-
2.
Moderate, severe, and profound ID are difficult to assess and classify which causes significant issues with accuracy of specific diagnosis of moderate, severe, or profound ID.
-
3.
The groups of moderate, severe, and profound ID are defined by qualitatively significantly higher levels impairments. Where people with mild intellectual disability have near independent lives with some or minimal support, those with moderate/severe/profound ID tend to be supported and supervised at all times.
-
4.
Impairments such as communication difficulties, making informed choices and needing supervision is similar in the group of people with moderate, severe, and profound intellectual disability, People with mild intellectual disability can make informed choices on most day-to-day matters and can be supported to provide a personal view on medication choice, compliance, and reporting side effects.
-
5.
Epilepsy possibly due to disturbed brain function is present in 30—50% of the moderate to Profound ID group as compared to 8–12% in the mild ID population and 0.6−1% in general population.
Rights and permissions
About this article
Cite this article
Sun, J.J., Perera, B., Henley, W. et al. Epilepsy related multimorbidity, polypharmacy and risks in adults with intellectual disabilities: a national study. J Neurol 269, 2750–2760 (2022). https://doi.org/10.1007/s00415-021-10938-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-021-10938-3