Abstract
Dysphagia is an important yet inconsistently recognized symptom of inclusion body myositis (IBM). It can be disabling and potentially life-threatening. We studied the prevalence and symptom-sign correlation of dysphagia. Fifty-seven IBM patients were interviewed using a standard questionnaire for dysphagia and 43 of these underwent swallowing videofluoroscopy (VFS). Symptoms of dysphagia were present in 37 of 57 patients (65%). Nevertheless, only 17 of these patients (46%) had previously and spontaneously complained about swallowing to their physicians. Both symptoms of impaired propulsion (IP) (59%) and aspiration-related symptoms (52%) were frequently mentioned. Swallowing abnormalities on VFS were present in 34 of 43 patients (79%) with IP of the bolus in 77% of this group. The reported feeling of IP was confirmed by VFS in 92% of these patients. Dysphagia in IBM is common but underreported by the vast majority of patients if not specifically asked for. In practice, two questions reliably predict the presence of IP on VFS: ‘Does food get stuck in your throat’ and ‘Do you have to swallow repeatedly in order to get rid of food’. These questions are an appropriate means in selecting IBM patients for further investigation through VFS and eventual treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Dysphagia is one of the main clinical features of inclusion body myositis (IBM) [3, 9–11, 15]. Together with weakness of quadriceps and finger flexor muscles, dysphagia constitutes a clue for the diagnosis. It may even be the presenting symptom [3, 13, 14, 20]. Dysphagia causes both social embarrassment and life threatening complications. It may lead to avoidance of shared meals and social isolation due to audible deglutition. Besides, it can lead to unintended weight loss. Due to a higher incidence of aspiration pneumonia, life expectancy is assumed to be shorter [12]. Therapeutical interventions described to be effective for dysphagia in IBM patients include cricopharyngeal myotomy, pharyngoesophageal dilatation and swallowing exercises such as the Mendelsohn maneuver [12].
We investigated the prevalence and symptom-sign correlation of swallowing dysfunction in a large group of IBM patients. Through this approach we aimed at finding specific questions which could reliably predict dysphagia in the IBM patient in order to influence the selection of patients who need further investigation through videofluoroscopy (VFS) or who need therapeutical interventions.
Patients and methods
Patients
The patients in this study were selected from a national cohort of 86 sporadic IBM patients. The method of recruitment applied here has been described previously [2]. Of these 86 patients, five patients could not be located, six died prior to assessment and 13 refrained from participation. Five patients were excluded because of prior cricopharyngeal myotomy. This left 57 patients to study fulfilling the ENMC criteria for definite (n = 51) or probable (n = 6) IBM [2]. To evaluate recruitment bias we compared age (at onset), sex and disease duration of these 57 patients with those of the whole cohort of 86 patients, based on their medical records. All patients gave informed consent. The study was approved by the Ethics committee of the Leiden University Medical Center. All patients answered a questionnaire and were examined by VFS, unless prevented by logistic difficulties.
Questionnaire
Patients were personally interviewed by one single investigator using a previously published standard questionnaire regarding dysphagia (Table 1) [19].
Dysphagia due to impaired propulsion (IP) was defined by the presence of at least one of the following symptoms: the feeling of food getting stuck in the throat or repetitive swallowing for one bolus. Aspiration-related (AR) dysphagia was defined by the presence of at least one of the following symptoms: choking for more than five times a month or coughing related to eating, drinking or lying down.
Videofluoroscopy
Videofluoroscopy was used to record the movements and anatomy of the pharynx and the cervical oesophagus in lateral view. Patients were seated upright with their heads in neutral position. The head was stabilized occipitally and frontally. Each patient successively swallowed four volumes of opaque fluid (Jopamiro), viz. 3, 6 and 9 ml, followed by a ‘dry swallow’ (0 ml). The VFS was scored by one single observer who was aware of the diagnosis, but uninformed with regard to the patient’s clinical features. Signs were subdivided in two categories: IP or AR.
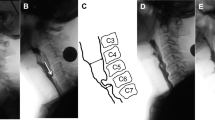
Impaired propulsion included repetitive swallowing, residue in the valleculae or piriform sinus and cricopharyngeal sphincter dysfunction. Sphincter dysfunction was defined by a posterior indentation of the sphincter, as a result of contraction of the cricopharyngeal muscle at the moment the pharynx was still dilated and filled with contrast [4].
Aspiration was defined by fluid entering the larynx. Because inadequate epiglottal downward tilting (IEDT) and residues in the valleculae and/or piriform sinus are generally regarded as risk factors for aspiration [5, 8], these three signs were also considered as AR signs. A normal swallow was concluded in the absence of IP or AR signs.
Furthermore, the presence or absence of a Zenker’s diverticulum was recorded.
Results
Demographical and clinical characteristics
The mean age of the 57 patients was 67 ± 8 years for men (n = 41) and 71 ± 10 years for women (n = 16), with a mean age at onset of muscle weakness at 57 ± 9 years for men and 59 ± 10 years for women. Most patients (n = 39, 68%) presented with weakness of the quadriceps muscles. Dysphagia was the presenting symptom in four patients (7%), at a mean age of 64 years. Mean duration of symptoms of muscle weakness was 10 ± 7 years for men and 12 ± 5 years for women. The investigated group did not differ significantly from the original population group of 86 patients with regard to age (at onset) and disease duration. The male sex however, was slightly over-represented in the investigated group compared with the group of 86 patients (male to female ratio: 2:1).
Questionnaire (n = 57)
Thirty-seven patients (65%) had symptoms of dysphagia. Women reported dysphagia more often compared to men (88 vs. 56%). Of these patients, 26 reported both IP and AR symptoms (46%), seven reported symptoms of IP only (12%) and four had exclusively AR symptoms (7%). The vast majority of these patients had symptoms on a daily basis. Solid food was the most likely to get stuck in the throat (n = 22, 71%), yet only one patient (2%) used ground food (Table 1).
Twenty patients who acknowledged dysphagia on the questionnaire (54%) had not spontaneously disclosed swallowing complaints to a physician before.
Videofluoroscopy (n = 43)
In 34 patients (79%) VFS was abnormal. Abnormal findings were equally frequent in men and women.
Thirty-three patients (77%) had signs of IP repetitive swallowing (n = 24, 56%), residues in the piriform sinus (n = 19, 44%) and valleculae (n = 16, 37%), or cricopharyngeal sphincter dysfunction (n = 16, 37%, Fig. 1).
Only one patient showed aspiration during VFS; this patient also had repetitive swallowing, vallecular and piriform sinus residues and IEDT. Twenty-three (53%) other patients had aspiration-related signs of whom 18 (43%) had IEDT. Normal swallowing function was observed in nine patients.
A Zenker’s diverticulum was found in eight patients (19%). The ostium of the diverticulum was invariably located just above the upper oesophageal sphincter.
Comparison between questionnaire and videofluoroscopy
In 25 patients who reported symptoms of IP, a VFS was performed. Of these, 23 had corresponding IP signs on VFS (positive predictive value: 0.92). The highest positive predictive values were calculated for the questions regarding food getting stuck in the throat (91%) and whether or not repeated swallows (92%) were needed. Nineteen patients (83%) showed repetitive swallowing, 15 (65%) had a piriform sinus residue, 13 (57%) had a vallecular residue and 10 (44%) demonstrated sphincter dysfunction. Remarkably, two (8%) patients had symptoms of IP, but a normal VFS. Ten out of 33 patients with IP signs on VFS had no symptoms of IP on questionnaire. The sensitivity of the questionnaire concerning IP was 0.70, the specificity 0.80 and the negative predictive value 0.44.
Twenty-three patients who underwent VFS reported AR symptoms on the questionnaire. Confirmation of aspiration on VFS was obtained in only one patient. Fourteen (65%) other patients showed one or more different AR signs on VFS (positive predictive value: 0.65). Nine out of 24 patients with AR signs on VFS had no symptoms of aspiration on the questionnaire. The sensitivity concerning AR signs was 0.63, the specificity 0.58 and the negative predictive value 0.55.
Abnormalities were more frequently detected by VFS than based on the questionnaire scores, 79 versus 65%.
Discussion
Dysphagia is a frequent, embarrassing and potentially dangerous symptom in IBM patients. Using a questionnaire, we aimed at developing a comprehensive view of the swallowing status of the patient. For analysis, we took those questions into account which we considered to be indicative of IP or aspiration and categorized them. The two categories were created to enable correlation between symptoms and signs.
We encountered dysphagia in 65% of our IBM patients after excluding patients who had undergone a cricopharyngeal myotomy. The prevalence of dysphagia in IBM differs considerably between reported studies, ranging from 40 to 80% [3, 9–11, 15]. The wide range in prevalence figures most likely originates from the absence of a universal definition for dysphagia.
In the present study, 37% of our patients had abnormal function of the cricopharyngeal sphincter. Other investigators described sphincter dysfunction in 47–69% of myositis-patients [13, 18]. Inflammatory involvement of the cricopharyngeal muscle is most likely the basis for dysfunction, as has been suggested by authors who reported the presence of inflammation or rimmed vacuoles in cricopharyngeal muscle biopsies [1, 6, 16, 18]. Due to inflammation, the compliance of the sphincter might be reduced, impeding the opening and thus the trans-sphincteric bolus flow [7]. Ageing may be another cause of a diminished sphincter opening, but ageing does not seem to prolong the pharyngeal bolus transit time, neither does it disturb trans-sphincteric bolus flow coordination [17].
Observed aspiration was rare in our patients (n = 1). However, aspiration-related signs were present in half the group. Two publications revealed higher prevalences of aspiration on VFS (24 and 61%) in inflammatory myopathies. These studies also included polymyositis and dermatomyositis patients [13, 18]. These studies, including the present study, used different fluid volumes for swallows. A different fluid consistency and volume, and a different position of the head during VFS may have influenced these prevalence figures. Differences in mechanisms of dysphagia within the inflammatory myopathies cannot be ruled out, either.
The sensitivity and specificity of questions regarding IP were disappointing. However, for the detection of dysphagia through questions from the questionnaire the positive predictive value is the most important. The positive predictive value appeared to be high enough to be of use when selecting patients to be investigated by VFS or for possible further treatment.
Despite the frequent occurrence of dysphagia in IBM only 54% of patients with dysphagia on the questionnaire had expressed swallowing difficulties to their physician spontaneously. This indicates that a proactive approach to detect dysphagia using a simple set of questions could facilitate early treatment and lead to prevention of complications.
References
Bachmann G, Streppel M, Krug B, Neuen-Jacob E (2001) Cricopharyngeal muscle hypertrophy associated with florid myositis. Dysphagia 16:244–248
Badrising UA, Maat-Schieman M, van Duinen SG, Breedveld F, van Doorn P, van Engelen B, van den HF, Hoogendijk J, Howeler C, de Jager A, Jennekens F, Koehler P, van der LH, de Visser M, Verschuuren JJ, Wintzen AR (2000) Epidemiology of inclusion body myositis in the Netherlands: a nationwide study. Neurology 55:1385–1387
Badrising UA, Maat-Schieman ML, van Houwelingen JC, van Doorn PA, van Duinen SG, van Engelen BG, Faber CG, Hoogendijk JE, de Jager AE, Koehler PJ, de Visser M, Verschuuren JJ, Wintzen AR (2005) Inclusion body myositis. Clinical features and clinical course of the disease in 64 patients. J Neurol 252:1448–1454
Berg HM, Jacobs JB, Persky MS, Cohen NL (1985) Cricopharyngeal myotomy: a review of surgical results in patients with cricopharyngeal achalasia of neurogenic origin. Laryngoscope 95:1337–1340
Buchholz DW, Bosma JF, Donner MW (1985) Adaptation, compensation, and decompensation of the pharyngeal swallow. Gastrointest Radiol 10:235–239
Danon MJ, Friedman M (1989) Inclusion body myositis associated with progressive dysphagia: treatment with cricopharyngeal myotomy. Can J Neurol Sci 16:436–438
Darrow DH, Hoffman HT, Barnes GJ, Wiley CA (1992) Management of dysphagia in inclusion body myositis. Arch Otolaryngol Head Neck Surg 118:313–317
Garon BR, Huang Z, Hommeyer M, Eckmann D, Stern GA, Ormiston C (2002) Epiglottic dysfunction: abnormal epiglottic movement patterns. Dysphagia 17:57–68
Houser SM, Calabrese LH, Strome M (1998) Dysphagia in patients with inclusion body myositis. Laryngoscope 108:1001–1005
Lindberg C, Persson LI, Bjorkander J, Oldfors A (1994) Inclusion body myositis: clinical, morphological, physiological and laboratory findings in 18 cases. Acta Neurol Scand 89:123–131
Lotz BP, Engel AG, Nishino H, Stevens JC, Litchy WJ (1989) Inclusion body myositis observations in 40 patients. Brain 112(Pt 3):727–747
Oh TH, Brumfield KA, Hoskin TL, Kasperbauer JL, Basford JR (2008) Dysphagia in inclusion body myositis: clinical features, management, and clinical outcome. Am J Phys Med Rehabil 87:883–889
Oh TH, Brumfield KA, Hoskin TL, Stolp KA, Murray JA, Bassford JR (2007) Dysphagia in inflammatory myopathy: clinical characteristics, treatment strategies, and outcome in 62 patients. Mayo Clin Proc 82:441–447
Riminton DS, Chambers ST, Parkin PJ, Pollock M, Donaldson IM (1993) Inclusion body myositis presenting solely as dysphagia. Neurology 43:1241–1243
Sayers ME, Chou SM, Calabrese LH (1992) Inclusion body myositis: analysis of 32 cases. J Rheumatol 19:1385–1389
Shapiro J, Martin S, DeGirolami U, Goyal R (1996) Inflammatory myopathy causing pharyngeal dysphagia: a new entity. Ann Otol Rhinol Laryngol 105:331–335
Shaw DW, Cook IJ, Gabb M, Holloway RH, Simula ME, Panagopoulos V, Dent J (1995) Influence of normal aging on oral-pharyngeal and upper esophageal sphincter function during swallowing. Am J Physiol 268:G389–G396
Williams RB, Grehan MJ, Hersch M, Andre J, Cook IJ (2003) Biomechanics, diagnosis, and treatment outcome in inflammatory myopathy presenting as oropharyngeal dysphagia. Gut 52:471–478
Wintzen AR, Badrising UA, Roos RA, Vielvoye J, Liauw L, Pauwels EK (1994) Dysphagia in ambulant patients with Parkinson’s disease: common, not dangerous. Can J Neurol Sci 21:53–56
Wintzen AR, Bots GT, de Bakker HM, Hulshof JH, Padberg GW (1988) Dysphagia in inclusion body myositis. J Neurol Neurosurg Psychiatry 51:1542–1545
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
For the Dutch IBM study group
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 1 (MPG 1552 kb)
Supplementary material 2 (MPG 4436 kb)
Appendix
Appendix
Authors and investigators of the Dutch IBM Study Group include the following: M. L. C. Maat-Schieman (Department of Neurology, Leiden University Medical Center); P. van Doorn (Department of Neurology, Erasmus Medical Center, Rotterdam); B. G. M. van Engelen (Department of Neurology, Radboud University Nijmegen Medical Center); C. G. Faber (Department of Neurology, Academic Hospital Maastricht); J. E. Hoogendijk (Department of Neurology, University Medical Center Utrecht) and M. de Visser (Department of Neurology, Academic Medical Center Amsterdam).
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Cox, F.M., Verschuuren, J.J., Verbist, B.M. et al. Detecting dysphagia in inclusion body myositis. J Neurol 256, 2009–2013 (2009). https://doi.org/10.1007/s00415-009-5229-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-009-5229-9