Abstract
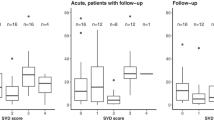
The purpose was to examine the occurrence of sleep-related breathing disorders (SRBD) and variables related to SRBD in patients with acute lacunar stroke. In 68 consecutive patients with radiologically proven lacunes, respiratory polygraphy within the first 48 h of stroke onset was performed. SRBDs were classified according to mutually exclusive cutoff values of the apnea/hypopnea index (AHI) as mild (AHI ≥10), moderate (AHI ≥20), and severe (AHI ≥30). Variables independently associated with SRBDs were assessed by logistic regression analysis. The mean (standard deviation) AHI was 21.9 (17.4). A total of 69.1% of patients showed AHI ≥10, 44.1% AHI ≥20, and 25% AHI ≥30. Cheyne-Stokes respiration (CSR) was present in 20.6% of patients. Smoking (>20 cigarettes/day) or location of lacunes in the internal capsule or the pons was significantly more frequent in the AHI ≥10 group than in the remaining AHI groups (80.9% vs. 57.1%, P = 0.041). AHI ≥20 and AHI ≥30 occurred more frequently in smokers or in capsular or pontine lacunes than in the remaining patients (20% vs. 2.6%, P = 0.053; 29.4% vs. 3.9%, P = 0.01, respectively). In the multivariate analysis, smoking or capsular or pontine topographies were associated with AHI ≥10 [odds ratio (OR) = 3.17, 95% confidence interval (CI) 1.02–9.79; P = 0.045]. Lacunes in the internal capsule or the pons in smokers were associated with AHI ≥20 (OR = 9.25, 95% CI 1.05–81.70; P = 0.045). Smoking (OR = 19.64, 95% CI 1.68–229.85; P = 0.010) and body mass index (OR = 1.68, 95% CI 1.13–2.50; P = 0.010) were associated with AHI ≥30. Smoker patients with capsular or pontine acute lacunar stroke should be screened for SRDB.
Similar content being viewed by others
References
Arboix A, Morcillo C, García-Eroles L, Oliveres M, Massons J, Targa C (2000) Different vascular risk factor profiles in ischemic stroke subtypes: a study from the “Sagrat Cor Hospital of Barcelona Stroke Registry”. Acta Neurol Scand 102:264–270
Arzt M, Young T, Finn L, Skatrud JB, Douglas Bradley T (2005) Association of sleep-disordered breathing and occurrence of stroke. Am J Respir Crit Care Med 172:1447–1451
Askenasy JM, Goldhamer I (1998) Sleep apnea as a feature of bulbar stroke. Stroke 19:637–639
Basile AM, Pantoni L, Pracucci G, Asplund K, Chabriat H, Erkinjuntti T, Fazekas F, Ferro JM, Hennerici M, O’Brien J, Scheltens P, Visser MC, Wahlund LO, Waldemar G, Wallin A, Inzitari D (2006) Age, hypertension, and lacunar stroke are the major determinants of the severity of age-related white matter changes. The LADIS (Leukoaraiosis and Disability in the Elderly Study). Cerebrovasc Dis 21:315–322
Bassetti C, Aldrich MS (1999) Sleep apnea in acute cerebrovascular disease: final report in 128 patients. Sleep 22:217–223
Bassetti CL, Milanova M, Gugger M (2006) Sleep-disordered breathing and acute ischemic stroke: diagnosis, risk factors, treatment, evolution, and long-term clinical outcome. Stroke 37:967–972
Chaudhary BA, Elguindi AS, King DW (1982) Obstructive sleep apnea after lateral medullary syndrome. South Med J 75:65–67
Cherniack NS, Longobardo G, Evangelista CJ (2005) Causes of Cheyne-Stokes respiration. Neurocrit Care 3:271–279
Durán J, Esnaola S, Rubio R, Iztueta A (2001) Obstructive sleep apnea-hypopnea and related clinical features in a population-based sample of subjects aged 30 to 70 yr. Am J Respir Crit Care Med 163:685–689
Dyken ME, Somers VK, Yamada T, Ren ZY, Zimmerman MB (1996) Investigating the relationship between stroke and obstructive sleep apnea. Stroke 27:401–407
Gandolfo C, Caponnetto C, Del Sette M, Santoloci D, Loeb C (1988) Risk factors in lacunar síndromes: a case-control study. Acta Neurol Scand 77:22–26
Harbison J, Gibson GJ, Birchall D, Zammit-Maempel I, Ford GA (2003) White matter disease and sleep-disordered breathing after acute stroke. Neurology 61:959–963
Harbison JA, James OFW, Gibson GJ, Ford GA (2000) Sleep apnea following stroke. Cerebrovasc Dis 10(Suppl 2):7
Hermann DM, Siccoli M, Kirov P, Gugger M, Bassetti CL (2007) Central periodic breathing during sleep in acute ischemic stroke. Stroke 38:1082–1084
Hudgel DW, Deradtta P, Hamilton H (1993) Pattern of breathing and upper airway mechanics during wakefulness and sleep in healthy elderly humans. J Appl Physiol 74:2198–2204
Hui D, Choy D, Wong L, Ko F, Li T, Woo J, Kay R (2002) Prevalence of sleep-disordered breathing and continuous positive airway pressure compliance. Chest 122:852–860
Jackson C, Sudlow C (2005) Are lacunar strokes really different? A systematic review of differences in risk factor profiles between lacunar and nonlacunar infarcts. Stroke 36:891–904
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth Sleepiness Scale. Sleep 14:540–545
Kapen S, Park A, Goldberg J, Whynter J (1991) The incidence and severity of obstructive sleep apnea in ischaemic cerebrovascular disease. Neurology 41(Suppl 1):125
Kokturk O, Ciftci TU, Mollarecep E, Ciftci B (2006) Serum homocysteine levels and cardiovascular morbidity in obstructive sleep apnea syndrome. Respir Med 100:536–541
Laloux P, Jamart J, Meurisse H, De Coster P, Laterre C (1996) Persisting perfusion deficit in transient ischaemic attacks: a new clinical useful group? Stroke 27:425–430
Lavie L, Lavie P (2008) Smoking interacts with sleep apnea to increase cardiovascular risk. Sleep Med 9:247–253
Lie C, Hirsch JG, Roßmanith C, Hennerici MG, Gass A (2004) Clinicotopographical correlation of corticospinal tract stroke: a color-coded diffusion tensor imaging study. Stroke 35:86–93
Liepert J, Restemeyer C, Kucinski T, Zittel S, Weiller C (2005) Motor strokes: the lesion location determines motor excitability changes. Stroke 36:2648–2653
Lodder J, Bamford JM, Sandercock PAG, Jones LN, Warlow CP (1990) Are hypertension or cardiac embolism likely causes of lacunar infarction? Stroke 21:375–381
Marín JM, Carrizo S, Vicente E, Agustí AG (2005) Long-term cardiovascular outcomes in men with obstructive sleep apnea-hypoapnea with or without treatment with continuous positive airway pressure: an observational study. Lancet 172:1447–1451
Martí-Vilalta JL, Arboix A, Mohr JP (2004) Lacunes. In: Mohr JP, Choi DW, Grotta JC, Weir B, Wolf PhA (eds) Stroke. Pathophysiology, diagnosis, and management. Churchill Livingstone, Philadelphia, pp 275–299
Martinez-Garcia MA, Galiano-Blancart R, Soler-Cataluna JJ, Cabero-Salt L, Roman-Sanchez P (2006) Improvement in nocturnal disordered breathing after first-ever ischemic stroke: role of dysphagia. Chest 129:238–245
Muñoz R, Duran-Cantolla J, Martinez-Vila E, Gallego J, Rubio R, Aizpuru F, De La Torre G (2006) Severe sleep apnea and risk of ischemic stroke in the elderly. Stroke 37:2317–2321
Nachtmann A, Siebler M, Rose G, Sitzer M, Teimetz H (1995) Cheyne-Stokes respiration in ischemic stroke. Neurology 45:820–821
Netzer N, Werner P, Jochums I, Lehmann M, Strohl K (1998) Blood flow of the middle cerebral artery with sleep-disordered breathing. Stroke 29:87–93
Nopmaneejumruslers C, Kaneko Y, Hajek V, Zivanovic V, Bradley TD (2005) Cheyne-Stokes respiration in stroke: relationship to hypocapnia and occult cardiac dysfunction. Am J Respir Crit Care Med 171:1048–1052
Norrving B, Staaf G (1991) Pure motor stroke from presumed lacunar infarct. Incidence, risk factors and initial course. Cerebrovasc Dis 1:203–209
Parra O (2004) Trastornos respiratorios del sueño y enfermedad vascular cerebral. Arch Bronconeumol 40:34–38
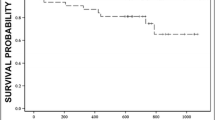
Parra O, Arboix A, Bechich S, Garcia-Eroles Monserrat JM, López JA, Ballester E, Guerra JM, Sopeña JJ (2000) Time course of sleep-related breathing disorders in first-ever stroke or transient ischemic attack. Am J Respir Crit Care Med 161:375–380
Parra O, Arboix A, Montserrat JM, Quinto L, Bechich S, Garcia-Eroles L (2004) Sleep-related breathing disorders: impact on mortality of cerebrovascular disease. Eur Respir J 24:267–272
Rowat AM, Dennis MS, Wardlaw JM (2006) Central periodic breathing observed on hospital admission is associated with an adverse prognosis in conscious acute stroke patients. Cerebrovasc Dis 21:340–347
Rowat AM, Wardlow JM, Dennis MS (2007) Abnormal breathing patterns in stroke—relationship to acute stroke lesion location and prior cerebrovascular disease. J Neurol Neurosurg Psychiatry 78:277–279
Sahlin C, Sandberg O, Gustafson Y, Bucht G, Carlberg B, Stenlund H, Franklin KA (2008) Obstructive sleep apnea is a risk factor for death in patients with stroke: a 10-year follow-up. Arch Int Med 168:297–301
Shahar E, Whitney CW, Redline S, Lee ET, Newman AB, Javier Nieto F, O’Connor GT, Boland LL, Schwartz JE, Samet JM (2001) Sleep-disordered breathing and cardiovascular disease. Cross-sectional results of the Sleep Heart Health Study. Am J Respir Crit Care Med 163:19–25
Sommers VK, White DP, Amin R, Abraham WT, Costa F, Culebras A, Daniels S, Floras JS, Hunt CE, Olson LJ, Pickering TG, Russell R, Woo M, Young T (2008) Sleep apnea and cardiovascular disease. Circulation 118:1080–1111
Underner M, Paquereau J, Meurice JC (2006) Tabagisme et troubles du sommeil. Rev Mal Respir 23:6S67–6S77
Van Swieten JC, Koudstaal PJ, Visser MC, Schoute HJA, van Gijn J (1988) Interobserver agreement for the assessment of handicap in stroke patients. Stroke 19:604–607
Yaggi H, Mohsenin V (2004) Obstructive sleep apnoea and stroke. Lancet Neurol 3:333–342
Wessendorf TE, Teschler H, Wang YM, Konietzko N, Thilmann AF (2000) Sleep disordered breathing among patients with first-ever stroke. J Neurol 247:41–47
Wessendorf TE, Thilmann AF, Wang YM, Schreiber A, Konietzko N, Teschler H (2000) Fibrinogen levels and obstructive sleep apnea in ischaemic stroke. Am J Respir Crit Care Med 162:2039–2042
Yaggi H, Mohsenin V (2003) Sleep-disordered breathing and stroke. Clin Chest Med 24:223–237
Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V (2005) Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med 353:2034–2041
You R, McNeil JJ, O’Malley HM, Davis SM, Donnan JA (1995) Risk factors for lacunar infarction syndromes. Neurology 45:1483–1487
Acknowledgments
The authors thank Marta Pulido, MD, for editing the manuscript and for editorial assistance. The first-author credit should be equally distributed among M. Bonnin-Vilaplana, A. Arboix, and O. Parra. This study was supported by a grant from FIS PI081514.
Conflicts of interest statement
None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bonnin-Vilaplana, M., Arboix, A., Parra, O. et al. Sleep-related breathing disorders in acute lacunar stroke. J Neurol 256, 2036–2042 (2009). https://doi.org/10.1007/s00415-009-5236-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-009-5236-x