Abstract
In patients with sudden severe headache and a negative computed tomography (CT) scan, a lumbar puncture (LP) is performed to rule in or out a subarachnoid haemorrhage (SAH), but this procedure is under debate. In a hospital-based series of 30 patients with sudden headache, a negative CT scan but a positive LP (defined as detection of bilirubin >0.05 at wavelength 458 nm), we studied the chance of harbouring an aneurysm and the clinical outcome. Aneurysms were found in none of both patients who presented within 3 days, in 8 of the 18 (44%) who presented within 4–7 days and in 5 of the 10 (50%) who presented within 8–14 days. Of the 13 patients with an aneurysm, 3 (23%) had poor outcome. In patients who present late after sudden headache, the yield in terms of aneurysms is high in those who have a positive lumbar puncture. In patients with an aneurysm as cause of the positive lumbar puncture, outcome is in the same range as in SAH patients admitted in good clinical condition.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Around one of every ten patients presenting with a sudden severe headache in general practice has a subarachnoid haemorrhage (SAH) [1]. Computed tomography (CT) scanning of the brain can confirm the diagnosis in most but not all instances. In particular, in patients who present late, CT can be non-diagnostic, because the sensitivity of CT for subarachnoid blood decreases over time from nearly 100% in the initial hours [2–4] to 50% after 1 week [4]. To exclude SAH in patients with a negative CT scan, cerebrospinal fluid (CSF) is investigated to detect bilirubin pigments. The added value of CSF examination in patients with a negative CT is, however, a matter of debate because of the small likelihood of SAH in these patients [5]. In addition to the small likelihood of SAH, the likelihood of a ruptured aneurysm may be even smaller. Patients with nonaneurysmal subarachnoid haemorrhage, such as patients with perimesencephalic SAH, have usually headache only and no focal deficits or disturbed consciousness, and may present later than patients with more severe clinical symptoms. Patients with nonaneurysmal subarachnoid haemorrhage may therefore be overrepresented in late-arriving patients with a negative CT scan. We studied clinical characteristics and the chance of harbouring an aneurysm in this group of patients.
Methods
Patients were retrieved from the SAH database from the University Hospital Utrecht and from the files of the Laboratory of Clinical Chemistry, including CSF spectrophotometric investigations in the period 2002–2007. We included patients who had a history of sudden severe headache and a negative CT scan of the brain at initial assessment, but who had extinction of bilirubin >0.05 (at wavelength 458 nm) in their CSF, according to the guidelines for analysis of cerebrospinal fluid for bilirubin in suspected subarachnoid haemorrhage [6].
All patients with the diagnosis of SAH based on a positive CSF examination were investigated with CT angiography (CTA), magnetic resonance imaging (MRA) or conventional angiography to confirm or exclude an aneurysm as the cause of the bleeding.
The CSF from patients inside our hospital was protected from (day)light by wrapping them in aluminium foil, and centrifuged at 1,500 rpm during 10 min. The supernatant was stored at 4°C until analysis. CSF investigations were performed using a Beckman DU 650 spectrophotometer (Beckman Coulter, The Netherlands).
For the included patients, we describe clinical characteristics and the results of the radiological investigations. Clinical condition of the patients was assessed according to the World Federation of Neurological Surgeons (WFNS) scale on admission [7]. We analysed data according to the interval of symptoms and presentation in the hospital: (1) early presentation (0–3 days), (2) intermediate presentation (4–7 days) and (3) late presentation (8–14 days). The modified Rankin scale was used to describe outcome in all patients; we dichotomized grade 0–3 as good outcome and grade 4 and 5 as poor outcome [8].
Results
During the study period 30 patients had been admitted with sudden severe headache or neck pain and a brain CT scan without subarachnoid blood but CSF stained with bilirubin. In total, 775 patients with SAH were admitted during this period in our hospital. Sixteen patients were men, and 14 were women. Median age was 50.9 years (range 27.3–72.9 years). On admission, WFNS score was 1 in all but one patient (who had WFNS score 2 and a slight hemiparesis). Of the total group, two patients (7%) presented early, within 3 days. Further investigation did not show any aneurysms in this group. The cause of the delay in the other patients was due to the patient (in 8), the doctor (in 11), or both (in 2) or unknown (in 7). Eighteen patients presented within 4–7 days, and eight of these (44%) had an aneurysm. Ten patients presented late (8–14 days), and five of them (50%) proved to have an aneurysm. Thus, in the total group of 30 patients, an aneurysm was found in 13 (43%) patients (Table 1).
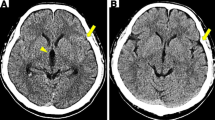
The CT scans of patients from the outside hospitals who were referred to our hospital were judged as normal by the radiologist from the outside hospital, but after revision by the neuroradiologist in our hospital (a tertiary referral hospital) slight abnormalities in 4 of 30 included patients were detected: 1 patient had a small hyperdensity in the left cerebellum, caused by an underlying arteriovenous malformation that was confirmed by angiography. This finding was not appreciated on the initial non-contrast CT scan by the radiologist from the outside hospital. One other patient had some sedimentation of blood in the posterior horns. Two other patients had ambiguous findings: suspicion of small amount of blood in the pentagon in two patients.
One other patient had on further follow-up with MRI a small hyperdensity in the parieto-occipital gyrus (not visible on contrast CT scan). Further investigations revealed an right subcortical aberrant vein in this patient draining to the sagittal sinus, without aneurysm.
All 16 patients without an aneurysm or arteriovenous malformation of the cause of their headache were investigated with CTA, MRI or MRA or additional four-vessel angiography (11 patients). In none of these 11 patients was focal or diffuse segmental arterial vasoconstriction shown.
Haematocrit was normal in 29 patients and not known in 1 patient. Serum bilirubin was measured in only one patient (who was pregnant).
Treatment of the aneurysm was done by coiling in nine patients and clipping in two. Two patients were not treated: one patient who developed ischaemia the day after admission and was in poor clinical condition, and one other patient who refused further angiography after MRA. The arteriovenous malformation in the cerebellum in one other patient was embolized successfully.
Eleven patients with an aneurysm were alive after 3 months and two died, because of rebleeding (1 patient) and secondary ischaemia (1 patient). One patient had a poor outcome with major neurological deficits including paresis and aphasia (because of secondary ischaemia). All patients without an aneurysm detected were alive after 2–7 years of follow-up and had good outcome without further episodes of SAH (Table 1).
Discussion
In our series of patients with sudden headache with a negative brain CT scan but a positive lumbar puncture with bilirubin pigments, nearly half had a ruptured aneurysm. The group of patients presenting within 3 days who did not show an aneurysm was very small. We think that, in general, the chance of an aneurysm is small in patients who present early after the onset of headache and who have a negative CT scan and a positive lumbar puncture because of the overall small chance of very early reabsorption of blood on CT. In patients who present later, the chance of reabsorption is larger, with blood being no longer detectable on CT. For patients presenting later, the results of our study show a high yield in terms of aneurysms and underscore the importance of examining CSF in patients with acute headache but a ‘negative’ brain CT scan.
The outcome of patients with a negative CT but a positive lumbar puncture and an aneurysm detected was comparable to that of patients with SAH detected on CT scan admitted in a good clinical condition [9–11]. The occurrence of rebleeding, secondary ischaemia and poor outcome in our series shows that the aneurysms detected were truly ruptured aneurysms and not incidental aneurysms found after a false-positive CSF exam.
In our study, 2 of the 30 CT scans that were read as normal in a local hospital were positive for SAH when reviewed in our hospital, and 2 other CT scans were assessed as ambiguous. In a recent paper on examination of patients with acute headache in tertiary care emergency departments in Canada, negative predictive value of CT scanning within 6 h after onset of headache was 100% (99.5–100%) [12]. The data from our study show that the negative predictive value of CT scanning is less in local hospitals, at least in The Netherlands, because several CT scans that were read as negative in local hospitals were positive or at least ambiguous after revision in our hospital. These results reflect clinical practice. In referring hospitals and during out-of-office hours, sensitivity of CT readers is apparently less optimal than during office hours in a highly specialized centre [4]. Another reason for false-negative CT scans is a low haematocrit (<30%) [4]. In our patients haematocrit was normal. A false-positive CSF examination after a negative CT could also be explained by a high serum bilirubin, transferred through the blood–brain barrier, resulting in a high CSF bilirubin [13]. This chance is, however, very small in patients without clinically overt jaundice, which is correlated to a lower range of hyperbilirubinaemia than xanthochromia.
In conclusion, CSF analysis including spectrophotometry, according to the guidelines [6], is mandatory in patients with acute headache but a CT scan negative for subarachnoid blood to rule out an SAH and an underlying ruptured aneurysm. This holds true in particular in patients who present late after the onset of headache. In patients who present early after the onset of headache, CT scans may be falsely considered negative because of insufficient scan techniques or less experience of the radiologist. Thus, also in patients presenting early after onset of headache, CSF examination remains pivotal after a CT scan being read as negative. For this category of patients immediate referral to a tertiary care centre might be an alternative, although this will increase the workload in these centres considerably.
References
Linn FHH, Wijdicks EFM, van der Graaf Y, Weerdesteyn-van Vliet FAC, Bartelds AIM, van Gijn J (1994) Prospective study of sentinel headache in aneurysmal subarachnoid haemorrhage. Lancet 344:590–593
Byyny RL, Mower WR, Shum N, Gabayan GZ, Fang S, Baraff LJ (2008) Sensitivity of noncontrast cranial computed tomography for the emergency department diagnosis of subarachnoid hemorrhage. Ann Emerg Med 51:697–703
Cortnum S, Sorensen P, Jorgensen J (2010) Determining the sensitivity of computed tomography scanning in early detection of subarachnoid hemorrhage. Neurosurgery 66:900–902
Edlow JA, Malek AM, Ogilvy CS (2008) Aneurysmal subarachnoid hemorrhage: update for emergency physicians. J Emerg Med 34:237–251
Coats TJ, Loffhagen R (2006) Diagnosis of subarachnoid haemorrhage following a negative computed tomography for acute headache: a Bayesian analysis. Eur J Emerg Med 13:80–83
Cruickshank A, Auld P, Beetham R, Burrows G, Egner W, Holbrook I, Keir G, Lewis E, Patel D, Watson I, White P (2008) Revised national guidelines for analysis of cerebrospinal fluid for bilirubin in suspected subarachnoid haemorrhage. Ann Clin Biochem 45:238–244
(1988) Report of World Federation of Neurological Surgeons Committee on a Universal Subarachnoid Hemorrhage Grading Scale. J Neurosurg 68:985–986
van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J (1988) Interobserver agreement for the assessment of handicap in stroke patients. Stroke 19:604–607
van Heuven AW, Dorhout Mees SM, Algra A, Rinkel GJ (2008) Validation of a prognostic subarachnoid hemorrhage grading scale derived directly from the Glasgow Coma Scale. Stroke 39:1347–1348
Dankbaar JW, de Rooij NK, Rijsdijk M, Velthuis BK, Frijns CJ, Rinkel GJ, van der Schaaf IC (2010) Diagnostic threshold values of cerebral perfusion measured with computed tomography for delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. Stroke 41:1927–1932
Bakker AM, Dorhout Mees SM, Algra A, Rinkel GJ (2007) Extent of acute hydrocephalus after aneurysmal subarachnoid hemorrhage as a risk factor for delayed cerebral infarction. Stroke 38:2496–2499
Perry JJ, Stiell IG, Sivilotti ML, Bullard MJ, Emond M, Symington C, Sutherland J, Worster A, Hohl C, Lee JS, Eisenhauer MA, Mortensen M, Mackey D, Pauls M, Lesiuk H, Wells GA (2011) Sensitivity of computed tomography performed within six hours of onset of headache for diagnosis of subarachnoid haemorrhage: prospective cohort study. BMJ 343:d4277
Seehusen DA, Reeves MM, Fomin DA (2003) Cerebrospinal fluid analysis. Am Fam Physician 68:1103–1108
Acknowledgments
This study has been approved by the Medical Ethics Committee of the University Hospital Center Utrecht, The Netherlands. The study has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki. The Medical Ethics Committee of the University Hospital Center decided that patients did not have to be informed personally because only data of the patient (anonymous) were used.
Conflict of interest
The authors declare that they have no conflict of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Horstman, P., Linn, F.H.H., Voorbij, H.A.M. et al. Chance of aneurysm in patients suspected of SAH who have a ‘negative’ CT scan but a ‘positive’ lumbar puncture. J Neurol 259, 649–652 (2012). https://doi.org/10.1007/s00415-011-6228-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-011-6228-1