Abstract
Background
Fifteen regional studies published over the last six decades surveying prevalence, mortality and hospital admissions have suggested that Scotland is amongst the highest risk nations for multiple sclerosis (MS) in the world. However, substantial intranational variation in rates (between regions) has been described in numerous countries, including in the only previous Scottish national survey, which used hospital admission data, to address this issue. Against this backdrop, the Scottish Multiple Sclerosis Register (SMSR) was established in 2010 to prospectively collect nationally comprehensive incidence data and to allow for regional comparisons.
Methods
Here, we present the SMSR and analyse the variation in crude and age–sex standardized incidence rates, lifetime risk (cumulative incidence), and the sex distribution of cases and rates, between the 14 administrative Health Boards or regions of Scotland: 01 January 2010 to 31 December 2017.
Results
The overall incidence rate for Scotland was 8.76/100,000 person-years (standardized: 8.54). Regional incidence rates varied significantly—up to threefold—between Health Boards (p < 1 × 10–13). The national female-to-male sex ratio was 2.3:1, but this too varied regionally (outlier regions result in a range from 1.0 to 4.2:1). Lifetime risk ranged from 19.9/1000 for females in Orkney (58.98°N) to 1.6/1000 for males in the Borders (55.60°N). Comparison with a previous national survey suggests that these differences are longstanding. In 6 of 14 regions the lifetime risk for women exceeds 1%.
Conclusions
This study introduces a national incidence register: a valuable research tool and the result of substantial public investment. The wide variation in incidence rates and sex ratios between regions, in a relatively homogenous population, raises questions for future study.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
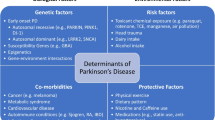
Broad consensus exists for genetic susceptibility interacting with potent environmental risk factors in the pathogenesis of multiple sclerosis (MS) [1,2,3]. Nevertheless, a detailed account of the causal chain remains elusive. One aspect of MS epidemiology that remains unexplained is the well recognized within-country regional variation in MS rates [4,5,6,7]. In many countries, differences in regional rates have been wide (up to tenfold) and persistent in the same regions across period cohorts, i.e. relative differences in regional rates persist despite different generations of patients being diagnosed by different generations of neurologists [5]. There may be an opportunity to identify novel contributors to aetiology by studying these variations, because the list of possible causes (genetic or environmental) is more limited between relatively similar sub-national regional populations than between disparate international ones. Addressing this, however, will require high quality and geographically precise epidemiological datasets that can guide targeted genetic, seroepidemiological, and biome research.
Scotland represents a powerful environment to study MS due its very high incidence of the disease. This is reflected in a strong history of Scottish MS epidemiological study over several decades. Fifteen surveys have been published since the first by Sutherland in 1956 [8], which have consistently shown a pattern of increasing prevalence and high rates by international standards [9, 10]. In addition, there are technical advantages particularly for making between-region comparisons in Scotland. These include a stable and homogeneous population of 5.3M, a unitary and free health-care provider system (NHS) and e-health infrastructural strengths such as a nationwide patient identifier (CHI) assigned at birth. The CHI enables lifelong tracking for all contact with public services including vaccinations, hospital admissions, prescriptions, etc., and consequently the creation and alignment of detailed datasets of social and health care interactions. However, only one study has attempted to document within-Scotland variation in rates using a national sample covering a single period [11].
In 2010, recognizing MS as an important public health problem, the Scottish Government established the Scottish MS Register (SMSR), a prospective incidence register, mandating the recording of all newly diagnosed cases of MS. The primary purpose was to ensure that all persons diagnosed with MS were offered contact with an MS specialist nurse within ten working days of diagnosis and, secondarily, to routinely and systematically collect comprehensive data for epidemiological research [12]. Our aims in this paper are twofold: first to present the SMSR to highlight its potential as a research tool, and second to analyse the first 8 years of incidence data captured therein to study the regional variability in MS rates between the 14 “Health Board” regions of Scotland.
Methods
Data
The SMSR aims for comprehensive ascertainment by coupling routine data collection with a continuous audit of service quality. The ten working day requirement is an “essential criteria” of a national standard [Standard 15.2 of the Clinical Standards for Neurology Services (2009)] which requires Health Boards to meet this target [13]. MS specialist nurses are obliged to report data on this outcome accurately and promptly after diagnosis which is then confirmed by the treating neurologist. Completeness and accuracy are continuously monitored by Information Services Division (ISD) of National Health Service (NHS) National Services Scotland (NSS).
Individual level SMSR data, including age, date and address at the time of diagnosis, were extracted in an anonymized form. Census data, publically available for Health Board populations, were used for the denominators for all calculations based on the Scottish national census 2011 (https://www.scotlandscensus.gov.uk/) [14].
Inclusion and exclusion criteria
Adults (legally persons ≥ 16 years old), newly diagnosed with MS in Scotland after 01/01/2010, as defined by the Revised McDonald Criteria 2005 [15], are routinely recorded on the SMSR. We included all those persons with MS (pwMS) on the register diagnosed up to 31 December 2017. Persons with possible MS or clinically isolated syndrome are excluded (https://www.msr.scot.nhs.uk/).
Health Board geography
Scotland has a universal health care system, publically owned and operated, free at the point of use (NHS). The great majority of health care in Scotland is delivered by the NHS. Private neurologists typically also work in the NHS (and refer to MS services via specialist nurses) and probably all pwMS in Scotland, who have been diagnosed, use some NHS services. NHS Scotland is separated into 14 territorial Health Boards which were the aggregate unit of geography used in this study. Health Board latitude was defined as the latitude of the administrative centre.
Ethics
Formal research ethics approval was not required as audit data were de-identified, but peer-review by the SMSR steering committee and independent internal (ISD) review by an NHS employed consultant of public health ensured the project was in line with the aims and objectives of the SMSR and consistent with usual public health practice for the use of routinely collected data obtained without explicit consent.
Statistical analyses
To allow for external comparisons unconfounded by population age–sex structure, direct-standardization of incidence rates was performed to the 2013 European Standard Population (ESP) (https://www.ons.gov.uk). Indirect standardization of regional rates was conducted using national rates as the referent for between-health-board comparisons. Maps were created using QGIS v2.18.23 using publicly available shapefiles (data.gov.uk). The cartogram was created using GeoDa v1.12.
Lifetime (risk) cumulative incidence rates (CIR) were calculated for each region as:
where i = age stratum, ID = incidence density for the ith age stratum, and wi = the width in years of the ith age stratum. This measure has the advantage of incorporating (in ID strata) the population size of the strata and so is comparable across populations of different age-structures. CIRs are the proportion of population affected over a given period, here calculated to reflect lifetime risk and are presented per 1000 persons.
Statistical significance was defined using an α of 0.05 throughout. Omnibus test of statistical significance of variation in rates by region was tested using a 14-sample Chi-squared test. Associations were inspected visually and where appropriate linear relationships were analysed using ordinary and weighted least squares regression models. Pearson’s correlation coefficients were generated for bivariate analyses. Simulated rates under a null hypothesis of complete spatial randomness were calculated by randomly allocating each of n = 3680 cases to Health Boards proportional to population size 100,000 times in order to create empirical distributions under the null. p values for observed rates occurring under the null were calculated by comparing observed rates to the empirically derived null distributions and correcting for m = 14 independent tests using the Bonferroni method (α/m). Statistical analyses, simulations and tests were conducted using R and R Studio (v. 3.5.1).
The dataset used here is available subject to approval of the SMSR steering committee and NHS NSS ISD.
Results
The Scottish MS Register
3680/3716 (99.0%) cases were included in the regional analyses with 36 persons excluded due to incomplete address data (Fig. 1).
The resident populations within Health Boards are presented in Table 1, showing regional variation in population number and density. The majority of Scotland’s population lives in the “central belt” which includes the two largest cities of Glasgow and Edinburgh. 98% of the Scottish population lives on the mainland and there are some 790 islands, 94 permanently inhabited which are broadly separated into four main island groups: The Outer Hebrides (which make up the Western Isles Health Board), The Inner Hebrides (which are grouped in the Highland Health Board), Orkney and Shetland.
Regional incidence 2010–2017
The incidence we refer to throughout this study is the incidence of diagnosis rather than the incidence of disease onset. The crude MS incidence rate for the Scottish population as a whole was 8.76/105 person-years (pys) (directly standardized to ESP, 8.54/105pys). The national crude incidence rate for females was 11.70/105 pys and for males 5.48/105 pys. The ratio of female case count to male was 2.27 (2.14 for adjusted rate ratio). The age range of subjects at the time of diagnosis was 65.8 years with mean age of 41.34 (SD 12.03) years and median of 40 years. Age-specific incidence rates (Fig. 2) were used to calculate indirectly age-standardized incidence rates (supplementary Table 1).
Crude and indirectly age-standardized rates by Health Board, over the study period, are presented in Table 1 and Fig. 3, demonstrating significant variation in the incidence rate by region (\(X_{{13}}^{2} = 94.7\), two-sided p < 1 × 10–13). Orkney was the highest incidence region in Scotland and there was good agreement between crude and standardized rates indicating that differences in population age-structure were not large contributors to apparent differences in rates. Lanarkshire (6.34), the Borders (6.66), Lothian (6.85) and Greater Glasgow and Clyde (7.21) formed a contiguous band of the lowest incidence regions, with adjusted rates approximately one-third that of Orkney (18.35) and one-half that of Shetland (11.01), Highland (12.07) and Tayside (12.81), the latter being the highest incidence region on the mainland.
Age-adjusted incidence rates by Health Board for period 2010–2017. (Right) cartogram of count of cases (colour) by population-weighted datazone (size), demonstrating distribution of population-at-risk and cases of MS with concentration in the “central belt” (the region containing Glasgow and Edinburgh). Population-weighted “datazones” are small areal units of geography comprising several postcodes with mean population ~ 800 persons
Our finding of differences in incidence rates by region agree with those previously estimated by Handel et al. [11] using a different method for case ascertainment [hospital admissions—Scottish Morbidity Records 01 (SMR01)]. We replicate the threefold between-health-board variation described in that study (r = 0.85, p < 0.001), finding the same regions to be high and low incidence, despite the different patient cohort: 1997–2009 in Handel et al. [11] and 2010–2017 in our study.
We considered whether ascertainment discrepancies, arising from systematic differences in time from first symptoms to diagnosis, might have contributed to these results and we hypothesized that, if so, this might be reflected in differences in distribution of age at diagnosis (Fig. 4). Whilst visual inspection did not suggest obvious systematic differences between groups, omnibus testing of the age distribution by region using Kruskal–Wallis test demonstrated a significant difference (\(X_{{14}}^{2}\) = 33.6, p = 0.002). However, this was not unexpected given the large number of cases and power to detect small deviations from uniformity, and in post hoc (Dunn’s) analyses only two (of 91) pairwise comparisons yielded a significant difference after correcting for multiple testing using the false discovery method: the median diagnosis in Glasgow occurred significantly earlier than in Forth Valley (+ 3.3 years, p = 0.02) and in Grampian (+ 3.7 years, p = 0.01) Health Boards.
In addition to variation in incidence rates, we found variation in the sex ratio of cases between regions (Table 2) albeit this was chiefly driven by two outlier regions in the Borders and Shetland: there was no significant difference across all regions \((X_{{13}}^{2} = 16.6,~p = 0.22)\). The (F:M) sex ratio was most equitable in Shetland 1.0 (n = 10:10, lat = 60.39°N) and most inequitable in the borders 4.18 (n = 46:11, lat = 55.58°N). Adjusting for differences in regional population age–sex structure accounted for little of this difference. A significant negative linear relationship of sex ratio on latitude was detected by ordinary least squares regression (β = − 1.30, p = 0.03)—i.e. relatively more females were affected at lower latitudes and the sex ratio was more equitable at higher latitudes. However, again the outliers drive this effect. No significant linear trend with latitude exists amongst the other Health Boards after excluding Shetland and the Borders (β = − 0.94, p = 0.56) and both areas have low numbers of cases. The effect is similarly not significant when accounting for population in weighted analyses (β = − 0.88, p = 0.09).
We found that the lifetime risk of MS in Scotland is 6.55 per 1000 persons for the country as a whole and, whilst the sex ratio varies regionally, in each region the lifetime risk for females is higher than for males. However, the degree of variation in incidence is such that the lifetime risk for males in Shetland (8.63), Orkney (7.94) and Tayside (6.89) is higher than for females in some other areas (for example, Lanarkshire (6.60), Lothian (6.98), and Greater Glasgow and Clyde (7.56)). Table 3 presents the calculated male, female and combined lifetime risk (CIR) by Health Board.
Discussion
This work provides the first report of standardized regional incidence rates for MS in Scotland based on the recently established SMSR which is the result of substantial far-sighted public investment. The high level of completeness of these data (99% for age, sex and address at diagnosis) is a result of mandatory reporting, the CHI system which incorporates sex and date of birth, and the importance of current address for the functioning of normal service within the NHS.
This study builds on a strong track record of several decades of MS epidemiological surveys in Scotland and utilizes the SMSR for its particular advantages for aetiological investigation: chiefly, that the register is truly national, is aiming for complete ascertainment, and has a prospective, incidence design. Until the recent emergence of disease-modifying treatments (DMTs), prevalence, mortality, hospital admission and even disability pensioning rates were comparable across regions relatively unaffected by differences in medical services available. However, an improved therapeutic arsenal now potentially confounds comparisons of these rates as regional discrepancies in care provision or practice may now also affect disability, admissions and survival. A strength, therefore, is that the SMSR captures incidence data, which is inherently more biologically meaningful than other rates—especially in the era of DMTs.
The national crude incidence rate of 8.71/105 pys confirms Scotland as a high-incidence nation, although not the highest reported internationally. The standardized incidence we report (8.54) is lower than recent studies from other high-income countries. For example, in Denmark at 9.43 (95% CI 9.17–9.69) [16] and Wales at 9.10 (95% CI 8.80–9.40) [17] per 105 pys. However, given the incidence register excludes possible MS and all cases are confirmed as definite by the diagnosing neurologist, it is likely that the rates we present reflect a lower bound on the estimate of the full burden of the condition in Scotland. Further, newly recognized clinical entities (such as neuromyelitis optica spectrum disorders), which in previous generations may have been included for calculation of MS rates, will now not be included. Caution may be merited in comparing these rates to those obtained in other settings by different methods. Our data support the assessment of the Scottish Public Health Observatory, that the SMSR is now the gold standard estimates of incidence in Scotland [18].
Given substantial regional variation, previous published estimates extrapolating prevalence from samples taken from single regions and/or using other methods may have erroneously estimated the burden of the disease in Scotland. Choice of index region and method of ascertainment are important potential sources for bias. A previous estimate, for example, of 10,000 prevalent cases would only be plausible if our figures represented an epidemic since 2010 and we suspect this to be a large underestimate [19]. Another estimate of 13,328 pwMS in 2010 derived from GP data supported by hospital episode data [10] appears more plausible. However, by roughly extrapolating prevalence from these incidence data, using life-expectancy and estimates of effects of MS diagnosis on early mortality [20], we suspect that this may also fall short. A recent study, using administrative data in the USA, has suggested that the prevalence of MS there may be as high as double that previously reported [21]. Similarly, we suspect that the burden of MS in Scotland may have been underestimated.
Our finding of differences in incidence rates by region agree with those estimated by Handel et al. [11] using different methods (hospital admissions) and our simulations demonstrate these differences are unlikely to have arisen due to chance (Table 1 and supplementary Fig. 1). This correlation between studies across distinct periods is externally consistent with reports of regional variability persisting across generations in other countries (where intergenerational correlation has been reported as r ~ 0.8) [6]. The consistency across two methods—our study corroborating their findings of threefold variation (r = 0.85, p < 0.001), finding the same regions to be high and low incidence, whilst using a more robust dataset, and in a different patient cohort—leads us to conclude that regional variation in Scotland is real, persistent and not explained by chance or bias.
In fact, a limitation of our methods is that address at the time of diagnosis is presumed to be an imperfect proxy for address at the time of onset and at the time of exposure to environmental risk factors [22]. Our study would thus be strengthened by data on pre-diagnosis location of residence. We would expect the imperfect correlation between location of residence at diagnosis and exposure to have diluted regional variation and so, despite finding large variations, we may have underestimated the extent of this effect.
The regional variation, even on the relatively ancestrally homogenous mainland, we find to be surprisingly large. Regional differences in CIR, which can be interpreted as a hypothetical lifetime risk, range substantially, from 19.9/1000 for females in Orkney (55.98°N) to 1.7/1000 for males in the Borders (55.60°N) (Table 3). And in 6 of 14 Scottish Health Boards the lifetime risk for women exceeds 1%. However, surprisingly, variation in incidence and sex ratio is of the degree that in some Health Boards of Scotland the lifetime risk for men exceeds the lifetime risk for women in other regions, despite an overall sex ratio of 2.3 (at the expense of women).
The variation in sex ratio between regions may be the result of chance. The negative correlation between sex ratio and latitude (greater proportion of females at low latitudes) in our unweighted analyses is in line with international trends [23]. However, the Borders and Shetland are outlier regions. No convincing linear relationship between sex ratio and latitude exists outwith these areas or on weighted analyses. However, the sex ratio of MS has been reported to have changed over decades, for example, in Canada [24] and Denmark [16], implicating changes in an environmental risk factor(s) for which males and females have differential sensitivity or exposures. Therefore, analysis of the regional sex ratio of future cases may be informative in demonstrating that these outliers arose due to chance, as we cannot yet exclude the possibility that they are the product of some local environmental factor.
Latitude predicts only a small proportion of the total variability in Scotland, but does remain significant even after controlling for population age–sex structure. This is perhaps in contrast to other Western European countries where it has been suggested that latitude’s association with incidence has diminished over time or was artefactually overestimated due to ascertainment issues or failure to standardize populations [25]. However, as northern populations in Scotland are typically more rural and have more outdoor work, it has been questioned—with empirical support—as to whether vitamin D levels robustly correlate with latitude in Scotland [26]. In addition, the lower incidence in Shetland, by far the most northerly point in Scotland, compared to Orkney and Tayside, raises further questions [26]. The remoteness of Shetland, with its distinct ancestry and—to an extent—culture, could explain the deviation from the general trend. However, this phenomenon, of a reversal of the latitude effect at extreme high latitudes, is actually consistent with international reports. For example, the same reversal has been noted in Scandinavia and Russia [25]. Nevertheless, even if some other factor explains the proportion of variation associated with latitude in the rest of Scotland, it is our opinion that this would not be any evidence against the importance of hypovitaminosis D in general, given international trends and multiple lines of evidence [27]. Hypovitaminosis D is widely prevalent in Scotland and may significantly contribute to the burden of MS [26].
This study uses routinely collected data with attendant methodological limitations. For example, it is not possible to exclude some regional variation in case ascertainment, although overall ascertainment is thought to be high suggesting that any such variation is probably small. Also, whilst the mean age at diagnosis (41.34 years) was somewhat higher in our study than in a clinically validated cohort from the UK MS register that does not include pwMS in Scotland (37.4 years) [28], the similar patterns of age at diagnosis across Health Boards is an argument against there being systematic differences in diagnostic efficiency by region in Scotland. Possible explanations for this discrepancy include: differences in proportions of patients by type of MS at onset in these two cohorts, an ageing population, truncation of the SMSR at young ages due to exclusion of cases with paediatric onset (age < 16 years old), and/or delays in diagnosis due to waiting times to see a neurologist. For example, it may be that younger median age at diagnosis in Glasgow, the only region where post hoc testing identified a significant difference (relative to two other areas), could, in part, reflect access to tertiary neurological care or waiting times to see neurologists. However, local differences in services and diagnostic preferences (e.g. propensity to request a lumbar puncture prior to diagnosis), and/or net rural-to-urban migration skewing the population-at-risk, will also be contributory factors, in addition to chance variation.
Conclusion
This paper presents the first 8 years of the SMSR, a prospective national incidence register. We confirm the high incidence of MS in Scotland, suggest that previous estimates of prevalence are likely underestimates, and corroborate previous reports of threefold variation by Health Board region suggesting these differences are both persistent and real. This has implications for service provision and supports further study to better understand the basis of regional variability. It raises the possibility that biologically important risk factors may be variably distributed in Scotland, at least regionally, and future work is now possible to determine if variation exists at a more local scale.
References
Ascherio A, Munger K (2008) Epidemiology of multiple sclerosis: from risk factors to prevention. Semin Neurol 28:017–28. https://doi.org/10.1055/s-2007-1019126
Banwell B, Bar-Or A, Arnold DL et al (2011) Clinical, environmental, and genetic determinants of multiple sclerosis in children with acute demyelination: a prospective national cohort study. Lancet Neurol 10:436–445. https://doi.org/10.1016/S1474-4422(11)70045-X
O’Gorman C, Lucas R, Taylor B (2012) Environmental risk factors for multiple sclerosis: a review with a focus on molecular mechanisms. Int J Mol Sci 13:11718–11752. https://doi.org/10.3390/ijms130911718
Wikström J, Palo J (1976) Studies on the geographic clustering of multiple sclerosis and optic neuritis in Finland. J Neurol. https://doi.org/10.1007/BF00313269
Kurtzke JF (1977) Geography in multiple sclerosis. J Neurol 215:1–26. https://doi.org/10.1007/BF00312546
Kurtzke JF (2000) Multiple sclerosis in time and space-geographic clues to cause. J Neurovirol 6(Suppl 2):S134–S140
Ebers G (2013) Interactions of environment and genes in multiple sclerosis. J Neurol Sci 334:161–163. https://doi.org/10.1016/j.jns.2013.08.018
Sutherland JM (1956) Observations on the prevalence of multiple sclerosis in Northern Scotland. Brain 79:635–654
Visser EM, Wilde K, Wilson JF et al (2012) A new prevalence study of multiple sclerosis in Orkney, Shetland and Aberdeen city. J Neurol Neurosurg Psychiatry 83:719–724. https://doi.org/10.1136/jnnp-2011-301546
Mackenzie IS, Morant SV, Bloomfield GA et al (2014) Incidence and prevalence of multiple sclerosis in the UK 1990–2010: a descriptive study in the General Practice Research Database. J Neurol Neurosurg Psychiatry 85:76–84. https://doi.org/10.1136/jnnp-2013-305450
Handel AE, Jarvis L, McLaughlin R et al (2011) The epidemiology of multiple sclerosis in Scotland: inferences from hospital admissions. PLoS ONE 6:e14606. https://doi.org/10.1371/journal.pone.0014606
SMSR Steering Group (2015) Scottish Multiple Sclerosis Register National Report 2015. https://www.msr.scot.nhs.uk/Reports/docs/scottish-ms-register-report-2015.pdf. Accessed 10 June 2019
NHS Quality Improvement Scotland (2009) Clinical Standards for Neurological Health Services. http://www.healthcareimprovementscotland.org/our_work/long_term_conditions/neurological_health_services/neurological_standards_2009.aspx. Accessed 10 June 2019
National Records of Scotland (2011) Scotland census 2011. https://www.scotlandscensus.gov.uk/. Accessed 27 May 2019
Polman CH, Reingold SC, Edan G et al (2005) Diagnostic criteria for multiple sclerosis: 2005 revisions to the “McDonald Criteria”. Ann Neurol 58:840–846. https://doi.org/10.1002/ana.20703
Koch-Henriksen N, Thygesen LC, Stenager E et al (2018) Incidence of MS has increased markedly over six decades in Denmark particularly with late onset and in women. Neurology 90:e1954–e1963. https://doi.org/10.1212/WNL.0000000000005612
Balbuena LD, Middleton RM, Tuite-Dalton K et al (2016) Sunshine, sea, and season of birth: MS incidence in Wales. PLoS ONE. https://doi.org/10.1371/journal.pone
Scottish Public Health Observatory (2019) Multiple Sclerosis: key points. https://www.scotpho.org.uk/health-wellbeing-and-disease/multiple-sclerosis/key-points/. Accessed 1 May 2019
Browne P, Chandraratna D, Angood C, Atlas of multiple sclerosis et al (2013) A growing global problem with widespread inequity. Neurology 2014:83. https://doi.org/10.1212/WNL.0000000000000768
Lunde HMB, Assmus J, Myhr KM et al (2017) Survival and cause of death in multiple sclerosis: a 60-year longitudinal population study. J Neurol Neurosurg Psychiatry 88:621–625. https://doi.org/10.1136/jnnp-2016-315238
Wallin MT, Culpepper WJ, Campbell JD et al (2019) The prevalence of MS in the United States: a population-based estimate using health claims data. Neurology 92:e1029–e1040. https://doi.org/10.1212/WNL.0000000000007035
Gale CR, Martyn CN (1995) Migrant studies in multiple sclerosis. Prog Neurobiol 47:425–448
Koch-Henriksen N, Sørensen PS (2010) The changing demographic pattern of multiple sclerosis epidemiology. Lancet Neurol 9:520–532. https://doi.org/10.1016/S1474-4422(10)70064-8
Orton S-M, Herrera BM, Yee IM et al (2006) Sex ratio of multiple sclerosis in Canada: a longitudinal study. Lancet Neurol 5:932–936. https://doi.org/10.1016/S1474-4422(06)70581-6
Simpson S, Blizzard L, Otahal P et al (2011) Latitude is significantly associated with the prevalence of multiple sclerosis: a meta-analysis. J Neurol Neurosurg Psychiatry 82:1132–1141. https://doi.org/10.1136/jnnp.2011.240432
Weiss E, Zgaga L, Read S et al (2016) Farming, foreign holidays, and vitamin D in Orkney. PLoS ONEe. https://doi.org/10.1371/journal.pone.0155633
Gianfrancesco MA, Stridh P, Rhead B et al (2017) Evidence for a causal relationship between low vitamin D, high BMI, and pediatric-onset MS. Neurology 88:1623–1629. https://doi.org/10.1212/WNL.0000000000003849
Middleton RM, Rodgers WJ, Chataway J et al (2018) Validating the portal population of the United Kingdom Multiple Sclerosis Register. Mult Scler Relat Disord 24:3–10. https://doi.org/10.1016/J.MSARD.2018.05.015
Rothman KJ, Greenland S, Lash TL (2008) Modern epidemiology, 3rd edn. Lippincott Williams & Wilkins (LWW), Boston
Acknowledgements
These data were diligently collected by Multiple Sclerosis specialist nurses and we are grateful to them for their hard work which was critical in making this study possible.
Funding
This study received no funding support.
Author information
Authors and Affiliations
Contributions
Conceptualization and first draft of manuscript: PK. Design and development of methodology: PK, AA, PC, MCC. Formal analysis: PK and MP. SMSR administration: MP, MON, CW, NMcD. Development of design of analysis: PK, CD, TC, JW, NMcD, PC, DP, IY, JMcD, AA. Acquisition of data: PK, MON, MP, CW, JOR, BW and NMcD. Visualization: PK. Supervision: AA, PC, MCC, SC. Development of initial analysis and interpretation of data: all. Substantial critical revision of all subsequent versions of manuscript: all. Final approval: all.
Corresponding author
Ethics declarations
Conflicts of interest
All authors have completed the ICMJE uniform disclosure form at https://www.icmje.org/coi_disclosure.pdf and declare: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Ethical standards
This study used de-identified, routinely collected data and includes no identifiable or individual data in the manuscript. Ethical approval was therefore not required although internal peer-review by the SMSR steering committee and independent internal review by an NHS employed consultant of public health ensured the project was in line with the aims and objectives of the SMSR and consistent with usual public health practice for the use of routinely collected data obtained without explicit consent.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Kearns, P.K.A., Paton, M., O’Neill, M. et al. Regional variation in the incidence rate and sex ratio of multiple sclerosis in Scotland 2010–2017: findings from the Scottish Multiple Sclerosis Register. J Neurol 266, 2376–2386 (2019). https://doi.org/10.1007/s00415-019-09413-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-019-09413-x