Abstract
Objective
To determine frequencies, interlaboratory reproducibility, clinical ratings, and prognostic implications of neural antibodies in a routine laboratory setting in patients with suspected neuropsychiatric autoimmune conditions.
Methods
Earliest available samples from 10,919 patients were tested for a broad panel of neural antibodies. Sera that reacted with leucine-rich glioma-inactivated protein 1 (LGI1), contactin-associated protein-2 (CASPR2), or the voltage-gated potassium channel (VGKC) complex were retested for LGI1 and CASPR2 antibodies by another laboratory. Physicians in charge of patients with positive antibody results retrospectively reported on clinical, treatment, and outcome parameters.
Results
Positive results were obtained for 576 patients (5.3%). Median disease duration was 6 months (interquartile range 0.6–46 months). In most patients, antibodies were detected both in CSF and serum. However, in 16 (28%) patients with N-methyl-d-aspartate receptor (NMDAR) antibodies, this diagnosis could be made only in cerebrospinal fluid (CSF). The two laboratories agreed largely on LGI1 and CASPR2 antibody diagnoses (κ = 0.95). The clinicians (413 responses, 71.7%) rated two-thirds of the antibody-positive patients as autoimmune. Antibodies against the α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor (AMPAR), NMDAR (CSF or high serum titer), γ-aminobutyric acid-B receptor (GABABR), and LGI1 had ≥ 90% positive ratings, whereas antibodies against the glycine receptor, VGKC complex, or otherwise unspecified neuropil had ≤ 40% positive ratings. Of the patients with surface antibodies, 64% improved after ≥ 3 months, mostly with ≥ 1 immunotherapy intervention.
Conclusions
This novel approach starting from routine diagnostics in a dedicated laboratory provides reliable and useful results with therapeutic implications. Counseling should consider clinical presentation, demographic features, and antibody titers of the individual patient.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neural immunoglobulin G (IgG) autoantibodies help to define or refine the diagnosis of autoimmune diseases of the central and peripheral nervous system (CNS, PNS) [19, 20, 24, 35]. These antibodies provide an understanding of the pathogenesis of these conditions [10], suggest adequate therapies, and permit prognostic estimates [12]. Most of our knowledge comes from reports by research laboratories on patients with specific antibodies. Much autoantibody testing in the world is done by diagnostic laboratories that investigate material from poorly selected patients, must rely on what is sent in (serum, cerebral spinal fluid [CSF], or CSF–serum pairs), utilize ready-to-use assays, and are expected to provide test results within a short timeframe. The added value of data from such a laboratory that it is closely connected to its clinical senders may be a “real-world” impression of frequencies, clinical correlates, and therapeutic and prognostic implications of neural antibodies. These factors may also further clarify the relevance of N-methyl d-aspartate receptor (NMDAR) antibodies in serum only. Here, we retrospectively evaluated the 4-year experience of one such diagnostic laboratory to address these issues.
Methods
Antibody testing
Sera, CSF samples, or CSF–serum pairs (latency CSF–serum collections: ≤ 7 days) received by the antibody laboratory in Bethel between 12/2011 and 12/2015 were analyzed. They had been transferred by clinicians for suspected neuropsychiatric autoimmune conditions or for confirmation of external antibody findings. Only the first material of a given patient sent to this laboratory was included. Some patients have been reported before [5,6,7, 14,15,16, 39].
Antibodies against surface antigens or glutamic acid decarboxylase 65 kDa (GAD65)
Antibodies were detected using commercially available biochips (Euroimmun, Lübeck, Germany). These cell-based assays (CBA) consist of human embryonic kidney (HEK-293) cells transfected with plasmids that encode the following antigens. Cells that express NMDAR with NR1 subunits only and GAD65 were fixed with acetone; cells that express leucine-rich glioma-inactivated protein 1 (LGI1), contactin-associated protein-2 (CASPR2), α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor subunits 1 and 2 (AMPAR1 and AMPAR2), γ-aminobutyric acid-B receptors (GABABR), or glycine receptor (GlyR) were fixed with paraformaldehyde. Their preparation follows an established principle [11] and has been described [46]. The protocol for indirect immunofluorescence followed the manufacturer’s recommendations (Euroimmun, FA 112d-1005-1, IgG) with these modifications (CGB, detailed in [4]): serum diluted 1:16; buffer was phosphate-buffered saline (PBS); secondary antibody was goat-anti-human IgG heavy and light chain (H + L) conjugated with Alexa Fluor 594 (Jackson ImmunoResearch, West Grove, PA, USA, No. 109-585-088), used at a dilution of 1:100 and incubated for 30 min at room temperature (RT); nuclear counterstaining with Hoechst 33,342, 1:10,000; embedding with 1,4-Diazabicyclo[2.2.2]octan. Stained biochips were examined using a fluorescence microscope (Leica DM 2000, Wetzlar, Germany) equipped with adequate filters. One of three neurologists experienced in the reading of this assay (CGB, CIB, or MDO) decided whether an antibody was present using the signal of the surrounding (supposedly negative) fields as respective negative controls. IgG positivity was confirmed by goat-anti-human antibody against the Fcγ fragment of IgG (conjugated with Alexa Fluor 488; Jackson Immunoresearch, No. 304-585-008) diluted 1:100 and incubated for 30 min at RT. Positive samples were endpoint titrated with the Fc antibody. These titrations were 1:16, 1:32, 1:64, and so on for serum and 1:1 (undiluted), 1:2, 1:4 and so on for CSF. Two of four investigators (CGB, CIB, MDO, or an experienced technician) determined the dilution that provided the last specific signal. This was noted as the titer. In cases of divergent ratings, the mean of the two ratings was recorded. We determined IgG subclasses as described before [6].
All samples were also tested on unfixed sagittal mouse brain slices that contained hippocampus, brain stem, and cerebellum (Euroimmun, Lübeck, Germany). These tissue-based assays (TBAs) were incubated with serum diluted 1:40 or undiluted CSF. More intense binding to the neuropil compared to cell bodies in hippocampus or cerebellum was noted as “neuropil staining”. Such reactivity was not required to make the diagnosis of a specified surface antibody; specific binding to transfected cells was sufficient.
Categorization and analyses
Patients were categorized by their antibody results (Table 1). Data on NMDAR-high, LGI1, CASPR2, and GAD65 patients are preferentially described. We considered them as “major antibody groups”, given their frequency in the literature [12] and in this study. For rarer antibodies, see the Supplementary material.
Interlaboratory reproducibility
All available sera with antibodies against LGI1, CASPR2, or the VGKC complex (as indicator of potential LGI1 or CASPR2 reactivity) plus 75 neighboring samples that did not harbor any of these antibodies (negative controls) were tested for LGI1 or CASPR2 antibodies by RH, who only knew that the samples were positive for at least one of the respective antibodies. In the first step, sera were screened with an in-house TBA. For this process, fresh adult rat brains were fixed in 4% paraformaldehyde for 1 h at 4 °C, cryoprotected with 40% sucrose for 48 h, embedded in freezing medium, and snap frozen in isopentane chilled with liquid nitrogen. Sagittal cryostat sections (7 μm) were defrosted for 15–30 min, washed in PBS, incubated for 15 min in 0.3% H2O2, and blocked for 60 min with 5% donkey serum in PBS. After incubation with patient’s serum (dilution: 1:200) at 4 °C overnight and labeling with secondary antibody (biotinylated donkey anti-human, 1:2000, 1 h, RT), slices were incubated with avidin–biotin for 1 h, visualized with 3.3-diaminobenzidin-tetrachlorid (DAB) for 7 min, and covered with coverslips. Samples with positive neuropil staining in the hippocampus and molecular layer of the cerebellum were further tested on a commercially available biochip (Euroimmun), according to the manufacturer´s instructions. A positive result in both TBA and CBA was required for the diagnosis of a surface antibody.
Delivery notes
The following pieces of information from the delivery notes were documented: demographic data, tentative diagnoses (free text), and date of disease onset. From 12/2014 to 12/2015, senders were also asked to categorize the patients according to this list: encephalitis, epilepsy, cognitive/psychiatric problem, other disorder; multiple selections were possible.
Questionnaires
The institutions who received positive antibody results were asked to complete a questionnaire with the following questions: date of questionnaire completion, previous viral encephalitis, antibody diagnosis known when material sent to this laboratory, date of disease onset, final diagnosis (free text), final judgement (CNS or PNS autoimmune disease), tumor, modified Rankin Scale (mRS) at antibody diagnosis and most recent follow-up, date of most recent follow-up. As follow-up, only visits ≥ 3 months from antibody diagnosis were accepted.
Clinical syndromes
Clinical syndromes were defined post hoc by CGB based on free text notes on the questionnaires and the delivery forms.
Ethics statement
The study was approved by the Ethics committee of the University of Münster, Germany (2017-005-f-S).
Statistics
Kappa coefficient and Mann–Whitney U test were used as indicated. Statistical analyses were performed with IBM SPSS (Version 25).
Data availability
Any data not published within this article are available at the Epilepsy Center Bethel. Data will be shared upon request from any qualified investigator, maintaining anonymization of the patients.
Results
Antibody-positive patients
Of the total 10,919 patients, 5592 were investigated in CSF–serum pairs (51.2%), 4803 for serum only (44.0%), and 524 for CSF only (4.8%). Mean age was 47.3 years (standard deviation [SD] 22.5, range 0.1–95 years; < 18 years: N = 1424 [13.0%]; females/males/sex unknown: 5696/5205/18, i.e., 52.3%/47.7%/0.2%); > 90% of results were returned within one week. For 3434 patients, 3481 clinical categorizations were noted: encephalitis (38.1%); epilepsy (18.6%); cognitive/psychiatric problem (1.0%); other (31.9%); no information (11.7%); multiple answers were possible. VGKC complex antibodies were assessed in 9239 cases (84.6%).
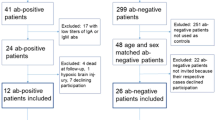
Neural antibodies were diagnosed in 576 patients (5.3%; Table 1). In 59 patients (10.2%), these results confirmed previous external antibody findings. The female/male/sex unknown percentages among the antibody-positive cases were 54.8%/45.0%/0.2%. For age and sex distributions, see Fig. 1.
Age, sex, and prevalence. Distribution of age (in 5-year-intervals) and sex (red = female, blue = male) in the four major groups and the negatives. In the diagrams to the right, the bars indicate antibody prevalences, i.e., the proportions of positives related to all investigated patients (divided into subgroups defined by age and sex)
In the patients with this piece of information available (N = 417), materials were sent after a median disease duration of 6 months (interquartile range [IQR] 0.6–46, mean 46, SD 92 months, maximum 63 years); for the single antibody groups, see Fig. 2a. The NMDAR-high group stood out, because in 16 (28%) cases, antibodies were detected in CSF only. In contrast, LGI1 and CASPR2 patients were identified by serum-only positivity in 33% and 48% of cases, respectively (Fig. 2b). The proportions of the subclasses for the four major groups (N = 279) are shown in Fig. 2c.
Disease durations, CSF/serum/CSF–serum pairs, IgG subclasses, and clinical ratings. a Latency (in months) between disease manifestation and antibody diagnostics in the antibody-positive cases with known disease onset. The lines indicate medians with quartiles. Antibody groups are given in ascending order of their median latencies. A1: linear x-axis, A2: logarithmic x-axis (note that “1” was added to all values to be able to include values of zero). b Ratio of cases with serum-only or CSF-only antibody positivity in the four major antibody groups plus onconeural and GABABR antibodies. The small groups with serum-only and CSF-only findings in the GAD65 group are cases with either very low CSF titers (N = 3) and negative serum or serum titers of just 1:500 and negative CSF samples (N = 2). In the onconeural group, there was one Ma2 case that was not fully appreciated in serum (blot positivity only) but clearly diagnosed in CSF (blot and tissue-based assay positive). c IgG subclasses in the four major antibody groups. d Clinical retrospective ratings (“Autoimmune disease of the CNS or PNS?”) in descending order of the positive ratings
Interlaboratory reproducibility of antibody test results
There was an agreement of 97.3% (223/229) with κ = 0.952 (p < 0.001; Table 2).
Clinical ratings
Of 173 contacted institutions, 115 (66.5%) filled in the questionnaires for 413/576 patients (71.7%). The “yes/not sure/no” rating percentages for retrospectively assuming a CNS or PNS autoimmune disease were 58.4%/5.8%/35.3%. The proportions provided a grading of the antibody groups (Fig. 2d and Table 1).
NMDAR high
Positive clinical ratings and clinical data consistent with autoimmune encephalitis were provided in 42/44 cases. Two were rated by treating physicians as negative: a 65-year old man with no previous encephalitis had a 13-month history of mediotemporal lobe seizures of unexplained origin and mild verbal memory impairment. Serum titer was 1:2000. CSF contained 153 cells/µl and NMDAR antibodies at 1:12. No alternative cause was established but neither the syndrome nor sex or age of the patients fit to classical anti-NMDAR encephalitis. The patient was lost to follow-up. A 15-year old boy with multiple sclerosis (MS) harbored NMDAR antibodies in CSF at 1:12 (serum negative) < 1 month after the first disease signs; myelin oligodendrocyte glycoprotein (MOG) and aquaporin-4 (AQP4) antibodies were negative. He developed relapsing–remitting MS but never anti-NMDAR encephalitis.
NMDAR in serum but not in CSF
Seven patients were serum-only-positive in the CBA; TBA was negative with serum and with CSF. They had etiologically unclear focal epilepsy (54 years, female), progressive myoclonus epilepsy (not further specified, 3 years, male), focal epilepsy after presumed limbic encephalitis (72 years, female, viral encephalitis in her history), anaplastic astrocytoma III° (4 years, male), frontotemporal dementia with parkinsonism (71 years, male), presumed limbic encephalitis, status epilepticus and bone metastases (suspected bronchial carcinoma, 72 years, male), and dementia with depression (48 years, female).
NMDAR in serum and no CSF tested
Thirteen patients had only serum studied as their first material. Eight underwent subsequent CSF studies. CSF was NMDAR antibody positive in six, five of which were classified as anti-NMDAR encephalitis (one had a positive serum-TBA), whereas one had structural post-herpes epilepsy [39]; two were CSF negative (focal epilepsy, 35 years, male; progressive supranuclear palsy, 72 years, male). The remaining five had no CSF study (cerebellar syndrome, 57 years, female; glioblastoma, 50 years, female; polymorphic subjective complaints and non-epileptic twitches, 41 years, male; dementia with depression, 48 years, female; focal epilepsy, 57 years, male). No patient in this subgroup without anti-NMDAR encephalitis had a positive serum-TBA.
LGI1
All 81 patients had serum antibody titers ≥ 1:64; the 56 patients with available clinical diagnoses had limbic encephalitis with or without faciobrachial dystonic seizures (FBDS).
Five cases received the diagnosis of focal epilepsy of an unknown cause (in one case, with hippocampal sclerosis) at epilepsy centers. Physicians rated them as “negative” or “uncertain”. Serum titers were 1:128-1:6000. Disease duration was longer than in the cases with a positive clinical rating (2.3, 4.2, 12.0, 12.0, and 302.5 months versus median 1.6, IQR 0–162 months; p = 0.04, Mann–Whitney U test). They did not receive immunotherapy. Three patients with a follow-up remained unchanged. Apparently, the cognitive decline and the imaging features were not impressive. Therefore, treating physicians did not make the autoimmune encephalitis diagnosis. Finally, one 78-year old woman had severe encephalomyeloradiculitis and albumino-cellular dissociation in CSF, as in Guillain-Barré syndrome. She also developed dementia. Five months after disease onset, she had a serum titer of 1:1000. Despite steroids, she remained at mRS 5 (due to the neuropathy, no information on cognitive outcome).
CASPR2
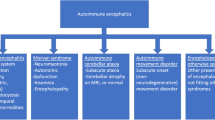
Thirty-four out of 44 CASPR2 cases (77%) with available clinical data had frequent and well-known clinical associations: limbic encephalitis (N = 26), Morvan syndrome (N = 3), neuromyotonia (N = 4) or cerebellar ataxia (N = 1). Clinical ratings were available in 25 patients, and they were all considered “positive”.
Three cases were rated “uncertain” but had high serum titers (1:32,000–1:6,000,000) and the clinical diagnoses of chorea (66 years, male), encephalitis with brain stem plus cerebellar lesions and histopathologic evidence of encephalitis (64 years, male), and lesions of the optic nerves with loss of vision in the presence of a thymoma (46 years, female).
The remaining patients had other conditions and were not rated as having an autoimmune disease (negative, N = 8; uncertain, N = 1). Serum titers were 1:128–1:500. Diagnoses were chronic-inflammatory demyelinating polyneuropathy (76 years, male), focal epilepsy with hippocampal sclerosis (48 years, female), dementia with amyloid angiopathy (male, 83 years), delusional disorder (60 years, male), paranoid-hallucinatory psychosis (54 years, female), Creutzfeldt-Jakob disease (75 years, male), chronic progressive external ophthalmoplegia (65 years, female), Parry–Romberg syndrome (30 years, male), and hemorrhagic encephalitis (74 years, female).
GAD65 antibodies
Clinical syndromes were available from 111/119 cases: focal epilepsy, N = 58 (49%); limbic encephalitis, N = 23 (19%); progressive encephalomyelitis with rigidity and myoclonus (PERM)/stiff-man syndrome (SMS)/stiff-limb syndrome, N = 8 (7%); cerebellar ataxia, N = 7 (6%); epilepsy not further specified, N = 5 (4%); single seizure, N = 1 (1%); other, N = 9 (7%; 2 patients had dementia, both 81 years; encephalopathy, 50 years; MS, 17 years; psychosis, 48 years; ocular myasthenia gravis with antibodies against the muscular acetylcholine receptor and titin plus sarcoidosis of lung and skin, 38 years; unclear coma, 47 years; developmental retardation with macrocephalia and periventricular leukomalacia, 1 year; depressive syndrome, 37 years, the only male patient within the syndromic category “other”). There was almost equipoise in clinical ratings of “yes” (N = 52) versus “no”/”uncertain” (N = 41). Even within the frequent syndromes (limbic encephalitis, focal epilepsy, PERM/SMS, and cerebellar ataxia), positive and non-positive ratings were equal. Disease durations did not differ between patients with “positive” and “negative”/”uncertain ratings”. The dominance of females (93/119, 78%) was found across all syndromic groups.
Other antibodies, tumors and previous viral encephalitis
See Supplementary material.
Immunotherapies and outcomes
A ≥ 3-month follow-up was available for 251 patients. These were rated after a mean of 32 months (SD 21, range 3–79 months) since antibody diagnosis and 23 months (SD 20, range 0–71 months) after last follow-up; 192 patients received at least one immunotherapy (Fig. 3a). Among all 244 patients with a ≥ 3-month follow-up and available outcome, 109 improved (44.7%). For patients with defined surface antibodies (AMPAR2, CASPR2, GABABR, GlyR, LGI1, or NMDAR-high), the ratio (72/102, 68.6%) was even better (Fig. 3b–f).
Immunotherapy and outcome in the four major antibody groups (NMDAR-high, LGI1, CASPR2, and GAD65). a Mean number of immunotherapies per patient with standard deviations. b Proportions and extent of changes according to the modified Rankin scale (mRS). Blue boxes indicate improvements, grey boxes stability, and reddish boxes deterioration. Labeling of the x-axis: after the N values, the median follow-up is given (mo = months). c–f Clinical performance (mRS) at antibody diagnostics (“pre”) and at most recent follow-up (“post”). Lower values indicate better performance. Left-most bars: all patients with rating at antibody diagnostics; second bars: patients with “post” ratings available at the time-point “pre” (there are no relevant differences between the total groups and those with an outcome); third bars: outcome; right-most bars: proportions of number of immunotherapies used. Please note that information on “no. of therapies” was only available for 34 LGI1 patients
Discussion
This large prospective series of > 10,000 patients was extensively and uniformly tested for neural antibodies in a routine laboratory with dedicated evaluators and a short turnover time. The general approach with an evaluation starting from the antibody findings in a routine diagnostic setting and not from patients with predefined features (this increases the likelihood of positive findings) [17, 22, 29] or selected antibodies [18, 26] is novel. Cases came from day-to-day practice and were considered clinically suspicious. However, selection criteria remained uncontrolled and were obviously not very stringent: only 5.3% of patients were antibody positive. The yield could be higher if patients were chosen in a more focused manner, e.g., according to Graus’ criteria of “possible autoimmune encephalitis” [20]. On the other hand, such an approach may miss cases with LGI1 antibodies and predominant focal seizures as reported above. CNS disorders prevailed (approximately two-thirds of samples). An overrepresentation of seizure disorders is possible; comparative figures from other laboratories are not available to our knowledge.
The four major antibody groups with defined targets were GAD65, LGI1, NMDAR-high, and CASPR2. Age, sex (Fig. 1), and IgG subclass distribution (Fig. 2c) were similar to previous publications [1, 23, 27, 41,42,43, 45]. Only half of the patients were tested within 6 months post-disease onset. The broad range of latencies suggests differential disease evolutions, fast for NMDAR, slow for GAD65 (Fig. 2a).
The Bethel VGKC complex, LGI1 and CASPR2 results had high interlaboratory reproducibility when verified in the Vienna laboratory. This suggests that the use of the Euroimmun assays in experienced hands provides reliable results, at least for these antibodies. Including VGKC complex antibody positives increased the a priori probability of finding LGI1 or CASPR2 antibody positives (more than just testing some of the many negatives). This gives the chance not only to replicate (or refute) positive findings but also to detect previously overlooked antibodies.
CSF was required for the diagnosis in 28% of NMDAR-high cases studied in serum–CSF pairs (Fig. 2b). This was previously reported (with 14% CSF-only NMDAR antibodies) [21].
Assessment of antibody validity is not easy, because there is no external gold standard. We did not exclude low-titer antibodies ante hoc (except in CASPR2 and GAD65 [6, 34]). Clinical ratings may be the best possible approximation. The retrospective judgement of the treating physicians (“autoimmune CNS or PNS disease”) provided the highest percentages of “positive” ratings for surface antibodies and onconeural antibodies (Fig. 2c). Groups with low percentages exhibited either equipoise in the interpretation (e.g., GAD65 antibodies: are they really indicative of an ongoing autoimmune process?), or physicians noted their conspicuous inhomogeneous nature (in VGKC complex, neuropil–CSF, and GlyR, specificity has been questioned in the literature [3, 40, 44]).
High-titer NMDAR antibodies (i.e., positive in CSF or a serum titer > 1:500) are very specific for anti-NMDAR encephalitis [21]. Patients ≤ 35 years and females are at a higher risk. In our series, 12% had ovarian teratomata. This is less than in North-American series. The probable reason is that patients of Afro-American and Asian descent are more frequent there. They more often have anti-NMDAR encephalitis with teratoma (> 40%) [42].
Serum-only reactivity with NMDAR-transfected cells (in the absence of neuropil staining in the TBA) at titers ≤ 1:500 is non-specific. This was previously inferred [20, 40], and it is formally demonstrated here. Only those patients who were subsequently found to have NMDAR antibodies in CSF, too, had typical anti-NMDAR encephalitis and responded to immunotherapy. Previous studies have at times considered low-titer serum-only findings as indicating specific autoimmune processes in patients with psychoses, other neurological and psychiatric diseases and potentially even healthy controls [8, 31]. Such interpretations have rightly been criticized for their lack of specificity [30]. This is supported by our findings.
LGI1 antibodies (all ≥ 1:64 in this study) were very specific: 50/56 patients had limbic encephalitis, in part with FBDS (89%). One elderly female had an autoimmune neuropathy but with dementia. Five patients with predominant recurrent focal seizures (in part for > 1 year) were seen at epilepsy centers and were neither diagnosed nor treated as autoimmune encephalitis. In contrast to most immunologically treated LGI1 patients, they did not improve. We speculate that these six patients had a forme fruste of limbic encephalitis; alternatively, they may have had a different disease, and the LGI1 antibodies may have been non-specific bystanders. People > 55 years had a higher likelihood of acquiring LGI1-antibody-associated diseases. Younger people, even in the pediatric age range, may occasionally be affected [37].
CASPR2 antibodies with a titer ≥ 1:128 are rather specific for limbic encephalitis, neuromyotonia, Morvan syndrome, or cerebellar ataxia. At times, CASPR2 antibodies occur with chorea, brainstem encephalitis plus cerebellitis, or less characteristic constellations like optic neuritis in the context of thymoma [18, 38]. CASPR2 antibodies are most often found in men > 55 years, as previously reported [23, 25, 28, 43]. Pediatric cases occur [37].
The majority of patients with GAD65 (> 80%) had focal epilepsy [32], limbic encephalitis [33], PERM/SMS [9], or cerebellar ataxia [2]. The almost equal positive versus negative/uncertain clinical rating ratios appear to be due to uncertainty how to interpret GAD65 antibodies. The preponderance of females suggests a genetic component. Antibody detection followed an inverted-U curve over the lifespan, with a peak at 40–45 years. This maximum was less marked than the peaks in the NMDAR-high, CASPR2, and LGI1 groups. The GAD65-CBA was recently found to produce reliable results in comparison to indirect immunohistochemistry or enzyme-linked immunosorbent assay [36].
Outcomes after ≥ 3 months were rated by the treating physicians (Fig. 3), an advantage over other studies, where it is not always clear who assessed the mRS. Among the four major groups, NMDAR-high and LGI1 patients had the largest proportions of improving cases and of mRS ≤ 2 (80% and 77%, respectively, and 70 and 83%; Fig. 2b). The rate of NMDAR-high patients with mRS ≤ 2 was similar to two large series (N = 252 after 2-year follow-up; N = 75 after a median follow-up of 27 months): 81% and 74%, respectively [13, 42]. In one study, the mRS ≤ 2 rate was 78% for LGI1 antibodies [13]. Of 28 CASPR2 patients, 57% improved after a median follow-up of 27 months. This is lower compared to two existing studies (94% of 16 patients after a median of 28 months [25] and 91% of 27 patients after a median of 36 months [43]). The reason for this difference is unknown. The 59 GAD65 patients had the poorest improvement rate of only 19%. To our knowledge, no figures for comparison are available from the literature.
Limitations are related to the study’s retrospective aspects. We did not get clinical information on all antibody-positive cases. The clinical assessment was not formalized. Our TBA was neither as sensitive as reported by in-house assays from other laboratories (many samples with clear-cut CBA results did not produce a neuropil staining) and it was also not very specific (the “neuropil staining” did not indicate many cases with autoimmune encephalitides). Control laboratory tests were only done for a subset of antibody-positive patients. Only a few negative materials were re-tested. We may have overlooked positive cases. The mRS may be insensitive to circumscribed cognitive problems, which makes the outcome of LGI1 patients look as good as NMDAR patients at follow-up; in fact, the LGI1 group has remaining memory problems that the NMDAR cases do not normally have.
In conclusion, test results for neural antibodies with commercially available assays in a dedicated routine laboratory are reliable (demonstrated for LGI1, CASPR2 and VGKC complex cases, if LGI1 or CASPR2 antibody positive or negative) and clinically meaningful. One should consider clinical presentation, demographic features, and titers when interpreting an antibody result in an individual patient. Patients positive for neural antibodies were in more than half of the cases retrospectively judged to have had an autoimmune condition. NMDAR-high, LGI1, GABABR, and AMPAR patients achieved positive ratings in ≥ 90% of cases. Of the patients with surface antibodies and follow-up, 64% improved. These data underscore the enormous therapeutic potential of this new branch of diagnostics.
Change history
25 June 2021
A Correction to this paper has been published: https://doi.org/10.1007/s00415-021-10634-2
12 May 2020
A Correction to this paper has been published: https://doi.org/10.1007/s00415-020-09855-8
References
Ariño H, Armangue T, Petit-Pedrol M, Sabater L, Martinez-Hernandez E, Hara M, Lancaster E, Saiz A, Dalmau J, Graus F (2016) Anti-LGI1-associated cognitive impairment: presentation and long-term outcome. Neurology 87:759–765
Ariño H, Gresa-Arribas N, Blanco Y, Martinez-Hernandez E, Sabater L, Petit-Pedrol M, Rouco I, Bataller L, Dalmau JO, Saiz A, Graus F (2014) Cerebellar ataxia and glutamic acid decarboxylase antibodies: immunologic profile and long-term effect of immunotherapy. JAMA Neurol 71:1009–1016
Armangue T, Sabater L, Torres-Vega E, Martinez-Hernandez E, Arino H, Petit-Pedrol M, Planaguma J, Bataller L, Dalmau J, Graus F (2016) Clinical and immunological features of opsoclonus-myoclonus syndrome in the era of neuronal cell surface antibodies. JAMA Neurol 73:417–424
Bien CG (2019) Diagnosing autoimmune encephalitis based on clinical features and autoantibody findings. Expert Rev Clin Immunol 15:511–527
Bien CG (2018) Overinterpretation and overtreatment of low-titer antibodies against contactin-associated protein-2. Front Immunol 9:703
Bien CG, Mirzadjanova Z, Baumgartner C, Onugoren MD, Grunwald T, Holtkamp M, Isenmann S, Kermer P, Melzer N, Naumann M, Riepe M, Schabitz WR, von Oertzen TJ, von Podewils F, Rauschka H, May TW (2017) Anti-contactin-associated protein-2 encephalitis: relevance of antibody titres, presentation and outcome. Eur J Neurol 24:175–186
Boesebeck F, Schwarz O, Dohmen B, Graef U, Vestring T, Kramme C, Bien CG (2013) Faciobrachial dystonic seizures arise from cortico-subcortical abnormal brain areas. J Neurol 260:1684–1686
Dahm L, Ott C, Steiner J, Stepniak B, Teegen B, Saschenbrecker S, Hammer C, Borowski K, Begemann M, Lemke S, Rentzsch K, Probst C, Martens H, Wienands J, Spalletta G, Weissenborn K, Stocker W, Ehrenreich H (2014) Seroprevalence of autoantibodies against brain antigens in health and disease. Ann Neurol 76:82–94
Dalakas MC, Li M, Fujii M, Jacobowitz DM (2001) Stiff person syndrome: quantification, specificity, and intrathecal synthesis of GAD65 antibodies. Neurology 57:780–784
Dalmau J, Geis C, Graus F (2017) Autoantibodies to synaptic receptors and neuronal cell surface proteins in autoimmune diseases of the central nervous system. Physiol Rev 97:839–887
Dalmau J, Gleichman AJ, Hughes EG, Rossi JE, Peng X, Lai M, Dessain SK, Rosenfeld MR, Balice-Gordon R, Lynch DR (2008) Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol 7:1091–1098
Dalmau J, Graus F (2018) Antibody-mediated encephalitis. N Engl J Med 378:840–851
de Bruijn MAAM, van Sonderen A, van Coevorden-Hameete MH, Bastiaansen AEM, Schreurs MWJ, Rouhl RPW, van Donselaar CA, Majoie M, Neuteboom RF, Sillevis Smitt PAE, Thijs RD, Titulaer MJ (2019) Evaluation of seizure treatment in anti-LGI1, anti-NMDAR, and anti-GABABR encephalitis. Neurology 92:e2185–e2196
Dogan Onugoren M, Deuretzbacher D, Haensch CA, Hagedorn HJ, Halve S, Isenmann S, Kramme C, Lohner H, Melzer N, Monotti R, Presslauer S, Schabitz WR, Steffanoni S, Stoeck K, Strittmatter M, Stogbauer F, Trinka E, von Oertzen TJ, Wiendl H, Woermann FG, Bien CG (2015) Limbic encephalitis due to GABAB and AMPA receptor antibodies: a case series. J Neurol Neurosurg Psychiatry 86:965–972
Dogan Onugoren M, Golombeck KS, Bien C, Abu-Tair M, Brand M, Bulla-Hellwig M, Lohmann H, Munstermann D, Pavenstadt H, Tholking G, Valentin R, Wiendl H, Melzer N, Bien CG (2016) Immunoadsorption therapy in autoimmune encephalitides. Neurol Neuroimmunol Neuroinflamm 3:e207
Dogan Onugoren M, Rauschka H, Bien CG (2014) Conjoint occurrence of GABAB receptor antibodies in Lambert-Eaton myasthenic syndrome with antibodies to the voltage gated calcium channel. J Neuroimmunol 273:115–116
Escudero D, Guasp M, Arino H, Gaig C, Martinez-Hernandez E, Dalmau J, Graus F (2017) Antibody-associated CNS syndromes without signs of inflammation in the elderly. Neurology 89:1471–1475
Gadoth A, Pittock SJ, Dubey D, McKeon A, Britton JW, Schmeling JE, Smith A, Kotsenas AL, Watson RE, Lachance DH, Flanagan EP, Lennon VA, Klein CJ (2017) Expanded phenotypes and outcomes among 256 LGI1/CASPR2-IgG-positive patients. Ann Neurol 82:79–92
Geis C, Planaguma J, Carreño M, Graus F, Dalmau J (2019) Autoimmune seizures and epilepsy. J Clin Invest 129:926–940
Graus F, Titulaer MJ, Balu R, Benseler S, Bien CG, Cellucci T, Cortese I, Dale RC, Gelfand JM, Geschwind M, Glaser CA, Honnorat J, Hoftberger R, Iizuka T, Irani SR, Lancaster E, Leypoldt F, Pruss H, Rae-Grant A, Reindl M, Rosenfeld MR, Rostasy K, Saiz A, Venkatesan A, Vincent A, Wandinger KP, Waters P, Dalmau J (2016) A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol 15:391–404
Gresa-Arribas N, Titulaer MJ, Torrents A, Aguilar E, McCracken L, Leypoldt F, Gleichman AJ, Balice-Gordon R, Rosenfeld MR, Lynch D, Graus F, Dalmau J (2014) Antibody titres at diagnosis and during follow-up of anti-NMDA receptor encephalitis: a retrospective study. Lancet Neurol 13:167–177
Hacohen Y, Wright S, Waters P, Agrawal S, Carr L, Cross H, De Sousa C, Devile C, Fallon P, Gupta R, Hedderly T, Hughes E, Kerr T, Lascelles K, Lin JP, Philip S, Pohl K, Prabahkar P, Smith M, Williams R, Clarke A, Hemingway C, Wassmer E, Vincent A, Lim MJ (2013) Paediatric autoimmune encephalopathies: clinical features, laboratory investigations and outcomes in patients with or without antibodies to known central nervous system autoantigens. J Neurol Neurosurg Psychiatry 84:748–755
Irani SR, Alexander S, Waters P, Kleopa KA, Pettingill P, Zuliani L, Peles E, Buckley C, Lang B, Vincent A (2010) Antibodies to Kv1 potassium channel-complex proteins leucine-rich, glioma inactivated 1 protein and contactin-associated protein-2 in limbic encephalitis, Morvan's syndrome and acquired neuromyotonia. Brain 133:2734–2748
Irani SR, Pettingill P, Kleopa KA, Schiza N, Waters P, Mazia C, Zuliani L, Watanabe O, Lang B, Buckley C, Vincent A (2012) Morvan syndrome: clinical and serological observations in 29 cases. Ann Neurol 72:241–255
Joubert B, Saint-Martin M, Noraz N, Picard G, Rogemond V, Ducray F, Desestret V, Psimaras D, Delattre JY, Antoine JC, Honnorat J (2016) Characterization of a subtype of autoimmune encephalitis with anti-contactin-associated protein-like 2 antibodies in the cerebrospinal fluid, prominent limbic symptoms, and seizures. JAMA Neurol 73:1115–1124
Kruse JL, Lapid MI, Lennon VA, Klein CJ, Toole OO, Pittock SJ, Strand EA, Frye MA, McKeon A (2015) Psychiatric autoimmunity: N-methyl-d-aspartate receptor igg and beyond. Psychosomatics 56:227–241
Lai M, Huijbers MG, Lancaster E, Graus F, Bataller L, Balice-Gordon R, Cowell JK, Dalmau J (2010) Investigation of LGI1 as the antigen in limbic encephalitis previously attributed to potassium channels: a case series. Lancet Neurol 9:776–785
Lancaster E, Huijbers MG, Bar V, Boronat A, Wong A, Martinez-Hernandez E, Wilson C, Jacobs D, Lai M, Walker RW, Graus F, Bataller L, Illa I, Markx S, Strauss KA, Peles E, Scherer SS, Dalmau J (2011) Investigations of Caspr2, an autoantigen of encephalitis and neuromyotonia. Ann Neurol 69:303–311
Lancaster E, Lai M, Peng X, Hughes E, Constantinescu R, Raizer J, Friedman D, Skeen MB, Grisold W, Kimura A, Ohta K, Iizuka T, Guzman M, Graus F, Moss SJ, Balice-Gordon R, Dalmau J (2010) Antibodies to the GABA(B) receptor in limbic encephalitis with seizures: case series and characterisation of the antigen. Lancet Neurol 9:67–76
Lancaster E, Leypoldt F, Titulaer MJ, Honnorat J, Waters PJ, Reindl M, Hoftberger R (2015) Immunoglobulin G antibodies to the N-methyl-d-aspartate receptor are distinct from immunoglobulin A and immunoglobulin M responses. Ann Neurol 77:183
Lennox BR, Palmer-Cooper EC, Pollak T, Hainsworth J, Marks J, Jacobson L, Lang B, Fox H, Ferry B, Scoriels L, Crowley H, Jones PB, Harrison PJ, Vincent A (2017) Prevalence and clinical characteristics of serum neuronal cell surface antibodies in first-episode psychosis: a case-control study. Lancet Psychiatry 4:42–48
Liimatainen S, Peltola M, Sabater L, Fallah M, Kharazmi E, Haapala AM, Dastidar P, Knip M, Saiz A, Peltola J (2010) Clinical significance of glutamic acid decarboxylase antibodies in patients with epilepsy. Epilepsia 51:760–767
Malter MP, Helmstaedter C, Urbach H, Vincent A, Bien CG (2010) Antibodies to glutamic acid decarboxylase define a form of limbic encephalitis. Ann Neurol 67:470–478
Meinck HM, Faber L, Morgenthaler N, Seissler J, Maile S, Butler M, Solimena M, DeCamilli P, Scherbaum WA (2001) Antibodies against glutamic acid decarboxylase: prevalence in neurological diseases. J Neurol Neurosurg Psychiatry 71:100–103
Mitoma H, Adhikari K, Aeschlimann D, Chattopadhyay P, Hadjivassiliou M, Hampe CS, Honnorat J, Joubert B, Kakei S, Lee J, Manto M, Matsunaga A, Mizusawa H, Nanri K, Shanmugarajah P, Yoneda M, Yuki N (2016) Consensus paper: neuroimmune mechanisms of cerebellar ataxias. Cerebellum 15:213–232
Muñoz-Lopetegi A, de Bruijn MA, Boukhrissi S, Bastiaansen AE, Nagtzaam MM, Hulsenboom ES, Boon AJ, Neuteboom RF, de Vries JM, Sillevis Smitt PA, Schreurs MW, Titulaer MJ (2020) Neurologic syndromes related to anti-GAD65: Clinical and serologic response to treatment. Neurol Neuroimmunol Neuroinflamm 7:e696
Nosadini M, Toldo I, Tascini B, Bien CG, Parmeggiani L, De Gaspari P, Zuliani L, Sartori S (2019) LGI1 and CASPR2 autoimmunity in children: systematic literature review and report of a young girl with Morvan syndrome. J Neuroimmunol 335:577008
O'Toole O, Lennon VA, Ahlskog JE, Matsumoto JY, Pittock SJ, Bower J, Fealey R, Lachance DH, McKeon A (2013) Autoimmune chorea in adults. Neurology 80:1133–1144
Popkirov S, Ismail FS, Gronheit W, Kapauer M, Wellmer J, Bien CG (2017) Progressive hippocampal sclerosis after viral encephalitis: potential role of NMDA receptor antibodies. Seizure 51:6–8
Rosenfeld MR, Titulaer MJ, Dalmau J (2012) Paraneoplastic syndromes and autoimmune encephalitis: five new things. Neurol Clin Pract 2:215–223
Saiz A, Blanco Y, Sabater L, Gonzalez F, Bataller L, Casamitjana R, Ramio-Torrenta L, Graus F (2008) Spectrum of neurological syndromes associated with glutamic acid decarboxylase antibodies: diagnostic clues for this association. Brain 131:2553–2563
Titulaer MJ, McCracken L, Gabilondo I, Armangue T, Glaser C, Iizuka T, Honig LS, Benseler SM, Kawachi I, Martinez-Hernandez E, Aguilar E, Gresa-Arribas N, Ryan-Florance N, Torrents A, Saiz A, Rosenfeld MR, Balice-Gordon R, Graus F, Dalmau J (2013) Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: an observational cohort study. Lancet Neurol 12:157–165
van Sonderen A, Ariño H, Petit-Pedrol M, Leypoldt F, Körtvélyessy P, Wandinger KP, Lancaster E, Wirtz PW, Schreurs MW, Sillevis Smitt PA, Graus F, Dalmau J, Titulaer MJ (2016) The clinical spectrum of Caspr2 antibody-associated disease. Neurology 87:521–528
van Sonderen A, Schreurs MW, de Bruijn MA, Boukhrissi S, Nagtzaam MM, Hulsenboom ES, Enting RH, Thijs RD, Wirtz PW, Sillevis Smitt PA, Titulaer MJ (2016) The relevance of VGKC positivity in the absence of LGI1 and Caspr2 antibodies. Neurology 86:1692–1699
van Sonderen A, Thijs RD, Coenders EC, Jiskoot LC, Sanchez E, de Bruijn MA, van Coevorden-Hameete MH, Wirtz PW, Schreurs MW, Sillevis Smitt PA, Titulaer MJ (2016) Anti-LGI1 encephalitis: clinical syndrome and long-term follow-up. Neurology 87:1449–1456
Wandinger KP, Saschenbrecker S, Stoecker W, Dalmau J (2011) Anti-NMDA-receptor encephalitis: a severe, multistage, treatable disorder presenting with psychosis. J Neuroimmunol 231:86–91
Acknowledgements
The authors would like to thank Mrs. Jutta Potthoff, Bielefeld, and Mrs. Kathrin Sipos, Vienna, for excellent technical and organizational assistance. The following colleagues kindly rated patients for the clinical data collection (all Germany if not otherwise stated): H. Baier, Ravensburg; F. Bauer, Munich; H. Bäzner, Stuttgart; J. Berrouschot, Altenburg; F. Bethke, Ibbenbüren; S. Beyenburg, Luxembourg, Luxembourg; R. Bitzer, Darmstadt; M. Bormann, Bremen; F. Borth, Hildesheim; F. Bösebeck, S. Ospina, Rotenburg; R. Brackmann, Herford; K. Brockmann, Göttingen; J. Bürmann, Homburg; A. Butnaru, Gütersloh; H. Dietzel, Damme; M. Dihné, Solingen; M. Friepörtner, Hamm; U. Goldammer, Hannover; P. Graneß, Berlin-Buch; F. Griesinger, Oldenburg; S. Guggenberger, Linz, Austria; C. G. Haase, Gelsenkirchen; S. Hennig, Hildesheim; R. Huber, Friedrichshafen; A. Kastrup, Bremen; P. Kermer, Sanderbusch; H. Klugkist, Emden; B. Korinth, Berlin; P. Körtvelyessy, Magdeburg; J. Kukolja, Wuppertal; S. Leiz, München; H. Lerche, Tübingen; H. Lode, Greifswald; H. Lohner, Rosenheim; C. Makowski, München; K. Mennicke, Rotenburg; A. Mey, Braunschweig; U. Neirich, Frankfurt; B. Neubauer, Gießen; D. Ostertag, Merzig; S. Paus, Bonn; J. Peters, München; I. Petrovic, Belgrade, Serbia; M. Pfeilstetter, Vogtareuth; G. Pilz, Salzburg, Austria; H. Pleuger, Schloss Holte-Stukenbrock; T. Postert, Paderborn; U. Pulkowski, Rendsburg; G. Puttinger, Linz, Austria; C. M. Quesada, Essen; K. Rieke, Hamm; M. W. Riepe, Günzburg; D. Sanner, Norden; P. Schelliger, Minden; M. Schimmel, Augsburg; H. M. Schippers, Nieuwegein, The Netherlands; S. Schultz, Hessisch Oldendorf; M. Seeck, Geneva, Switzerland; R. Seitz, Düsseldorf; B. Steinhoff, Kehl-Kork; W. Steinke, Düsseldorf; A. Strickler, Eisenach; B. Stüve, Köln; R. Trollmann, Erlangen; U. v. Mengershausen, St. Gallen, Switzerland; M. Voigtländer, Hamburg; C. von Arnim, Ulm; P. von Laer, Bielefeld; M. von Mering, Bremen; T. von Oertzen, Linz, Austria; R. von Wrede, Bonn; A. Weichselbaum, Tübingen; K. Wessel, Braunschweig; P. Zacher, Radeberg.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Dr. CG Bien obtained honoraria for speaking engagements from UCB, Desitin (Hamburg, Germany), and Euroimmun. He receives research support from Deutsche Forschungsgemeinschaft (German Research Council, Bonn, Germany) and Gerd-Altenhof-Stiftung (Deutsches Stiftungszentrum, Essen, Germany). Dr. M Holtkamp obtained speaker’s honoraria and/or consultancy fees from Arvelle, Bial, Desitin, Eisai, GW Pharmaceuticals, Novartis, and UCB. Dr. N Melzer has received honoraria for lecturing and travel expenses for attending meetings from Biogen Idec, GlaxoSmith Kline, Teva, Novartis Pharma, Bayer Healthcare, Genzyme, Alexion Pharmaceuticals, Fresenius Medical Care, Diamed, and BIAL, and has received financial research support from Euroimmun, Fresenius Medical Care, Diamed, Alexion Pharmaceuticals, and Novartis Pharma. Dr. F von Podewils obtained honoraria for speaking engagements from UCB, Eisai, and BIAL. Dr H Rauschka obtained honoraria for speaking engagements, consulting, serving on advisory boards and funding for conference travels from Biogen, Merck, Novartis, Roche, Sanofi and Teva-Ratiopharm. Dr. R Höftberger obtained honoraria for speaking engagements from Euroimmun and Novartis. She receives research support from the Jubiläumsfonds der Österreichischen Nationalbank, Project 16919, and the GBS/CIDP Foundation International. The Medical University of Vienna receives payments for antibody assays. The other authors report no conflicts of interest.
Ethics approval
The study was approved by the Ethics committee of the University of Münster, Germany (2017–005-f-S).
Consent to participate
Not applicable (retrospective evaluation, waived by Ethics committee).
Consent for publication
Not applicable (retrospective evaluation, waived by Ethics committee).
Availability of data and material
Any data not published within this article are available at the Epilepsy Center Bethel. Data will be shared upon request from any qualified investigator, maintaining anonymization of the patients.
Code availability
Not applicable.
Additional information
The original online version of this article was revised due to a retrospective Open Access order.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bien, C.G., Bien, C.I., Dogan Onugoren, M. et al. Routine diagnostics for neural antibodies, clinical correlates, treatment and functional outcome. J Neurol 267, 2101–2114 (2020). https://doi.org/10.1007/s00415-020-09814-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-020-09814-3