Abstract
Background and purpose
Cardiorespiratory fitness (CRF) is closely related to our health, but whether high cardiorespiratory fitness could reduce stroke risk remains controversial. We used a meta-analysis to examine the overall association between cardiorespiratory fitness and stroke incidence.
Methods
A systematic search was performed in PubMed, EMBASE, and Web of science. We estimated the overall relative risk (RR) of stroke incidence for high levels of CRF individuals versus individuals with low levels of CRF. Meanwhile, we made a quantitative analysis of the association between CRF and the risk of stroke.
Results
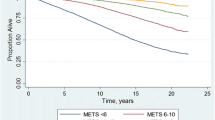
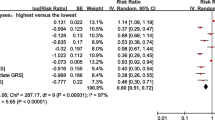
14 cohort studies containing 1,409,340 participants were included in this meta-analysis, and 23,894 stroke patients were observed. The meta-analysis documented that the high-CRF individuals had a 42% lower risk of stroke (RR_0.58; 95% CI 0.51–0.66) compared with low-CRF individuals. Besides, subgroup analysis showed that the inverse association of CRF with the risk of stroke was consistent. There are 29% lower risk of ischemic stroke (RR_0.71; 95% CI 0.54–0.93) and 31% lower risk of hemorrhagic stroke (RR_0.69; 95% CI 0.47–1.00). Dose–response analysis showed that every “unit-dose” increment of five metabolic equivalents (METs) reduced a 15% lower risk of stroke (RR_0.85; 95% CI 0.79–0.91).
Conclusion
This meta-analysis provides the evidence that better CRF was with a lower risk of stroke incidence.




Similar content being viewed by others
References
Myers J, McAuley P, Lavie CJ, Despres JP, Arena R, Kokkinos P (2015) Physical activity and cardiorespiratory fitness as major markers of cardiovascular risk: their independent and interwoven importance to health status. Prog Cardiovasc Dis 57(4):306–314. https://doi.org/10.1016/j.pcad.2014.09.011
Kodama S, Saito K, Tanaka S, Maki M, Yachi Y, Asumi M, Sugawara A, Totsuka K, Shimano H, Ohashi Y, Yamada N, Sone H (2009) Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. JAMA 301(19):2024–2035. https://doi.org/10.1001/jama.2009.681
Meschia JF, Bushnell C, Boden-Albala B, Braun LT, Bravata DM, Chaturvedi S, Creager MA, Eckel RH, Elkind MS, Fornage M, Goldstein LB, Greenberg SM, Horvath SE, Iadecola C, Jauch EC, Moore WS, Wilson JA, Stroke Council on C AHA, Stroke N, Council on Clinical C, Council on Functional G, Translational B, Council H (2014) Guidelines for the primary prevention of stroke: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 45(12):3754–3832. https://doi.org/10.1161/STR.0000000000000046
Haskell WL, Leon AS, Caspersen CJ, Froelicher VF, Hagberg JM, Harlan W, Holloszy JO, Regensteiner JG, Thompson PD, Washburn RA et al (1992) Cardiovascular benefits and assessment of physical activity and physical fitness in adults. Med Sci Sports Exerc 24(6 Suppl):S201–220
Hussain N, Gersh BJ, Carta KG, Sydo N, Lopez-Jimenez F, Kopecky SL, Thomas RJ, Asirvatham SJ, Allison TG (2018) Impact of cardiorespiratory fitness on frequency of atrial fibrillation, stroke, and all-cause mortality. Am J Cardiol 121(1):41–49
Wessel TR, Arant CB, Olson MB, Johnson BD, Reis SE, Sharaf BL, Shaw LJ, Handberg E, Sopko G, Kelsey SF, Pepine CJ, Merz NB (2004) Relationship of physical fitness vs body mass index with coronary artery disease and cardiovascular events in women. JAMA 292(10):1179–1187. https://doi.org/10.1001/jama.292.10.1179
Aberg ND, Kuhn HG, Nyberg J, Waern M, Friberg P, Svensson J, Toren K, Rosengren A, Aberg MA, Nilsson M (2015) Influence of cardiovascular fitness and muscle strength in early adulthood on long-term risk of stroke in Swedish men. Stroke 46(7):1769–1776. https://doi.org/10.1161/STROKEAHA.115.009008
Kurl S, Laukkanen JA, Niskanen L, Rauramaa R, Tuomainen TP, Sivenius J, Salonen JT (2005) Cardiac power during exercise and the risk of stroke in men. Stroke 36(4):820–824. https://doi.org/10.1161/01.STR.0000157592.82198.28
Sui X, Howard VJ, McDonnell MN, Ernstsen L, Flaherty ML, Hooker SP, Lavie CJ (2018) Racial differences in the association between nonexercise estimated cardiorespiratory fitness and incident stroke. Mayo Clin Proc 93(7):884–894
Hooker SP, Sui X, Colabianchi N, Vena J, Laditka J, LaMonte MJ, Blair SN (2008) Cardiorespiratory fitness as a predictor of fatal and nonfatal stroke in asymptomatic women and men. Stroke 39(11):2950–2957
Lee IM, Hennekens CH, Berger K, Buring JE, Manson JE (1999) Exercise and risk of stroke in male physicians. Stroke 30(1):1–6
Habibzadeh MR, Farzaneh-Far R, Sarna P, Na B, Schiller NB, Whooley MA (2010) Association of blood pressure and heart rate response during exercise with cardiovascular events in the Heart and Soul Study. J Hypertens 28(11):2236–2242. https://doi.org/10.1097/HJH.0b013e32833d455b
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 62(10):1006–1012. https://doi.org/10.1016/j.jclinepi.2009.06.005
Pierre-Louis B, Guddati AK, Syed MKH, Gorospe VE, Manguerra M, Bagchi C, Aronow WS, Ahn C (2014) Exercise capacity as an independent risk factor for adverse cardiovascular outcomes among nondiabetic and diabetic patients. Arch Med Sci 10(1):25–32. https://doi.org/10.5114/aoms.2014.40731
Patton JF, Vogel JA, Mello RP (1982) Evaluation of a maximal predictive cycle ergometer test of aerobic power. Eur J Appl Physiol 49(1):131–140. https://doi.org/10.1007/bf00428971
Jackson AS, Sui X, O'Connor DP, Church TS, Lee DC, Artero EG, Blair SN (2012) Longitudinal cardiorespiratory fitness algorithms for clinical settings. Am J Prev Med 43(5):512–519. https://doi.org/10.1016/j.amepre.2012.06.032
Kohl HW, Blair SN, Paffenbarger RS Jr, Macera CA, Kronenfeld JJ (1988) A mail survey of physical activity habits as related to measured physical fitness. Am J Epidemiol 127(6):1228–1239
Hlatky MA, Boineau RE, Higginbotham MB, Lee KL, Mark DB, Califf RM, Cobb FR, Pryor DB (1989) A brief self-administered questionnaire to determine functional capacity (the Duke Activity Status Index). Am J Cardiol 64(10):651–654
Orsini N, Li R, Wolk A, Khudyakov P, Spiegelman D (2012) Meta-analysis for linear and nonlinear dose-response relations: examples, an evaluation of approximations, and software. Am J Epidemiol 175(1):66–73. https://doi.org/10.1093/aje/kwr265
Kokkinos P (2014) Cardiorespiratory fitness, exercise, and blood pressure. Hypertension 64(6):1160–1164. https://doi.org/10.1161/HYPERTENSIONAHA.114.03616
Zaccardi F, O'Donovan G, Webb DR, Yates T, Kurl S, Khunti K, Davies MJ, Laukkanen JA (2015) Cardiorespiratory fitness and risk of type 2 diabetes mellitus: a 23-year cohort study and a meta-analysis of prospective studies. Atherosclerosis 243(1):131–137. https://doi.org/10.1016/j.atherosclerosis.2015.09.016
Fernstrom M, Fernberg U, Eliason G, Hurtig-Wennlof A (2017) Aerobic fitness is associated with low cardiovascular disease risk: the impact of lifestyle on early risk factors for atherosclerosis in young healthy Swedish individuals—the Lifestyle, Biomarker, and Atherosclerosis study. Vasc Health Risk Manag 13:91–99. https://doi.org/10.2147/VHRM.S125966
Parto P, Lavie CJ, Swift D, Sui X (2015) The role of cardiorespiratory fitness on plasma lipid levels. Expert Rev Cardiovasc Ther 13(11):1177–1183. https://doi.org/10.1586/14779072.2015.1092384
Bose A, O'Neal WT, Bennett A, Judd SE, Qureshi WT, Sui X, Howard VJ, Howard G, Soliman EZ (2017) Relation between estimated cardiorespiratory fitness and atrial fibrillation (from the reasons for geographic and racial differences in stroke study). Am J Cardiol 119(11):1776–1780. https://doi.org/10.1016/j.amjcard.2017.03.008
Boots EA, Schultz SA, Oh JM, Larson J, Edwards D, Cook D, Koscik RL, Dowling MN, Gallagher CL, Carlsson CM, Rowley HA, Bendlin BB, LaRue A, Asthana S, Hermann BP, Sager MA, Johnson SC, Okonkwo OC (2015) Cardiorespiratory fitness is associated with brain structure, cognition, and mood in a middle-aged cohort at risk for Alzheimer's disease. Brain Imaging Behav 9(3):639–649. https://doi.org/10.1007/s11682-014-9325-9
Hankey GJ (2017) Stroke. Lancet 389(10069):641–654. https://doi.org/10.1016/s0140-6736(16)30962-x
Madssen E, Skaug EA, Wisloff U, Ellingsen O, Videm V (2019) Inflammation is strongly associated with cardiorespiratory fitness, sex, BMI, and the metabolic syndrome in a self-reported healthy population: HUNT3 fitness study. Mayo Clin Proc. https://doi.org/10.1016/j.mayocp.2018.08.040
Tibaut M, Caprnda M, Kubatka P, Sinkovic A, Valentova V, Filipova S, Gazdikova K, Gaspar L, Mozos I, Egom EE, Rodrigo L, Kruzliak P, Petrovic D (2019) Markers of atherosclerosis: part 1—serological markers. Heart Lung Circ 28(5):667–677. https://doi.org/10.1016/j.hlc.2018.06.1057
Moriya J (2019) Critical roles of inflammation in atherosclerosis. J Cardiol 73(1):22–27. https://doi.org/10.1016/j.jjcc.2018.05.010
Eliakim A, Nemet D (2010) Exercise training, physical fitness and the growth hormone-insulin-like growth factor-1 axis and cytokine balance. Med Sport Sci 55:128–140. https://doi.org/10.1159/000321977
Traustadottir T, Davies SS, Su Y, Choi L, Brown-Borg HM, Roberts LJ 2nd, Harman SM (2012) Oxidative stress in older adults: effects of physical fitness. Age 34(4):969–982. https://doi.org/10.1007/s11357-011-9277-6
Lee S, Bacha F, Gungor N, Arslanian SA (2006) Cardiorespiratory fitness in youth: relationship to insulin sensitivity and beta-cell function. Obesity 14(9):1579–1585. https://doi.org/10.1038/oby.2006.182
Lee CD, Folsom AR, Blair SN (2003) Physical activity and stroke risk: a meta-analysis. Stroke 34(10):2475–2481. https://doi.org/10.1161/01.STR.0000091843.02517.9D
de Carvalho Souza Vieira M, Boing L, Leitao AE, Vieira G, Coutinho de Azevedo Guimaraes A (2018) Effect of physical exercise on the cardiorespiratory fitness of men—a systematic review and meta-analysis. Maturitas 115:23–30. https://doi.org/10.1016/j.maturitas.2018.06.006
Skinner JS, Jaskolski A, Jaskolska A, Krasnoff J, Gagnon J, Leon AS, Rao DC, Wilmore JH, Bouchard C, Study HF (2001) Age, sex, race, initial fitness, and response to training: the HERITAGE family study. J Appl Physiol 90(5):1770–1776. https://doi.org/10.1152/jappl.2001.90.5.1770
Jimenez MC, Manson JE, Cook NR, Kawachi I, Wassertheil-Smoller S, Haring B, Nassir R, Rhee JJ, Sealy-Jefferson S, Rexrode KM (2019) Racial variation in stroke risk among women by stroke risk factors. Stroke 50(4):797–804. https://doi.org/10.1161/STROKEAHA.117.017759
Howard VJ (2013) Reasons underlying racial differences in stroke incidence and mortality. Stroke 44(6 Suppl 1):S126–128. https://doi.org/10.1161/STROKEAHA.111.000691
Pandey A, Park BD, Ayers C, Das SR, Lakoski S, Matulevicius S, de Lemos JA, Berry JD (2016) Determinants of racial/ethnic differences in cardiorespiratory fitness (from the Dallas Heart Study). Am J Cardiol 118(4):499–503. https://doi.org/10.1016/j.amjcard.2016.05.043
Siconolfi SF, Lasater TM, Snow RC, Carleton RA (1985) Self-reported physical activity compared with maximal oxygen uptake. Am J Epidemiol 122(1):101–105
Duscha BD, Slentz CA, Johnson JL, Houmard JA, Bensimhon DR, Knetzger KJ, Kraus WE (2005) Effects of exercise training amount and intensity on peak oxygen consumption in middle-age men and women at risk for cardiovascular disease. Chest 128(4):2788–2793. https://doi.org/10.1378/chest.128.4.2788
Swift DL, Johannsen NM, Lavie CJ, Earnest CP, Johnson WD, Blair SN, Church TS, Newton RL Jr (1985) (2013) Racial differences in the response of cardiorespiratory fitness to aerobic exercise training in Caucasian and African American postmenopausal women. J Appl Physiol 114(10):1375–1382. https://doi.org/10.1152/japplphysiol.01077.2012
Sieverdes JC, Sui X, Lee D-c, Lee IM, Hooker SP, Blair SN (2011) Independent and joint associations of physical activity and fitness on stroke in men. Phys Sports Med 39(2):119–126
Talbot LA, Morrell CH, Metter EJ, Fleg JL (2002) Comparison of cardiorespiratory fitness versus leisure time physical activity as predictors of coronary events in men aged %3c or = 65 years and %3e 65 years. Am J Cardiol 89(10):1187–1192
Kim ES, Ishwaran H, Blackstone E, Lauer MS (2007) External prognostic validations and comparisons of age- and gender-adjusted exercise capacity predictions. J Am Coll Cardiol 50(19):1867–1875. https://doi.org/10.1016/j.jacc.2007.08.003
Ross R, Blair SN, Arena R, Church TS, Despres JP, Franklin BA, Haskell WL, Kaminsky LA, Levine BD, Lavie CJ, Myers J, Niebauer J, Sallis R, Sawada SS, Sui X, Wisloff U, American Heart Association Physical Activity Committee of the Council on L, Cardiometabolic H, Council on Clinical C, Council on E, Prevention, Council on C, Stroke N, Council on Functional G, Translational B, Stroke C (2016) Importance of Assessing cardiorespiratory fitness in clinical practice: a case for fitness as a clinical vital sign: a scientific statement from the American heart association. Circulation 134(24):e653–e699. https://doi.org/10.1161/CIR.0000000000000461
Funding
This work was supported by a grant from National Scientific Foundation of China NSFC81771961.
Author information
Authors and Affiliations
Contributions
YYW: conceptualized the study; ZYX, YYW and FL: design of study; YYW, FL and LGG: literature retrieval, study selection, data extraction, statistical analyses, interpretation of the data and drafting of the initial manuscript; YC: quality evaluation; ZYX: critical revision and comment for important intellectual content; all authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
All authors report no disclosures relevant to the manuscript.
Ethical standards
This article does not contain any studies with human participants performed by any of the authors. As a systematic review and meta-analysis, no ethical approval or consent to participate was required.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wang, Y., Li, F., Cheng, Y. et al. Cardiorespiratory fitness as a quantitative predictor of the risk of stroke: a dose–response meta-analysis. J Neurol 267, 491–501 (2020). https://doi.org/10.1007/s00415-019-09612-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-019-09612-6