Abstract
The objective of this study is to evaluate the clinical and radiological characteristics and the outcome of status epilepticus (SE). 117 consecutive patients with SE were evaluated including their demographics, history of epilepsy, antiepileptic drug (AED) default, comorbidities, SE type and duration. The study included 22 children, 77 adults and 18 elderly patients with SE. Blood counts, serum chemistry, ECG, cranial MRI, cerebrospinal fluid and EEG were done. Patients were treated with IV phenytoin, valproate, lorazepam or diazepam as per a fixed protocol and responses to first and second drugs were noted. Death during hospital was recorded. The etiology of SE was infection in 53.8%, drug default in 7.9%, metabolic in 14.5%, stroke in 12.8% and miscellaneous in 11% of patients. 92.3% of patients had convulsive and 7.7% nonconvulsive SE. Cranial MRI was abnormal in 62%. Infection as an etiology was more common in children, drug default and metabolic causes in adults and stroke in adults and elderly. Following first AED, SE was controlled in 50%. 30% of patients remained refractory to second AED which was related to duration of SE and mortality. 29% patients died and death was higher in elderly (44%) compared to children (14%). Acute symptomatic SE is more common in developing countries. Refractory SE is associated with SE duration and mortality.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Status epilepticus (SE) is a common and serious neurological emergency; its mortality rate has declined from 50% in earlier studies to 20–39% in recent studies [2, 10, 11, 23, 37]. The epidemiology of SE differs widely in different geographical regions. In the developing countries, infections, infestations and birth and head injuries, as well as seizure, are important causes of SE. In a review of the etiology of SE, the important causes of SE were idiopathic, remote symptomatic, acute symptomatic and progressive encephalopathies [9]. In a study from Ethiopia, the important causes of SE were CNS infection (36%), drug default (17%) and idiopathic causes (16.8%) [2]. In developed countries stroke (16.7–60%) is an important cause of SE in adults [3, 17]. The etiology of SE may also differ between adults and children. In adults the important causes of SE are stroke, antiepileptic drug withdrawal, alcohol withdrawal, anoxia and metabolic disorders; infection as an etiology is more common in children. In our earlier studies, we have reported SE in CNS infections and encephalitis highlighting the response to AED and outcome [16, 23]. The socioeconomic transition of India may be reflected in the etiology and outcome of SE. In the present study we report the clinical characteristics, MRI changes, response to treatment and outcome in consecutive patients with SE in different age groups.
Subjects and methods
Consecutive patients with SE admitted in neurology or other wards of the institute or attending the emergency ward during 2002–2007 were prospectively evaluated. Patients 12 years or below were grouped as children and 60 years or above as elderly. Status epilepticus was defined as occurrence of two or more convulsive seizures without full recovery of consciousness between the seizures or continuous convulsive activity lasting for more than 10 min. Nonconvulsive SE was defined when the patient had coma with ictal discharges on EEG with or without subtle convulsive movements, e.g., rhythmic twitching of arms, trunk, leg or facial muscles, tonic eye movement or nystagmoid jerks [36]. Alcohol withdrawal SE was defined as SE precipitated by documented alcohol withdrawal. Systemic infection was defined as presence of infection without evidence of central nervous system or meningeal infection. History of seizures in the past was noted. Decrease in antiepileptic drug as a precipitant of SE in patients with pre-existing epilepsy was defined as documented cessation of antiepileptic drug. Congenital causes were defined as preexisting central nervous system or vascular malformation. Anoxia, cerebral hemorrhage, ischemic stroke, tumor, metabolic conditions, head trauma, drug induced and central nervous system infections were defined as precipitating causes of SE using standard clinical definitions. Idiopathic SE was defined when there was no identifiable cause [7].
Type of SE was categorized into generalized convulsive, secondary generalized or nonconvulsive SE. The duration of SE prior to treatment was noted. Consciousness was assessed by Glasgow Coma scale (GCS) after control of seizures. Presence of cranial nerve palsy, fundus abnormality and focal weakness were noted. Muscle tone and tendon reflexes were graded as increased, decreased or normal.
Investigations
Blood counts, hemoglobin, ESR and peripheral blood smear for malaria were carried out. Blood sugar and serum creatinine, bilirubin, transaminase, sodium, potassium, calcium, magnesium and albumin were estimated. Radiograph of chest and electrocardiogram (ECG) were also carried out. In patients with suspected infection, blood and urine culture and sensitivity for bacteria were carried out. Cranial MRI was done using a 1.5T (Signa GE Medical Systems, Wisconsin, USA) scanner. T1, T2 and FLAIR (fluid attenuated inversion recovery) images were obtained. Electroencephalography (EEG) was carried out using 21 channel EEG equipment. The EEG was carried out within 1 h of control of convulsive SE. 30 min recording was obtained using the 10–20 system of electrode placement in a number of horizontal and vertical montages. Presence of epileptiform discharges, asymmetry and slowing were noted. In patients with suspected central nervous infection, cerebrospinal fluid was examined for cell, protein, sugar and bacteria as well as fungal culture. CSF was also analyzed for herpes simplex, Japanese encephalitis and dengue virus infection using polymerase chain reaction and IgM capture ELISA.
Treatment
The patients were treated with IV phenytoin sodium 20 mg/kg or sodium valproate 30 mg/kg as per a fixed protocol used for a randomized controlled trial which was duly approved by our institute ethics committee [24]. The drugs were crossed over in the patients who were resistant to the first antiepileptic drug. Patients not responding to the second antiepileptic drug were administered intravenous lorazepam (0.1 mg/kg), midazolam (0.1 mg/kg) or diazepam (0.15 mg/kg). The response to the treatment was defined on the basis of clinical cessation of convulsion in GCSE. In NCSE, regaining alertness and EEG evidence were taken as responses to AED. In GCSE, EEG was also performed within 1 h of clinical cessation of convulsions, however the patient was not treated as SE on the basis of EEG alone. Occurrence of hypotension, arrhythmia, respiratory dysfunction and other complications were noted. The patients not responding even to a third antiepileptic drug were given oral carbamazepine, gabapentin, clobazam, acetazolamide and levetiracetam in various combinations. In uncontrolled convulsive SE, if there was respiratory compromise, the patient was put on a mechanical ventilator. All patients were managed in the general ward with central oxygen and suction as well as mechanical ventilation facilities. If SE was not controlled with two AEDs, it was considered to be refractory [13]. Recurrence of seizure within 24 h in patients who responded to initial antiepileptic drugs was noted. Patients also received treatment for underlying diseases such as acyclovir for herpes simplex encephalitis, antibiotics for septicemia and dialysis in chronic renal failure. Hospital mortality was recorded and categorized as mortality related to SE or to other causes.
Statistical analysis
Relationship of various clinical, etiological, and MRI findings and response to antiepileptic drugs with outcomes (death or survival) were evaluated employing Chi-square, Fisher’s exact test and independent t test using SPSS version 12 software. Clinical characteristics, MRI findings and outcomes were compared among different age groups using one way ANOVA. Multiple comparisons were done for significant variables.
Results
Demography
The study included 117 patients with SE of whom 22 were children (≤12 years), 77 adults and 18 elderly (>60 years). The median age of the patients was 33 (range 1–78) years. Status epilepticus was most frequent in the third decade, occurring in 17% of patients (Fig. 1). The majority of our patients were Hindus (105).
Etiology
The etiology of SE was infection (CNS 57 and systemic 6) in 63 (53.8%) patients, stroke in 15 (12.8%), metabolic causes in 17 (14.5%), antiepileptic drug default in 9 (7.9%) and miscellaneous causes in 13 (11.1%). The CNS infection group included meningitis in 14 (tubercular 10, fungal 1, pyogenic 3) patients, encephalitis in 35 (herpes 4, Japanese 9, dengue 1, nonspecific 21), neurocysticercosis in 4, tuberculoma in 2 and cerebral malaria in 1 patient. Seven patients had only systemic infections. In the stroke group, eight had ischemic stroke, five intracerebral hemorrhage and two cerebral venous sinus thrombosis. In the metabolic group, the causes included liver failure in 2, renal failure in 11, hyponatremia in 1 and hyperglycemia in 3 patients. The miscellaneous group was comprised of post cardiac arrest (1), acute disseminated encephalomyelitis (2), progressive multifocal leucoencephalopathy (1), idiopathic origin (1), pituitary tumor (1), hypertensive encephalopathy (1), idiopathic thrombocytopenic purpura (1), post head injury (1), mitochondrial encephalopathy (1), encephalitis sequelae (1) and Creutzfeldt-Jakob disease (1). Infection dominated the etiology of SE in both adults (57.6%) and children (66.7%) whereas stroke was more frequent in the elderly (44.4%). Drug default and metabolic abnormalities were more frequent causes of SE in adults compared to children. Stroke was higher in elderly (44.4%) compared to adults (9%). The various etiologies of SE in children, adults and elderly are summarized in Table 1.
Types of status epilepticus
In the present study, convulsive SE was the most common type of SE, occurring in 108 (92.3%) patients; only 9 (7.7%) had nonconvulsive status epilepticus. Todd’s paralysis was present in 25 patients in the form of hemiplegia in all cases where it occurred. The median duration of SE was 10 h (range 0.25–610). The duration of SE was longer in children (99.84 ± 180.37 h) compared to adults (21.37 ± 47.05 h) and elderly (20.65 ± 22.07 h).
Radiological findings
Cranial imaging was done in 105 patients, MRI in 44, CT scan in 44 and both in 17 patients. Imaging was abnormal in 65 (61.9%) patients. The abnormalities were cortical in location in 15, subcortical in 20 and both cortical and subcortical in 30 patients. The distribution of radiological abnormality between children, adults and elderly is summarized in Table 2.
Electroencephalography (EEG)
Electroencephalography within 1 h of cessation of convulsion was carried out in 90 patients and was abnormal in 84. Epileptiform discharges were present in 26 (28.9%) patients, periodic lateralized epileptiform discharges in 6 (6.7%) and slowing in 46 (51%). All patients with nonconvulsive SE were diagnosed on the basis of epileptiform discharges on EEG. None of the children had normal EEG; however, the pattern of EEG was not significantly different between the groups (Table 2).
Response to treatment
65 patients received sodium valproate and 52 received phenytoin as a first line antiepileptic drug as per a fixed protocol, which resulted in control of SE in 59 (50.4, 56% with valproate and 44% with phenytoin). Crossing over of the treatment protocol to uncontrolled patients resulted in remission in 41 additional patients, and 35 (30%) remained refractory to 2 antiepileptic drugs. In the remaining uncontrolled patients, intravenous lorazepam (4), diazepam (7), midazolam (3) or intramuscular paraldehyde (2) were given, following which eight additional patients had remission. Within 24 h, discrete seizures recurred in six patients whose SE initially responded to the first or second AED. SE was well controlled following the first antiepileptic drug in children (66.7%) compared to adults (51.3%) and elderly (27.8%; P = 0.05).
Response to the first antiepileptic drug and refractoriness of SE were not related to etiology (Table 3). The duration of SE in the patients who were controlled following the first antiepileptic drug was shorter (19.49 ± 35.73 h) compared to those who were not controlled (50.17 ± 120.7 h). This difference, however, was not statistically significant (Z = − 1.5, P = 0.13). Refractoriness of SE, however, was related to duration of SE (Z = 2.1, P = 0.04). The duration of status epilepticus in the refractory group was 59.18 ± 111.06 h and that in the nonrefractory group it was 25.80 ± 75.35 h. Control of SE was not related to cranial imaging abnormality; 31 of 65 patients with abnormal imaging were controlled by the first antiepileptic drug and 22 out of 40 without imaging abnormality were also controlled by the first drug.
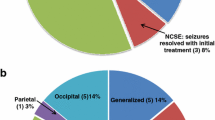
Mortality
In our study, 34 (29%) patients died in hospital; death was higher in elderly (44.4%) compared to adults (29.5%) and children (14%). Death in the elderly was significantly higher compared to children (P = 0.03). Death was due to status epilepticus per se in eight, while the remaining patients died due to underlying diseases. Out of 9 patients with nonconvulsive SE, 2 died, and the remaining 32 deaths were in the convulsive group. Death was highest in the infection (33.3%) and metabolic (35.3%) groups. The details regarding death as per etiology are shown in Fig. 2. Death was related to refractoriness of SE (P = 0.008); 50% patients with refractory SE died compared to 23.4% in the nonrefractory group. Duration of SE was not related to mortality (Z = − 1.06, P = 0.29).
Discussion
In the present study, infection triggering factor of SE in both adults and children, while stroke was most important in the elderly. Children responded better to treatment. Duration of status epilepticus was associated with refractoriness, which was related to high mortality. In an analysis of eight studies in SE, the causes in children were idiopathic in 24–39%, remote symptomatic in 10–23%, febrile in 20–28%, acute symptomatic in 24–50% and progressive encephalopathy in 2–6%. In contrast, the causes of SE in adults were idiopathic in 24–38%, remote symptomatic in 3–17%, febrile in 0–3% and acute symptomatic in 40–57% [1, 3, 5, 10, 21, 29, 31, 33]. In our study, acute symptomatic SE was the cause of status in all except 22 patients. In the acute symptomatic group, infection constituted 53.8% of cases. In a study from South India, the etiology of SE was acute symptomatic in 54%, remote symptomatic in 7%, cryptogenic in 19%, and earlier epilepsy in 19%. CNS infection was found in 28% of patients [27]. Another study from China reported history of epilepsy in 50%, CNS infection in 32.7% and discontinuation or reduction of antiepileptic drugs in 15.5% of patients with convulsive SE [4]. The high prevalence of acute symptomatic epilepsy in our study may be due to referral bias; as our facility is a tertiary care super specialty public hospital, complicated cases with infection and organ failure are referred to us. Moreover, our institute, being a public hospital, caters mostly middle and low class socioeconomic strata. Neurocysticercosis is the commonest cause of focal epilepsy in developing countries [8, 26, 28] and tuberculous meningitis and encephalitis are prevalent in South East Asia [15, 25]. Central nervous system infection has also been reported as a major cause of SE from Ethiopia (36%) and Senegal (67%) [2, 22]. Stroke as a cause of SE has been reported in 16.7–60%, metabolic causes in 8.7–28%, CNS tumor in 5–16%, drug default in 10.4–22.5% and idiopathic in 3–18% in various studies [3, 14, 17, 32, 34]. High prevalence of stroke in India, especially in the young, may also contribute to the burden of seizures and SE. In our study 14.5% of patients had SE due to metabolic causes. This may reflect the referral bias as our institute is active in the organ transplantation programme. These may account for differences between the etiologies of SE in our study and those reported from Western countries [12, 35].
In an earlier large study, the peak incidence of status epilepticus was in the sixth and seventh decades [6]. In our study, the highest incidence of SE was in third and closely followed by sixth decade. 83.8% of patients were below the age of 61 years. In the study from Ethiopia, also, 90% of patients were below the age of 60 years [2]. The patients in the third decade may be due to the high frequency of infection in the present cohort and the lesser number of children and elderly. Children in our study responded to the first antiepileptic drug better than adults. Response to antiepileptic drugs is the best predictor of mortality in SE. In the reported literature the mortality of SE ranged between 11 and 29.7% [2, 4, 22, 23, 27, 32]. The mortality in our patients was 29%, which was insignificantly higher in the elderly compared to children. Lower mortality in children compared to the elderly has been reported in a large retrospective analysis in which 2.3% children and 25% adults died [6]. In a Chinese study, 15.8% of SE patients died within 30 days of hospitalization, and duration of SE, mechanical ventilation and complications after admission were independent predictors of death [18].
In our study, the median duration of status epilepticus was 10 (0.25–610) h. This is related to poor medical infrastructure facilities and the nature of tertiary care hospital based studies. Duration of status has been reported to be associated with control of status and mortality in a number of studies [6, 13, 19]. In our study, however, duration of SE was not related to mortality or seizure control but was related to refractoriness of status. In earlier studies, refractoriness of status was related to extreme of age, duration of SE, acute symptomatic and nonconvulsive status [13, 20, 36]. Mortality of SE is reported to be high in cases of acute symptomatic status [17, 30]. The higher mortality in our study may be due to prolonged duration of status, high frequency of acute symptomatic epilepsy and lack of an intensive care facility. Moreover, we have used valproate and phenytoin as first line antiepileptic drugs instead of lorazepam or diazepam, which are recommended as first line AEDs in the management of SE. This may also account for the higher frequency of refractory SE in our study. However, in a study comparing lorazepam, phenytoin, diazepam and phenobarbitone in SE, there was no significant difference in the number needed to treat, SE control, recurrence of seizure and 30 days outcome [36]. We have not done blood levels of AEDs, as the results are not available immediately to modify the dose.
Our results are applicable to the patients of the developing world and are quite different from Western countries, highlighting the importance of acute symptomatic SE and need for early treatment.
References
Aicardi J, Chevrie JJ (1970) Convulsive status epilepticus in infants and children. A study of 239 cases. Epilepsia 11:187–197
Amare A, Zenebe G, Hammack J, Davey G (2008) Status epilepticus: clinical presentation, cause, outcome and predictors of death in 119 Ethiopian patients. Epilepsia 49:600–607
Aminoff MJ, Simon RP (1989) Status epilepticus: causes, clinical features and consequences in 98 patients. Am J Med 69:657–666
Chen L, Zhou B, Li JM, Zhu Y, Wang JH, Sander JW, Stefan H, Zhou D (2009) Clinical features of convulsive status epilepticus: a study of 220 cases in western China. Eur J Neurol 16:444–449
(1993) Commission on epidemiology and prognosis of the international league against epilepsy. Epilepsia 34:592–596
DeLorenzo RJ, Towne AR, Pellock JM, Ko D (1992) Status epilepticus in children, adults, and the elderly. Epilepsia 33:S15–S25
Engel JE, Jr (ed) (1989) Causes of Human epilepsy. In: Seizures and epilepsy. F.A. Davis, Philadephia, 112–134
Garcia HH, Del Brutto OH (2005) Neurocysticercosis: updated concepts about an old disease. Lancet Neurol 4:653–661
Gross-Tsur V, Shinnar S (1993) Convulsive status epilepticus in children. Epilepsia 34:S12–S20
Hauser WA (1983) Status epilepticus: frequency, etiology, and neurological sequelae. Adv Neurol 34:3–14
Hauser WA (1990) Status epilepticus: epidemiologic considerations. Neurology 40(5 Suppl 2):9–13
Hesdorffer DC, Logroscino G, Cascino G, Annegers JF, Hauser WA (1998) Incidence of status epilepticus in Rochester, Minnesota, 1965–1984. Neurology 50:735–741
Holtkamp M, Othman J, Buchheim K, Meierkord H (2005) Predictors and prognosis of refractory status epilepticus treated in a neurological intensive care unit. J Neurol Neurosurg Psychiatry 76:534–539
Hui A, Joyn GM, Li H, Wong KS (2003) Status epilepticus in Hong Kong Chinese: etiology, outcome and predictors of death and morbidity. Seizure 12:478–482
Kalita J, Misra UK, Pandey S, Dhole TN (2003) A comparison of clinical and radiological findings in adults and children with Japanese encephalitis. Arch Neurol 60:1760–1764
Kalita J, Nair PP, Misra UK (2008) Status epilepticus in encephalitis: a study of clinical findings, magnetic resonance imaging, and response to antiepileptic drugs. J Neurovirol 14:412–417
Knake S, Rosenow F, Vescovi M, Oertel WH, Mueller HH, Wirbatz A, Katsarou N, Hamer HM (2001) Status Epilepticus Study Group Hessen (SESGH) incidence of status epilepticus in adults in Germany: a prospective, population-based study. Epilepsia 42:714–718
Li JM, Chen L, Zhou B, Zhu Y, Zhou D (2009) Convulsive status epilepticus in adults and adolescents of southwest China: mortality, etiology, and predictors of death. Epilepsy Behav 14:146–149
Maegaki Y, Kurozawa Y, Hanaki K, Ohno K (2005) Risk factors for fatality and neurological sequelae after status epilepticus in children. Neuropediatrics 36:186–192
Mayer SA, Claassen J, Lokin J, Mendelsohn F, Dennis LJ, Fitzsimmons BF (2002) Refractory status epilepticus: frequency, risk factors, and impact on outcome. Arch Neurol 59:205–210
Maytal J, Shinnar S, Moshé SL, Alvarez LA (1989) Low morbidity and mortality of status epilepticus in children. Pediatrics 83:323–331
Mbodj I, Ndiaye M, Sene F, Salif Sow P, Sow HD, Diagana M, Pierre Ndiaye I, Gallo Diop A (2000) Treatment of status epilepticus in the context of a developing country. Neurophysiol Clin 30:165–169
Misra UK, Kalita J, Nair PP (2008) Status epilepticus in central nervous system infections: an experience from a developing country. Am J Med 121:618–623
Misra UK, Kalita J, Patel R (2006) Sodium valproate vs phenytoin in status epilepticus: a pilot study. Neurology 67:340–342
Misra UK, Kalita J, Roy AK, Mandal SK, Srivastava M (2000) Role of clinical, radiological, and neurophysiological changes in predicting the outcome of tuberculous meningitis: a multivariable analysis. J Neurol Neurosurg Psychiatry 68:300–303
Murthy JM (2002) Seizures due to solitary cysticercus granuloma. In: Singh G, Prabhakar S (eds) Taenia solium cysticercoids: from basic to clinical science. CABI Publishing, Oxon, pp 251–256
Murthy JM, Jayalaxmi SS, Kanikannan MA (2007) Convulsive status epilepticus: clinical profile in a developing country. Epilepsia 48:2217–2223
Murthy JM, Yangala R (1999) Acute symptomatic seizures—incidence and etiological spectrum: a hospital-based study from South India. Seizure 8:162–165
Oxbury JM, Whitty CW (1971) Causes and consequences of status epilepticus in adults. A study of 86 cases. Brain 94:733–744
Parent JM, Lowenstein DH (1994) Treatment of refractory generalized status epilepticus with continuous infusion of midazolam. Neurology 44:1837–1840
Roberts MR, Eng-Bourquin J (1995) Status epilepticus in children. Emerg Med Clin North Am 13:489–507
Rossetti AO, Hurwitz S, Logroscino G, Bromfield EB (2006) Prognosis of status epilepticus: role of aetiology, age, and consciousness impairment at presentation. J Neurol Neurosurg Psychiatry 77:611–615
Rowan AJ, Scott DF (1970) Major status epilepticus. A series of 42 patients. Acta Neurol Scand 46:573–584
Towne AR (2007) Epidemiology and outcomes of status epilepticus in the elderly. Int Rev Neurobiol 81:111–127
Towne AR, Pellock JM, Ko D, DeLoreanzo RJ (1994) Determinant of mortality in status epilepticus. Epilepsia 35:27–34
Treiman DM, Meyers PD, Walton NY, Collins JF, Colling C, Rowan AJ, Handforth A, Faught E, Calabrese VP, Uthman BM, Ramsay RE, Mamdani MB (1998) A comparison of four treatments for generalized convulsive status epilepticus. Veterans Affairs Status Epilepticus Cooperative Study Group. N Engl J Med 339:792–798
Vignatelle L, Rinaldi R, Galeotti M, deCardes P, D’ Alessandro R (2005) Epidemiology of status epilepticus in a rural area of northern Italy: a 2 year population based study. Eur J Neurol 12:897–902
Acknowledgments
We thank Rakesh Kumar Nigam and KS Bist for technical support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kalita, J., Nair, P.P. & Misra, U.K. A clinical, radiological and outcome study of status epilepticus from India. J Neurol 257, 224–229 (2010). https://doi.org/10.1007/s00415-009-5298-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-009-5298-9