Abstract
Traumatic brain injury (TBI) is a major cause of death and its accurate diagnosis is an important concern of daily forensic practice. However, it can be challenging to diagnose TBI in cases where macroscopic signs of the traumatic head impact are lacking and little is known about the circumstances of death. In recent years, several post-mortem studies investigated the possible use of biomarkers for providing objective evidence for TBIs as the cause of death or to estimate the survival time and time since death of the deceased. This work systematically reviewed the available scientific literature on TBI-related biomarkers to be used for forensic purposes. Post-mortem TBI-related biomarkers are an emerging and promising resource to provide objective evidence for cause of death determinations as well as survival time and potentially even time since death estimations. This literature review of forensically used TBI-biomarkers revealed that current markers have low specificity for TBIs and only provide limited information with regards to survival time estimations and time since death estimations. Overall, TBI fatality-related biomarkers are largely unexplored in compartments that are easily accessible during autopsies such as urine and vitreous humor. Future research on forensic biomarkers requires a strict distinction of TBI fatalities from control groups, sufficient sample sizes, combinations of currently established biomarkers, and novel approaches such as metabolomics and mi-RNAs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As defined by the US Centers for Disease Control and Prevention, a traumatic brain injury (TBI) describes a disruption of the brain’s normal function caused by bumps, blows, jolts, or penetrating head injuries [1]. TBI considerably contributes to the global injury burden and in light of a growing population, the absolute number of TBIs is expected to grow further [2]. A lethal outcome occurs in approximately a quarter to a third of patients who suffer a severe TBI, which is about the same percentage compared to the ones that fully recover from a severe traumatic head impact [3]. A TBI-related death most often results from intentional self-harm (33%), followed by unintentional falls (28%) and motor vehicle accidents (19%) [4]. Hence, it is not surprising that TBI is an important topic for forensic pathologists with cases ranging from suicidal head banging [5] to homicidal head blows [6]. Especially, when macroscopic signs of head impacts such as contusions, bleedings, or lacerations are lacking, it can be challenging to determine a TBI as the sole or contributing cause of death [7]. Post-mortem biochemical analyses could be a promising objective resource for forensic pathologists to diagnose lethal TBIs as the cause of death. Forensic biochemical investigations are already described and widely used for the cause of death determination of hypothermia, ketoacidosis, myocardial infarction, drowning, or anaphylaxis [8]. From ante-mortem studies, it is known that several biomarkers show significant differences following traumatic head impacts compared to atraumatic controls [9, 10]. On that basis, several forensic groups have explored the potential to use those TBI biomarkers for forensic purposes in a post-mortem setting [7, 11,12,13]. However, forensic expectations on TBI biomarkers as well as the conditions under which the samples are obtained considerably differ from ante-mortem clinical practice. Clinically used TBI biomarkers provide information on the diagnosis, prognosis, and treatment efficiency of TBIs [14]. In contrast, forensic pathologists expect additional objective data on TBI survival time estimations or time since death estimations [15, 16]. Ante-mortem, TBI biomarkers are determined in blood or cerebrospinal fluid (CSF), which are sampled from living individuals under aseptic conditions [17]. Contrary to that, the body fluids for the determination of TBI biomarkers in forensic cases are sampled from dead and often at least partly putrefied individuals during forensic autopsies. Post-mortem changes and sampling conditions raise the question of whether forensic biochemical investigations can provide any valuable information at all [7, 18]. Contrary to the clinical setting, practically all tissues of the human body can be used to determine TBI biomarkers in forensic investigations. However, as post-mortem reference values for different causes of death are lacking, their potential value for forensic investigations related to TBI fatalities has to be explored from scratch. This given work provides an up-to-date review of the post-mortem biochemistry of lethal TBIs including information on their value for forensically relevant topics such as cause of death determinations, survival time estimations, and time since death estimations. Also, it will be compiled whether these TBI biomarkers are relevantly influenced by factors such as age, sex, hemolysis, perimortem rescue procedures, or storage conditions. Thus far, a forensically focused TBI biomarker review is not available. The following eight biomarkers were chosen to be presented in this review: S100 calcium-binding protein B (S100B), neuron-specific enolase (NSE), glial fibrillary acidic protein (GFAP), interleukin-6 (IL-6), brain-derived neurotrophic factor (BDNF), and microtubule-associated protein tau (MAPT), which were selected as these are well-known candidate fluid biomarkers related to TBI pathophysiology [19]. Furthermore, lactate dehydrogenase (LDH), ferritin, and neutrophil gelatinase-associated lipocalin (NGAL) were chosen to be presented here based on previous own post-mortem studies of the authors. However, the search strategy was not limited to the selected biomarkers to avoid the risk of missing important others.
Materials/Methods
The here performed review of post-mortem TBI biomarkers contains the following two components: (i) a systematic component of previous post-mortem studies to detect a fatal TBI including the following biomarkers: S100B, NSE, GFAP, IL-6, LDH, Ferritin, BDNF, NGAL, and MPAT; (ii) data from peer-reviewed studies that summarize information from clinical studies on the respective biomarker or laboratory analyses, which were not part of the strategic search but provide important context for the forensic investigations. This literature review compiles the following information for each of the abovementioned biomarkers:
-
Molecular weight - what is the molecular weight of the respective marker?
-
Expression - where is the biomarker expressed within the human body?
-
Function - which function does the marker serve within the human body (as far as this has been answered to date)?
-
Cause of death determination - does the biomarker allow to significantly differentiate lethal TBIs and non-TBI control cases?
-
Survival time estimation - does the biomarker discriminate different survival times between the traumatic head impact and the death on a statistically significant level?
-
Post-mortem interval correlation - was the marker discriminative with regards to the post-mortem interval (PMI) on a statistically significant level? The PMI refers to the time between the death of the cadaver and the autopsy, in which the tissues undergo alterations such as degradation or putrefaction.
-
Reason for biomarker level change within compartment - which mechanism underlies the significantly different biomarker concentration between TBI fatalities and controls in the respective compartment?
-
Age- or sex-dependence - did the biomarker correlate with the age at death or the sex of the deceased in the respective compartment on a statistically significant level?
-
Hemolysis index (H-index) dependence - did the biomarker level correlate with the hemolysis index of the fluid sample on a statistically significant level?
-
Influence of rescue procedures or intensive care procedures - was the biomarker level in the respective compartment significantly different, if the deceased was subjected to rescue (e.g., cardiopulmonary resuscitation attempt) or intensive care unit procedures (e.g., neurosurgical intervention)?
-
Comparison to clinical biomarker levels - how were the TBI-related biomarker levels measured in a forensic setting compared to known clinical values of the identical compartment?
-
In vitro freeze–thaw-cycle influence - did the in vitro biomarker concentration within a forensically relevant compartment correlate with the number of applied freeze–thaw cycles on a statistically significant level?
-
In vitro biomarker stability - does the in vitro measured biomarker concentration within a forensically relevant compartment change over time on a statistically significant level? P-values of 0.05 or less were considered to be statistically significant.
The information for the points cause of death determination, survival time estimation, age- or sex-dependence, H-index, and the post-mortem biomarker levels for the comparison to the clinical values were extracted from PubMed-listed forensic studies. These were searched up until August 2021 according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines [20] (Fig. 1). Initially, the articles were screened by their title and abstract. If the title and/or abstract revealed that the selected TBI-related biomarkers were measured in post-mortem tissues, the full text was sought for retrieval and assessed for eligibility. Then, the reference lists of the respective papers were screened. The following inclusion criteria were defined: (i) TBI as the cause of death, (ii) study must contain a control group, (iii) only studies on humans, and (iv) only peer-reviewed original works. The systematic part of the literature review was independently performed by two authors (JZ and RK) according to the inclusion criteria that are listed in Fig. 1. A third author (BO) checked the results for accuracy and decided, whether information that the two authors (JZ and RK) could not agree on should be included.
Results
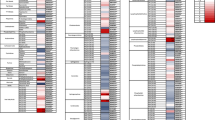
A total of 17 studies were identified from the literature search (Fig. 2). Of these, six studies reported results dealing with IL-6 [21,22,23,24,25,26]; five with GFAP [11, 13, 24, 26, 27], LDH [23, 24, 26, 28, 29], and S100B [7, 26, 30,31,32]; four with NSE [24, 26, 30, 31]; three with BDNF [11, 24, 26], MAPT [13, 33, 34], and ferritin [23, 24, 26]; and two with NGAL [11, 26]. Information regarding cause of death determination and survival time estimation are presented below. The rest of the extracted data is compiled in Tables 1, 2, and 3. The used body fluids for the measurement of TBI-related biomarkers in previous studies and the hypotheses that explain the biomarker alterations after the traumatic head impact are depicted in Figs. 3 and 4.
PRISMA flow chart for the methodology undertaken for the screening of relevant literature based on Moher et al. [20]
Several methods for the change in biomarker concentrations following traumatic head impacts are depicted for CSF and blood (exemplified on astrocytes). In response to a traumatic head impact, biomarkers can be secreted from intact astrocytes (A) or released from damaged astrocytes (B). Blood–brain barrier disruptions then cause an increase of biomarkers in the blood (C). Also, elevated biomarkers from the periphery could leak into the CSF via the disrupted blood–brain barrier (D)
S100 calcium-binding protein B
Cause of death determination
CSF concentrations of S100B were significantly higher in TBI fatalities compared to controls (isolated torso trauma, cerebrovascular injury, and sudden natural deaths) [30, 31]. Recently, it was stated that a fatal acute TBI (survival time less than 2 h) can be detected with 79% accuracy and 97% specificity in post-mortem CSF when the S100B concentration reaches a threshold of 2267 ng/ml [26]. In serum, S100B was significantly higher in TBI cases compared with isolated torso traumas but was not statistically different from cases with cerebrovascular insufficiency and sudden natural deaths in a small sample size investigating 17 TBI fatalities and 23 controls [30]. However, all aforementioned controls were not statistically different from TBI fatalities in serum in a larger sample size of 45 TBI fatalities and 47 controls [31]. Serum S100B levels were significantly correlated with the severity of head injury [7]. It was observed that post-mortem serum S100B levels were also significantly elevated in fatalities with non-TBI-related brain injuries such as strangulation or hanging [7]. Also, significantly higher S100B concentrations were observed in serum of TBI fatalities compared to isolated torso traumas but not cerebrovascular injuries and sudden natural deaths [30].
Survival time estimation
CSF S100B levels were consistently increased compared to controls throughout survival times of up to 10 days [30, 31]. CSF S100B levels > 10,000 ng/ml were observed only in TBI fatalities with survival times of at least 20 min and in every TBI fatality with survival times between 2 h and 5 days [30]. Serum levels of subacute TBI fatalities (survival times between 3 and 48 h) were significantly higher compared to acute (survival time of few seconds to 42 min) TBI fatalities [30]. Serum S100B levels decreased again 72 h after traumatic head impact [30].
Neuron-specific enolase
Cause of death determination
CSF samples of NSE have been determined as reliable measurements of TBI fatalities as levels were significantly elevated in TBI cases when compared to controls that died from isolated torso traumas and sudden natural deaths but not from acute myocardial infarctions [31]. NSE values in CSF > 6000 ng/ml were only observed in TBI fatalities, but not in control fatalities (isolated torso trauma, cerebrovascular insufficiency, and sudden natural death) [30]. Both NSE CSF and serum levels were not statistically different in TBI fatalities that showed a macroscopically visible brain contusion (and intracerebral bleeding) compared to cases that only revealed intracerebral bleeding [31]. Serum levels of TBI fatalities were statistically non-different from control cases (isolated torso trauma, cerebrovascular insufficiency, and sudden natural death) [30].
Survival time estimation
CSF NSE values > 6000 ng/ml were exclusively detected in TBI cases with a survival time between 15 min and 5 days [30]. Recently, it was stated that a lethal acute TBI (survival time less than 2 h) can be detected with an accuracy of 83% and a specificity of 97% in post-mortem CSF when the NSE concentration reaches a threshold value of 599 ng/ml [26]. Peak CSF concentrations of NSE were reached within survival times of 3 to 4 days [31]. No significantly different CSF NSE concentrations between TBI fatalities and controls that died from hypoxia, sudden cardiac events, or miscellaneous causes were observed within a mean TBI survival time of 1 h [29]. For TBI fatalities with a maximum survival time of up to 2 h, CSF NSE levels were shown to be significantly higher compared to cases of diffuse cerebral hypoxia and isolated torso trauma, but not acute myocardial infarctions [31]. Serum levels of NSE did not correlate with the survival times of TBI fatalities on a statistically significant level [30].
Glial fibrillary acidic protein
Cause of death determination
CSF and serum GFAP levels have been shown to be significantly increased in TBI fatalities compared to myocardial infarction and isolated torso trauma deaths, but not diffuse cerebral hypoxia [11, 13]. Post-mortem CSF GFAP levels are not specific for TBI fatalities, as they revealed a higher median for diffuse cerebral hypoxia compared to acute (survival times of less than 2 h) and delayed (survival times between 72 and 456 h) TBI fatalities [11]. When the GFAP CSF level exceeds 385.5 ng/ml, a fatal TBI can be diagnosed with a sensitivity of 71.1% and a specificity of 71.4% [11]. For fatal TBIs with a survival time of fewer than 2 h, a GFAP CSF concentration of 134 ng/ml discriminates a TBI fatality from control fatalities (acute myocardial infarction, diffuse cerebral hypoxia, and isolated torso trauma) with an accuracy of 78% and a specificity of 94% [26]. Contrary to the study of Ondruschka et al. [11], another post-mortem study revealed no differences in serum GFAP level between fatalities with macroscopically visible brain damage (including TBI) compared to control fatalities (cardiac cause, respiratory cause, intoxications, exsanguinations, or multi-organ failures) [27]. In serum, a fatal TBI can be diagnosed with a sensitivity of 76.2% and a specificity of 73.8% once the GFAP concentration surpasses 0.91 ng/ml [11]. Huge inter-individual variations were observed for both GFAP CSF and serum levels [11].
Survival time estimation
In CSF, the GFAP level peaks in the subacute group (survival time between 2 and 60 h). However, no significant difference was detected between the different TBI survival times neither in CSF nor in serum [11]. In serum, GFAP levels peak in acute TBI fatalities (survival times of less than 2 h) and, with increasing TBI survival times up to 456 h, approximate the concentrations of the control group (acute myocardial infarction, diffuse cerebral hypoxia, and isolated torso trauma) [11].
Interleukin-6
Cause of death determination
IL-6 levels in CSF and serum are significantly higher in TBI fatalities compared to non-infectious controls for which the survival time was assumed to be zero such as atraumatic hypoxic brain damage or acute myocardial infarction [11, 21]. When IL-6 levels of TBI fatalities were compared to fatalities that died from isolated torso trauma, CSF but not serum levels were significantly higher [11]. Recently, it was shown that a lethal acute TBI (survival time less than 2 h) can be detected with an accuracy of 86% and a specificity of 96% in post-mortem CSF when the IL-6 concentration reaches a threshold value of 99.1 pg/ml [26]. Trauma fatalities including TBI fatalities revealed significantly higher serum values compared to atraumatic deaths resulting from atraumatic causes of death as well as natural deaths [22].
Survival time estimation
With regards to the TBI survival time, no statistically significant differences of IL-6 levels were detected in post-mortem CSF and serum samples within an investigated survival time span of at least 3 days [11]. However, CSF IL-6 levels of more than 100,000 pg/ml were only detected in TBI fatalities with a survival time of more than three days [23].
Lactate dehydrogenase
Cause of death determination
LDH CSF levels of TBI fatalities (all survival times pooled between a few seconds and 19 days) are significantly higher compared to controls that died from isolated torso trauma, diffuse cerebral hypoxia, or acute myocardial infarction [23]. Also, LDH CSF levels were higher in TBI fatalities compared to fatalities due to hypoxia, sudden cardiac death, or natural and non-natural deaths that could not be attributed to any of the former [28, 29]. Recently, it was stated that a lethal acute TBI (survival time less than 2 h) can be detected with an accuracy of 81% and a specificity of 97% in post-mortem CSF when the LDH concentration reaches a threshold value of 16.71 ukat/l [26]. Serum LDH levels of TBI fatalities (all survival times between a few seconds and 19 days pooled) were only higher compared to isolated torso traumas, but not for diffuse cerebral hypoxia or acute myocardial infarctions [23]. In vitreous humor, LDH levels were higher in TBI fatalities compared to sudden cardiac deaths, but lower than hypoxia-related deaths or natural and non-natural deaths that could not be classified as TBI-related, hypoxia, or sudden cardiac deaths [28]. However, it was not mentioned whether the former results in vitreous humor were statistically significant [28].
Survival time estimation
For CSF, LDH levels were shown to be stable for survival times between a few seconds and 19 days in one study [23] but decreased in another study that investigated a TBI fatality group with a mean survival time of 1 h [29]. Serum LDH levels have not been stated to vary on a statistically significant level for TBI fatalities with survival times ranging from a few seconds to 19 days [23]. No statistically significant survival time dependence was stated for vitreous humor levels of LDH [29].
Ferritin
Cause of death determination
CSF ferritin levels of TBI fatalities were significantly higher compared to each of the following fatality groups: isolated torso trauma, diffuse cerebral hypoxia, and acute myocardial infarction [23]. CSF ferritin levels of > 8.0 mg/l were only reached by TBI fatalities but none of the aforementioned controls fatalities [23]. Recently, it was stated that a lethal acute TBI (survival time less than 2 h) can be detected with an accuracy of 87% and a specificity of 96% in post-mortem CSF when the ferritin concentration reaches a threshold value of 1.73 mg/l [26]. In serum, the pooled TBI fatalities were only significantly higher compared to diffuse cerebral hypoxia fatalities, but not for acute myocardial infarctions of isolated torso traumata [23].
Survival time estimation
Both CSF and serum levels of ferritin were significantly higher for TBI fatalities with a survival time of more than 72 h (maximum 19 days) compared to survival times between a few seconds and 43 h [23]. A CSF ferritin level of > 30.0 mg/l was only reached after a minimum TBI survival time of 2 h [23].
Brain-derived neurotrophic factor
Cause of death determination
CSF BDNF values are discriminative between TBI fatalities and fatalities that died from diffuse cerebral hypoxia and acute myocardial infarction but not from isolated torso trauma [11]. A TBI fatality can be diagnosed post-mortem with a sensitivity of 71.0% and a specificity of 83.3% when a CSF BDNF level of 29.0 pg/ml is reached [11]. Recently, it was noted that a lethal acute TBI (survival time less than 2 h) can be detected with an accuracy of 86% and a specificity of 96% in post-mortem CSF when the BDNF concentration reaches a threshold value of 11.1 pg/ml [26]. Serum BDNF values of TBI fatalities were statistically non-different from the aforementioned control groups [11]. Huge inter-individual variations were observed for BDNF CSF and serum levels [11].
Survival time estimation
Both CSF and serum levels of TBI fatalities revealed the highest median levels in acute TBI fatalities with a survival time between a few seconds and 107 min [11]. The CSF and serum values of BDNF decreased with increasing survival times [11]. However, neither CSF nor serum levels revealed statistically significant BDNF level changes between the trauma survival time groups (survival times between a few seconds and 456 h), which renders the marker not useful for survival time estimations [11].
Neutrophil gelatinase-associated lipocalin(lipocalin-2)
Cause of death determination
NGAL CSF levels of TBI fatalities were significantly higher compared to each of the following control fatalities: isolated torso trauma, diffuse cerebral hypoxia, and acute myocardial infarction [11]. A CSF NGAL value of 1050.5 ng/ml detects a lethal TBI with a sensitivity of 72.7% and a specificity of 89.7% [11]. Huge inter-individual variations were observed for NGAL CSF levels [11]. A lethal acute TBI (survival time less than 2 h) can be detected with an accuracy of 84% and a specificity of 94% in post-mortem CSF when the NGAL concentration reaches a threshold value of 334.4 ng/ml [26]. Post-mortem NGAL serum measurements are not described yet.
Survival time estimation
CSF values of NGAL revealed the highest median values for survival times between 2 and 72 h; however, no statistically significant differences were observed regardless of the investigated survival times between a few seconds and 456 h of TBI fatalities [11].
Microtubule-associated protein Tau
Cause of death determination
Post-mortem CSF, serum, urine, and saliva levels of MAPT were significantly higher in a group consisting of TBI fatalities and fatalities with a suspected TBI as a co-morbidity based on macroscopic signs compared to a control group that consisted of deaths from sudden cardiopulmonary failures [33]. However, no statistically significant MAPT levels were found in vitreous humor between the aforementioned groups [33].
Discussion
Accurate and reliable evidence collection is an essential component of forensic medicine and thus makes an important contribution to the proper function of the legal system. Forensic biochemistry is an accepted part of particular forensic investigations [8] and research efforts have increased dramatically in the last decade [11,12,13, 23, 24, 26, 30, 33]. This review paper summarized the current literature on post-mortem biomarkers in TBI-related forensic questions. A critical consideration of the summarized findings and an outlook on this forensic niche is provided below.
The value of forensic biomarkers to determine a TBI as the cause of death
The summary given here revealed that several biomarkers discriminate between TBI fatalities and several different control fatalities at a statistically significant level. This indicates that forensic biochemistry is a promising field to provide additional objective data to determine TBI as the cause of death. Regarding this, several points have to be critically discussed based on this given review. Ideally, if a biomarker reaches a particular threshold value in a certain compartment, a lethal TBI can be diagnosed with 100% sensitivity and specificity, respectively. However, none of the biomarkers used in forensic science is specific for fatal TBI but shows significant changes in marker values in other fatalities as well, which is commonly much higher when compared to living subjects. Moreover, this summary highlights that each individual biomarker was statistically dependent on at least one co-factor such as PMI, hemolysis, or whether neurosurgery was performed. Together with unpredictable peri- and post-mortem changes including untraceable biomarker concentration changes in the respective compartments [134], the TBI-related biomarkers show enormous standard variations in both TBI fatalities and controls, which usually overlap. Therefore, none of the biomarkers used forensically to date is able to distinguish between TBI and non-TBI fatalities based on the concentration of a particular biomarker in 100% of cases. However, several cut-off values, mainly in CSF, have already been reported to corroborate the suspicion of a lethal TBI together with other post-mortem investigation results rather than to prove it independently [11, 23, 26, 30]. Indeed, the selection and careful categorization of control fatalities within the studies on post-mortem TBI-biomarkers are of special interest. For example, serum IL-6 can discriminate TBI fatalities from fatalities due to acute myocardial infarctions and diffuse cerebral hypoxias, but not from isolated torso traumas [23]. This information can provide valuable objective evidence when serum IL-6 concentration is considered together with other autopsy findings, e.g., when an isolated torso trauma can be excluded. Therefore, it is of higher importance to compare TBI fatalities with homogenous individual control groups rather than with a pooled control group of all non-TBI cases. When thresholds are set by individual studies, this is essentially against the selected (or available) control deaths. However, this literature review revealed that there is considerable variation in the definition of control deaths between studies, potentially affecting the respective results and conclusions. Apart from the voluntary allocation of fatalities to the TBI and control groups, a TBI fatality, or at least a fatality with a TBI as a confounding cause, could easily end up in the control group in some studies, affecting the results, which is more likely in cases without macroscopic correlates of the traumatic event against the head. Lastly, using forensic biochemistry might be challenging to reliably discriminate between TBI fatalities and control cases whenever the entire cohort is considered. However, it seems to be realistic to define “extreme” biomarker levels that are just achieved by TBI fatalities, which essentially means defining upper cut-off values that reflect 100% specificity with poor sensitivity. The CSF NSE values > 6000 ng/ml, which have just been reached in TBI fatalities [30], are an example of such an “extreme” cut-off value. It has to be mentioned that threshold values apply only when the same laboratory testing setup, and a measurement kit is used as in the respective study. However, this has to be validated against a broad variety of control fatalities to be valid with reasonable certainty. Some of the aforementioned studies revealed difficulties in defining cut-off values due to different measurement methods and inter-individual differences.
Post-mortem biomarkers for TBI survival time estimations - are they useful?
The previous research on TBI-related post-mortem biomarkers uncovered the potential of several biomarkers in various compartments to discriminate between different survival times of TBI fatalities. The factors that influence the cause of death determination can equally be listed for survival time estimations, explaining why particular biomarker levels that pinpoint certain survival times are lacking to date or, in fact, most likely impossible to achieve. However, the here given literature summary observed a trend that certain post-mortem TBI biomarkers can indicate minimum survival times if high biomarker values are reached [23, 30]. CSF levels of > 10,000 ng/ml for S100B [30], > 6000 ng/ml for NSE [30], > 30 mg/l for ferritin [23], and > 100,000 pg/ml for IL-6 [23] were only observed for minimum survival times of 20, 15, 120 min, and 3 days, respectively. Since a tendency for low biomarker concentrations can be suspected for short survival times [23], more such cut-off values for determining a minimum survival time probably exist for other compartments besides CSF but have not received sufficient attention so far. Future research on TBI survival time estimations using post-mortem biomarkers should report cut-off values for minimum survival times to further explore the potential of whether post-mortem biochemistry can provide reliable cut-off values for minimum survival times in TBI fatalities.
The role of post-mortem biomarkers in time since death estimations of TBI fatalities
Several biomarkers of various compartments correlated with the PMI [23, 28, 30, 31], being the fundamental requirement to be used for time since death estimations. However, this correlation was largely attributed to the increasing hemolysis occurring with increasing PMI. Future studies on fluid TBI-related biomarkers should provide additional quantitative information on the correlation between the biomarker concentrations and the PMI. Moreover, the use of cut-off values should be explored for PMI correlations as well. In light of the potentially inevitable influence of the progressive hemolysis in post-mortem samples, cut-off values for particularly short PMIs yielding low biomarker concentrations seem most promising in this regard. However, given the currently available information, post-mortem biomarkers seem to be of no merit for time since death estimations of TBI fatalities.
The present and future of post-mortem TBI-related biomarkers
This literature review demonstrated the potential of post-mortem biomarkers to provide objective evidence for cause of death determinations and survival time estimations of TBI fatalities. However, forensic biochemistry, as a promising investigative branch of forensic medicine, is still at the very beginning and data on particular causes of death such as TBI fatalities are scarce. Therefore, it is yet too early to include current observations into the daily routine without further verifications that respect detected pitfalls such as the influence of perimortem procedures or hemolysis on the biomarker levels. Equally, TBI-related biomarkers that did not reveal sufficient potential to provide additional information for forensically relevant investigations should not be neglected too soon as these results could have been biased by limited sample sizes or the inaccurate allocation of TBI fatalities to the control group and vice versa. LDH and MPAT were the only two biomarkers that were investigated in post-mortem samples other than CSF, serum, or the brain so far [28, 33]. Especially, MPAT demonstrated the potential of discriminating TBI fatalities from controls in urine and saliva and these two compartments should be further investigated using other biomarkers. Moreover, other promising clinically relevant TBI biomarkers should be investigated in post-mortem body fluids in the future. These include for example αII-spectrin breakdown products, myelin basic protein, neurofilament proteins, ubiquitin C-terminal hydrolase-L1, tumor necrosis factor alpha, or interleukin-1B [19]. Ideally, all observations on post-mortem biomarkers including but not limited to the ones of TBI fatalities should be collected in forensic biochemical databases to further explore the opportunities and challenges of this emerging post-mortem field allowing for collective sample sizes that surpass the ones of individual departments by far.
Recent pioneering works regarding the consideration of mi-RNAs [135] or the entity of metabolites (metabolome) [136, 137] to prove lethal TBIs in a forensic setting should be further explored. Using a combination of six different mi-RNAs, it was possible to discriminate TBI cases from controls that were free of neurological symptoms [135]. Even though the former study was based on ante-mortem blood samples, the six candidate mi-RNAs were identified and validated on 38 post-mortem brain tissues before [135, 138]. Groups of metabolites were shown to be relevantly elevated in TBI fatalities compared to controls in post-mortem CSF [136]. Future studies will tell whether mi-RNAs and metabolites are superior to the forensically used TBI biomarkers that were discussed in this review and if/how much a combination of all these fluid biomarker groups can benefit forensic practice.
Limitations
Based on the selected search criteria, especially the selected search terms, some relevant articles might have been missed. Initially, the articles were retrieved through title screening, which might have led to an exclusion of relevant articles based on inappropriate title selection by the respective authors or misinterpretation by the authors of this given literature review. Location bias might have led to an oversight of articles in less accessible journals.
Conclusions
Forensic TBI-biomarkers are an emerging and promising resource to provide objective evidence for cause of death determinations and survival time estimations. However, all TBI-biomarkers that were forensically investigated to date are unspecific for TBIs and only allow for particular information such as detections of TBI fatalities with poor sensitivity or minimum survival time estimations. Future research on forensic biomarkers requires a strict separations of TBI fatalities and control groups with sufficient sample sizes, the exploration of the current biomarkers in additional compartments such as urine, saliva, and vitreous humor, the addition of further clinically promising biomarkers to the forensic field, and the in-depth forensic exploration of promising biomarker categories such as metabolites or mi-RNAs.
References
Faul M, Coronado V (2015) Epidemiology of traumatic brain injury. Handb Clin Neurol 127:3–13. https://doi.org/10.1016/B978-0-444-52892-6.00001-5
GBD 2016 Neurology Collaborators (2019) Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 18:56–87. https://doi.org/10.1016/S1474-4422(18)30415-0
Jiang JY, Gao GY, Li WP, Yu MK, Zhu C (2002) Early indicators of prognosis in 846 cases of severe traumatic brain injury. J Neurotrauma 19:869–874. https://doi.org/10.1089/08977150260190456
Capizzi A, Woo J, Verduzco-Gutierrez M (2020) Traumatic brain injury: an overview of epidemiology, pathophysiology, and medical management. Med Clin North Am 104:213–238. https://doi.org/10.1016/j.mcna.2019.11.001
Chester V, Alexander RT (2018) Head banging as a form of self-harm among inpatients within forensic mental health and intellectual disability services. J Forensic Psychiatry Psychol 29:557–573
Kremer C, Racette S, Dionne CA, Sauvageau A (2008) Discrimination of falls and blows in blunt head trauma: systematic study of the hat brim line rule in relation to skull fractures. J Forensic Sci 53:716–719. https://doi.org/10.1111/j.1556-4029.2008.00725.x
Li DR, Zhu BL, Ishikawa T, Zhao D, Michiue T, Maeda H (2006) Postmortem serum protein S100B levels with regard to the cause of death involving brain damage in medicolegal autopsy cases. Leg Med (Tokyo) 8:71–77. https://doi.org/10.1016/j.legalmed.2005.07.004
Belsey SL, Flanagan RJ (2016) Postmortem biochemistry: current applications. J Forensic Leg Med 41:49–57. https://doi.org/10.1016/j.jflm.2016.04.011
Goyal A, Failla MD, Niyonkuru C et al (2013) S100b as a prognostic biomarker in outcome prediction for patients with severe traumatic brain injury. J Neurotrauma 30:946–957. https://doi.org/10.1089/neu.2012.2579
Kumar RG, Diamond ML, Boles JA et al (2015) Acute CSF interleukin-6 trajectories after TBI: associations with neuroinflammation, polytrauma, and outcome. Brain Behav Immun 45:253–262. https://doi.org/10.1016/j.bbi.2014.12.021
Ondruschka B, Sieber M, Kirsten H, Franke H, Dressler J (2018) Measurement of cerebral biomarkers proving traumatic brain injuries in post-mortem body fluids. J Neurotrauma 35:2044–2055. https://doi.org/10.1089/neu.2017.5441
Zwirner J, Anders S, Bohnert S et al (2021) Screening for fatal traumatic brain injuries in cerebrospinal fluid using blood-validated CK and CK–MB immunoassays. Biomolecules 11:1061. https://doi.org/10.3390/biom11071061
Olczak M, Kwiatkowska M, Niderla-Bielinska J, Chutoranski D, Tarka S, Wierzba-Bobrowicz T (2018) Brain-originated peptides as possible biochemical markers of traumatic brain injury in cerebrospinal fluid post-mortem examination. Folia Neuropathol 56:97–103. https://doi.org/10.5114/fn.2018.76613
Dash PK, Zhao J, Hergenroeder G, Moore AN (2010) Biomarkers for the diagnosis, prognosis, and evaluation of treatment efficacy for traumatic brain injury. Neurotherapeutics 7:100–114. https://doi.org/10.1016/j.nurt.2009.10.019
Ondruschka B, Babian C, Neef M, Zwirner J, Schwarz M (2019) Entomological and cardiologic evidence of time since death in short postmortem intervals. J Forensic Sci 64:1563–1567. https://doi.org/10.1111/1556-4029.14010
Trautz F, Franke H, Bohnert S et al (2019) Survival-time dependent increase in neuronal IL-6 and astroglial GFAP expression in fatally injured human brain tissue. Sci Rep 9:11771. https://doi.org/10.1038/s41598-019-48145-w
Agoston DV, Shutes-David A, Peskind ER (2017) Biofluid biomarkers of traumatic brain injury. Brain Inj 31:1195–1203. https://doi.org/10.1080/02699052.2017.1357836
Luna A (2009) Is postmortem biochemistry really useful? Why is it not widely used in forensic pathology? Leg Med (Tokyo) 11(Suppl 1):S27-30. https://doi.org/10.1016/j.legalmed.2009.02.040
Zetterberg H, Blennow K (2016) Fluid biomarkers for mild traumatic brain injury and related conditions. Nat Rev Neurol 12:563–574. https://doi.org/10.1038/nrneurol.2016.127
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2010) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 8:336–41. https://doi.org/10.1016/j.ijsu.2010.02.007
Mimasaka S, Funayama M, Hashiyada M, Nata M, Tsunenari S (2007) Significance of levels of IL-6 and IL-8 after trauma: a study of 11 cytokines post-mortem using multiplex immunoassay. Injury 38:1047–1051. https://doi.org/10.1016/j.injury.2007.02.045
Mimasaka S, Hashiyada M, Nata M, Funayama M (2001) Correlation between serum IL-6 levels and death: usefulness in diagnosis of “traumatic shock”? Tohoku J Exp Med 193:319–324. https://doi.org/10.1620/tjem.193.319
Ondruschka B, Schuch S, Pohlers D, Franke H, Dressler J (2018) Acute phase response after fatal traumatic brain injury. Int J Legal Med 132:531–539. https://doi.org/10.1007/s00414-017-1768-2
Ondruschka B, Woydt L, Bernhard M et al (2019) Post-mortem in situ stability of serum markers of cerebral damage and acute phase response. Int J Legal Med 133:871–881. https://doi.org/10.1007/s00414-018-1925-2
Mimasaka S (2002) Postmortem cytokine levels and the cause of death. Tohoku J Exp Med 197:145–150. https://doi.org/10.1620/tjem.197.145
Zwirner J, Bohnert S, Franke H et al (2021) Assessing protein biomarkers to detect lethal acute traumatic brain injuries in cerebrospinal fluid. Biomolecules 11(11):1577. https://doi.org/10.3390/biom11111577
Breitling B, Brunkhorst R, Verhoff M, Foerch C (2018) Post-mortem serum concentrations of GFAP correlate with agony time but do not indicate a primary cerebral cause of death. PLoS ONE 13:e0205323. https://doi.org/10.1371/journal.pone.0205323
Osuna E, Perez-Carceles MD, Luna A, Pounder DJ (1992) Efficacy of cerebro-spinal fluid biochemistry in the diagnosis of brain insult. Forensic Sci Int 52:193–198. https://doi.org/10.1016/0379-0738(92)90107-8
Vazquez MD, Sanchez-Rodriguez F, Osuna E et al (1995) Creatine kinase BB and neuron-specific enolase in cerebrospinal fluid in the diagnosis of brain insult. Am J Forensic Med Pathol 16:210–214. https://doi.org/10.1097/00000433-199509000-00004
Ondruschka B, Pohlers D, Sommer G et al (2013) S100B and NSE as useful postmortem biochemical markers of traumatic brain injury in autopsy cases. J Neurotrauma 30:1862–1871. https://doi.org/10.1089/neu.2013.2895
Sieber M, Dressler J, Franke H, Pohlers D, Ondruschka B (2018) Post-mortem biochemistry of NSE and S100B: a supplemental tool for detecting a lethal traumatic brain injury? J Forensic Leg Med 55:65–73. https://doi.org/10.1016/j.jflm.2018.02.016
Li DR, Zhu BL, Ishikawa T, Zhao D, Michiue T, Maeda H (2006) Immunohistochemical distribution of S-100 protein in the cerebral cortex with regard to the cause of death in forensic autopsy. Leg Med (Tokyo) 8:78–85. https://doi.org/10.1016/j.legalmed.2005.09.002
Olczak M, Poniatowski LA, Niderla-Bielinska J et al (2019) Concentration of microtubule associated protein tau (MAPT) in urine and saliva as a potential biomarker of traumatic brain injury in relationship with blood-brain barrier disruption in postmortem examination. Forensic Sci Int 301:28–36. https://doi.org/10.1016/j.forsciint.2019.05.010
Olczak M, Niderla-Bielinska J, Kwiatkowska M, Samojlowicz D, Tarka S, Wierzba-Bobrowicz T (2017) Tau protein (MAPT) as a possible biochemical marker of traumatic brain injury in postmortem examination. Forensic Sci Int 280:1–7. https://doi.org/10.1016/j.forsciint.2017.09.008
Plog BA, Dashnaw ML, Hitomi E et al (2015) Biomarkers of traumatic injury are transported from brain to blood via the glymphatic system. J Neurosci 35:518–526. https://doi.org/10.1523/JNEUROSCI.3742-14.2015
Haque A, Ray SK, Cox A, Banik NL (2016) Neuron specific enolase: a promising therapeutic target in acute spinal cord injury. Metab Brain Dis 31:487–495. https://doi.org/10.1007/s11011-016-9801-6
Zoltewicz JS, Mondello S, Yang B et al (2013) Biomarkers track damage after graded injury severity in a rat model of penetrating brain injury. J Neurotrauma 30:1161–1169. https://doi.org/10.1089/neu.2012.2762
Tanaka T, Narazaki M, Kishimoto T (2014) IL-6 in inflammation, immunity, and disease. Cold Spring Harb Perspect Biol 6:a016295. https://doi.org/10.1101/cshperspect.a016295
Ghandour MS, Labourdette G, Vincendon G, Gombos G (1981) A biochemical and immunohistological study of S100 protein in developing rat cerebellum. Dev Neurosci 4:98–109. https://doi.org/10.1159/000112745
Krohn M, Dressler J, Bauer M, Schober K, Franke H, Ondruschka B (2015) Immunohistochemical investigation of S100 and NSE in cases of traumatic brain injury and its application for survival time determination. J Neurotrauma 32:430–440. https://doi.org/10.1089/neu.2014.3524
Sen J, Belli A (2007) S100B in neuropathologic states: the CRP of the brain? J Neurosci Res 85:1373–1380. https://doi.org/10.1002/jnr.21211
Cocchia D, Miani N (1980) Immunocytochemical localization of the brain-specific S-100 protein in the pituitary gland of adult rat. J Neurocytol 9:771–782. https://doi.org/10.1007/BF01205018
Vila-Porcile E (1972) The network of the folliculo-stellate cells and the follicles of the adenohypophysis in the rat (pars distalis). Z Zellforsch Mikrosk Anat 129:328–369
Schmechel D, Marangos PJ, Brightman M (1978) Neurone-specific enolase is a molecular marker for peripheral and central neuroendocrine cells. Nature 276:834–836. https://doi.org/10.1038/276834a0
Haimoto H, Takahashi Y, Koshikawa T, Nagura H, Kato K (1985) Immunohistochemical localization of gamma-enolase in normal human tissues other than nervous and neuroendocrine tissues. Lab Invest 52:257–263
Eng LF (1985) Glial fibrillary acidic protein (GFAP): the major protein of glial intermediate filaments in differentiated astrocytes. J Neuroimmunol 8:203–214. https://doi.org/10.1016/s0165-5728(85)80063-1
Arneson D, Zhang G, Ying Z et al (2018) Single cell molecular alterations reveal target cells and pathways of concussive brain injury. Nat Commun 9:3894. https://doi.org/10.1038/s41467-018-06222-0
Hol EM, Roelofs RF, Moraal E et al (2003) Neuronal expression of GFAP in patients with Alzheimer pathology and identification of novel GFAP splice forms. Mol Psychiatry 8:786–796. https://doi.org/10.1038/sj.mp.4001379
Bender BL, Yunis EJ (1980) Central nervous system pathology of tuberous sclerosis in children. Ultrastruct Pathol 1:287–299. https://doi.org/10.3109/01913128009141432
Yang Z, Wang KK (2015) Glial fibrillary acidic protein: from intermediate filament assembly and gliosis to neurobiomarker. Trends Neurosci 38:364–374. https://doi.org/10.1016/j.tins.2015.04.003
Brenner M (1994) Structure and transcriptional regulation of the GFAP gene. Brain Pathol 4:245–257. https://doi.org/10.1111/j.1750-3639.1994.tb00840.x
Sanceau J, Falcoff R, Beranger F, Carter DB, Wietzerbin J (1990) Secretion of interleukin-6 (IL-6) by human monocytes stimulated by muramyl dipeptide and tumour necrosis factor alpha. Immunology 69:52–56
Benveniste EN, Sparacio SM, Norris JG, Grenett HE, Fuller GM (1990) Induction and regulation of interleukin-6 gene expression in rat astrocytes. J Neuroimmunol 30:201–212. https://doi.org/10.1016/0165-5728(90)90104-u
Woodroofe MN, Sarna GS, Wadhwa M et al (1991) Detection of interleukin-1 and interleukin-6 in adult rat brain, following mechanical injury, by in vivo microdialysis: evidence of a role for microglia in cytokine production. J Neuroimmunol 33:227–236. https://doi.org/10.1016/0165-5728(91)90110-s
Welc SS, Clanton TL (2013) The regulation of interleukin-6 implicates skeletal muscle as an integrative stress sensor and endocrine organ. Exp Physiol 98:359–371. https://doi.org/10.1113/expphysiol.2012.068189
Akira S, Taga T, Kishimoto T (1993) Interleukin-6 in biology and medicine. Adv Immunol 54:1–78. https://doi.org/10.1016/s0065-2776(08)60532-5
Donato R, Sorci G, Riuzzi F et al (2009) S100B’s double life: intracellular regulator and extracellular signal. Biochim Biophys Acta 1793:1008–1022. https://doi.org/10.1016/j.bbamcr.2008.11.009
Van Eldik LJ, Christie-Pope B, Bolin LM, Shooter EM, Whetsell WO Jr (1991) Neurotrophic activity of S-100 beta in cultures of dorsal root ganglia from embryonic chick and fetal rat. Brain Res 542:280–285. https://doi.org/10.1016/0006-8993(91)91579-p
Willoughby KA, Kleindienst A, Muller C, Chen T, Muir JK, Ellis EF (2004) S100B protein is released by in vitro trauma and reduces delayed neuronal injury. J Neurochem 91:1284–1291. https://doi.org/10.1111/j.1471-4159.2004.02812.x
Selinfreund RH, Barger SW, Pledger WJ, Van Eldik LJ (1991) Neurotrophic protein S100 beta stimulates glial cell proliferation. Proc Natl Acad Sci U S A 88:3554–3558. https://doi.org/10.1073/pnas.88.9.3554
Hu J, Van Eldik LJ (1996) S100 beta induces apoptotic cell death in cultured astrocytes via a nitric oxide-dependent pathway. Biochim Biophys Acta 1313:239–245. https://doi.org/10.1016/0167-4889(96)00095-x
Kawata K, Liu CY, Merkel SF, Ramirez SH, Tierney RT, Langford D (2016) Blood biomarkers for brain injury: what are we measuring? Neurosci Biobehav Rev 68:460–473. https://doi.org/10.1016/j.neubiorev.2016.05.009
Hafner A, Obermajer N, Kos J (2012) gamma-Enolase C-terminal peptide promotes cell survival and neurite outgrowth by activation of the PI3K/Akt and MAPK/ERK signalling pathways. Biochem J 443:439–450. https://doi.org/10.1042/BJ20111351
Zheng J, Liang J, Deng X et al (2012) Mitogen activated protein kinase signaling pathways participate in the active principle region of Buyang Huanwu decoction-induced differentiation of bone marrow mesenchymal stem cells. Neural Regen Res 7:1370–1377
Sofroniew MV, Vinters HV (2010) Astrocytes: biology and pathology. Acta Neuropathol 119:7–35. https://doi.org/10.1007/s00401-009-0619-8
Kishimoto T (2010) IL-6: from its discovery to clinical applications. Int Immunol 22:347–352. https://doi.org/10.1093/intimm/dxq030
Romano M, Sironi M, Toniatti C et al (1997) Role of IL-6 and its soluble receptor in induction of chemokines and leukocyte recruitment. Immunity 6:315–325. https://doi.org/10.1016/s1074-7613(00)80334-9
Nakanishi M, Niidome T, Matsuda S, Akaike A, Kihara T, Sugimoto H (2007) Microglia-derived interleukin-6 and leukaemia inhibitory factor promote astrocytic differentiation of neural stem/progenitor cells. Eur J Neurosci 25:649–658. https://doi.org/10.1111/j.1460-9568.2007.05309.x
Di Pietro V, Amorini AM, Lazzarino G et al (2015) S100B and glial fibrillary acidic protein as indexes to monitor damage severity in an in vitro model of traumatic brain injury. Neurochem Res 40:991–999. https://doi.org/10.1007/s11064-015-1554-9
Li DR, Ishikawa T, Zhao D et al (2009) Histopathological changes of the hippocampus neurons in brain injury. Histol Histopathol 24:1113–1120. https://doi.org/10.14670/HH-24.1113
Petzold A, Keir G, Green AJ, Giovannoni G, Thompson EJ (2004) An ELISA for glial fibrillary acidic protein. J Immunol Methods 287:169–177. https://doi.org/10.1016/j.jim.2004.01.015
Frugier T, Morganti-Kossmann MC, O’Reilly D, McLean CA (2010) In situ detection of inflammatory mediators in post mortem human brain tissue after traumatic injury. J Neurotrauma 27:497–507. https://doi.org/10.1089/neu.2009.1120
Williams AJ, Wei HH, Dave JR, Tortella FC (2007) Acute and delayed neuroinflammatory response following experimental penetrating ballistic brain injury in the rat. J Neuroinflammation 4:17. https://doi.org/10.1186/1742-2094-4-17
Banks WA, Kastin AJ, Gutierrez EG (1994) Penetration of interleukin-6 across the murine blood-brain barrier. Neurosci Lett 179:53–56. https://doi.org/10.1016/0304-3940(94)90933-4
Raabe A, Kopetsch O, Gross U, Zimmermann M, Gebhart P (2003) Measurements of serum S-100B protein: effects of storage time and temperature on pre-analytical stability. Clin Chem Lab Med 41:700–703. https://doi.org/10.1515/CCLM.2003.106
Ramont L, Thoannes H, Volondat A, Chastang F, Millet MC, Maquart FX (2005) Effects of hemolysis and storage condition on neuron-specific enolase (NSE) in cerebrospinal fluid and serum: implications in clinical practice. Clin Chem Lab Med 43:1215–1217. https://doi.org/10.1515/CCLM.2005.210
Abdelhak A, Hottenrott T, Morenas-Rodriguez E et al (2019) Glial activation markers in CSF and serum from patients with primary progressive multiple sclerosis: potential of serum GFAP as disease severity marker? Front Neurol 10:280. https://doi.org/10.3389/fneur.2019.00280
Schwieler L, Larsson MK, Skogh E et al (2015) Increased levels of IL-6 in the cerebrospinal fluid of patients with chronic schizophrenia–significance for activation of the kynurenine pathway. J Psychiatry Neurosci 40:126–133. https://doi.org/10.1503/jpn.140126
Kenis G, Teunissen C, De Jongh R, Bosmans E, Steinbusch H, Maes M (2002) Stability of interleukin 6, soluble interleukin 6 receptor, interleukin 10 and CC16 in human serum. Cytokine 19:228–235
Rezaii PG, Grant GA, Zeineh MM et al (2019) Stability of blood biomarkers of traumatic brain injury. J Neurotrauma 36:2407–2416. https://doi.org/10.1089/neu.2018.6053
Ikeda Y, Umemura K (2005) Analysis of reference values of serum S100B concentrations of Japanese adults. Rinsho Byori 53:395–399
Garver DL, Tamas RL, Holcomb JA (2003) Elevated interleukin-6 in the cerebrospinal fluid of a previously delineated schizophrenia subtype. Neuropsychopharmacology 28:1515–1520. https://doi.org/10.1038/sj.npp.1300217
Fraser DD, Close TE, Rose KL et al (2011) Severe traumatic brain injury in children elevates glial fibrillary acidic protein in cerebrospinal fluid and serum. Pediatr Crit Care Med 12:319–324. https://doi.org/10.1097/PCC.0b013e3181e8b32d
Casmiro M, Maitan S, De Pasquale F et al (2005) Cerebrospinal fluid and serum neuron-specific enolase concentrations in a normal population. Eur J Neurol 12:369–374. https://doi.org/10.1111/j.1468-1331.2004.01021.x
Schindler CR, Lustenberger T, Woschek M et al (2020) Severe traumatic brain injury (TBI) modulates the kinetic profile of the inflammatory response of markers for neuronal damage. J Clin Med 9.https://doi.org/10.3390/jcm9061667
Lei J, Gao G, Feng J et al (2015) Glial fibrillary acidic protein as a biomarker in severe traumatic brain injury patients: a prospective cohort study. Crit Care 19:362. https://doi.org/10.1186/s13054-015-1081-8
Ferreira LC, Regner A, Miotto KD et al (2014) Increased levels of interleukin-6, -8 and -10 are associated with fatal outcome following severe traumatic brain injury. Brain Inj 28:1311–1316. https://doi.org/10.3109/02699052.2014.916818
Jaenicke R, Knof S (1968) Molecular weight and quaternary structure of lactic dehydrogenase. 3. Comparative determination by sedimentation analysis, light scattering and osmosis. Eur J Biochem 4:157–163. https://doi.org/10.1111/j.1432-1033.1968.tb00187.x
Worwood M (1990) Ferritin. Blood Rev 4:259–269. https://doi.org/10.1016/0268-960x(90)90006-e
Jungbluth S, Bailey K, Barde YA (1994) Purification and characterisation of a brain-derived neurotrophic factor/neurotrophin-3 (BDNF/NT-3) heterodimer. Eur J Biochem 221:677–685. https://doi.org/10.1111/j.1432-1033.1994.tb18780.x
Murer MG, Yan Q, Raisman-Vozari R (2001) Brain-derived neurotrophic factor in the control human brain, and in Alzheimer’s disease and Parkinson’s disease. Prog Neurobiol 63:71–124. https://doi.org/10.1016/s0301-0082(00)00014-9
Kjeldsen L, Johnsen AH, Sengelov H, Borregaard N (1993) Isolation and primary structure of NGAL, a novel protein associated with human neutrophil gelatinase. J Biol Chem 268:10425–10432
Farhana A, Lappin SL (2021) Biochemistry, Lactate Dehydrogenase. StatPearls Treasure Island, FL
Arosio P, Levi S (2002) Ferritin, iron homeostasis, and oxidative damage. Free Radic Biol Med 33:457–463. https://doi.org/10.1016/s0891-5849(02)00842-0
Liu HD, Li W, Chen ZR et al (2013) Increased expression of ferritin in cerebral cortex after human traumatic brain injury. Neurol Sci 34:1173–1180. https://doi.org/10.1007/s10072-012-1214-7
Dreyfus CF, Dai X, Lercher LD, Racey BR, Friedman WJ, Black IB (1999) Expression of neurotrophins in the adult spinal cord in vivo. J Neurosci Res 56:1–7. https://doi.org/10.1002/(SICI)1097-4547(19990401)56:1%3c1::AID-JNR1%3e3.0.CO;2-3
Lommatzsch M, Zingler D, Schuhbaeck K et al (2005) The impact of age, weight and gender on BDNF levels in human platelets and plasma. Neurobiol Aging 26:115–123. https://doi.org/10.1016/j.neurobiolaging.2004.03.002
Lommatzsch M, Braun A, Mannsfeldt A et al (1999) Abundant production of brain-derived neurotrophic factor by adult visceral epithelia. Implications for paracrine and target-derived Neurotrophic functions. Am J Pathol 155:1183–1193. https://doi.org/10.1016/S0002-9440(10)65221-2
Cowland JB, Borregaard N (1997) Molecular characterization and pattern of tissue expression of the gene for neutrophil gelatinase-associated lipocalin from humans. Genomics 45:17–23. https://doi.org/10.1006/geno.1997.4896
Kjeldsen L, Cowland JB, Borregaard N (2000) Human neutrophil gelatinase-associated lipocalin and homologous proteins in rat and mouse. Biochim Biophys Acta 1482:272–283. https://doi.org/10.1016/s0167-4838(00)00152-7
Zhao J, Chen H, Zhang M et al (2016) Early expression of serum neutrophil gelatinase-associated lipocalin (NGAL) is associated with neurological severity immediately after traumatic brain injury. J Neurol Sci 368:392–398. https://doi.org/10.1016/j.jns.2016.07.060
Lagana G, Barreca D, Calderaro A, Bellocco E (2019) Lactate dehydrogenase inhibition: biochemical relevance and therapeutical potential. Curr Med Chem 26:3242–3252. https://doi.org/10.2174/0929867324666170209103444
Cohen-Cory S, Kidane AH, Shirkey NJ, Marshak S (2010) Brain-derived neurotrophic factor and the development of structural neuronal connectivity. Dev Neurobiol 70:271–288. https://doi.org/10.1002/dneu.20774
Beatty WW, Monson N, Goodkin DE (1989) Access to semantic memory in Parkinson’s disease and multiple sclerosis. J Geriatr Psychiatry Neurol 2:153–162. https://doi.org/10.1177/089198878900200306
Alonso M, Vianna MR, Depino AM et al (2002) BDNF-triggered events in the rat hippocampus are required for both short- and long-term memory formation. Hippocampus 12:551–560. https://doi.org/10.1002/hipo.10035
Jha MK, Lee S, Park DH et al (2015) Diverse functional roles of lipocalin-2 in the central nervous system. Neurosci Biobehav Rev 49:135–156. https://doi.org/10.1016/j.neubiorev.2014.12.006
Giordano G, Hong S, Faustman EM, Costa LG (2011) Measurements of cell death in neuronal and glial cells. Methods Mol Biol 758:171–178. https://doi.org/10.1007/978-1-61779-170-3_11
Rao CJ, Shukla PK, Mohanty S, Reddy YJ (1978) Predictive value of serum lactate dehydrogenase in head injury. J Neurol Neurosurg Psychiatry 41:948–953. https://doi.org/10.1136/jnnp.41.10.948
Newell E, Shellington DK, Simon DW et al (2015) Cerebrospinal fluid markers of macrophage and lymphocyte activation after traumatic brain injury in children. Pediatr Crit Care Med 16:549–557. https://doi.org/10.1097/PCC.0000000000000400
Keir G, Tasdemir N, Thompson EJ (1993) Cerebrospinal fluid ferritin in brain necrosis: evidence for local synthesis. Clin Chim Acta 216:153–166. https://doi.org/10.1016/0009-8981(93)90148-w
Hicks RR, Numan S, Dhillon HS, Prasad MR, Seroogy KB (1997) Alterations in BDNF and NT-3 mRNAs in rat hippocampus after experimental brain trauma. Brain Res Mol Brain Res 48:401–406. https://doi.org/10.1016/s0169-328x(97)00158-7
Cuhadar S, Koseoglu M, Atay A, Dirican A (2013) The effect of storage time and freeze-thaw cycles on the stability of serum samples. Biochem Med (Zagreb) 23:70–77. https://doi.org/10.11613/bm.2013.009
Brinc D, Chan MK, Venner AA et al (2012) Long-term stability of biochemical markers in pediatric serum specimens stored at -80 degrees C: a CALIPER Substudy. Clin Biochem 45:816–826. https://doi.org/10.1016/j.clinbiochem.2012.03.029
Kang HJ, Jeon SY, Park JS et al (2013) Identification of clinical biomarkers for pre-analytical quality control of blood samples. Biopreserv Biobank 11:94–100. https://doi.org/10.1089/bio.2012.0051
Polyakova M, Schlogl H, Sacher J et al (2017) Stability of BDNF in human samples stored up to 6 months and correlations of serum and EDTA-plasma concentrations. Int J Mol Sci 18.https://doi.org/10.3390/ijms18061189
Wang J, Zhu HH, Xue JH, Wu SS, Chen Z (2015) Effects of storage conditions on the stability of serum CD163, NGAL, HMGB1 and MIP2. Int J Clin Exp Pathol 8:4099–4105
Pedersen KR, Ravn HB, Hjortdal VE, Norregaard R, Povlsen JV (2010) Neutrophil gelatinase-associated lipocalin (NGAL): validation of commercially available ELISA. Scand J Clin Lab Invest 70:374–382. https://doi.org/10.3109/00365513.2010.486868
Shimizu Y, Ichihara K (2019) Elucidation of stability profiles of common chemistry analytes in serum stored at six graded temperatures. Clin Chem Lab Med 57:1388–1396. https://doi.org/10.1515/cclm-2018-1109
Spencer BR, Brodsky JP, Holley GC, Foster GA, Winton C, Stramer SL (2019) Expanded feasibility of ferritin testing: stability of ferritin stored as whole blood and validation of plastic tubes. Transfusion 59:3424–3430. https://doi.org/10.1111/trf.15513
Sacri AS, Ferreira D, Khoshnood B, Gouya L, Barros H, Chalumeau M (2017) Stability of serum ferritin measured by immunoturbidimetric assay after storage at -80 degrees C for several years. PLoS ONE 12:e0188332. https://doi.org/10.1371/journal.pone.0188332
Bakay RA, Ward AA Jr (1983) Enzymatic changes in serum and cerebrospinal fluid in neurological injury. J Neurosurg 58:27–37. https://doi.org/10.3171/jns.1983.58.1.0027
Failla MD, Conley YP, Wagner AK (2016) Brain-derived neurotrophic factor (BDNF) in traumatic brain injury-related mortality: interrelationships between genetics and acute systemic and central nervous system BDNF profiles. Neurorehabil Neural Repair 30:83–93. https://doi.org/10.1177/1545968315586465
Petzold A, Worthington V, Appleby I, Kerr ME, Kitchen N, Smith M (2011) Cerebrospinal fluid ferritin level, a sensitive diagnostic test in late-presenting subarachnoid hemorrhage. J Stroke Cerebrovasc Dis 20:489–493. https://doi.org/10.1016/j.jstrokecerebrovasdis.2010.02.021
Simon D, Nicol JM, Sabino da Silva S et al (2015) Serum ferritin correlates with Glasgow coma scale scores and fatal outcome after severe traumatic brain injury. Brain Inj 29:612–617. https://doi.org/10.3109/02699052.2014.995228
Goedert M, Spillantini MG, Jakes R, Rutherford D, Crowther RA (1989) Multiple isoforms of human microtubule-associated protein tau: sequences and localization in neurofibrillary tangles of Alzheimer’s disease. Neuron 3:519–526. https://doi.org/10.1016/0896-6273(89)90210-9
Lei P, Ayton S, Finkelstein DI, Adlard PA, Masters CL, Bush AI (2010) Tau protein: relevance to Parkinson’s disease. Int J Biochem Cell Biol 42:1775–1778. https://doi.org/10.1016/j.biocel.2010.07.016
Guo T, Noble W, Hanger DP (2017) Roles of tau protein in health and disease. Acta Neuropathol 133:665–704. https://doi.org/10.1007/s00401-017-1707-9
Trojanowski JQ, Schuck T, Schmidt ML, Lee VM (1989) Distribution of tau proteins in the normal human central and peripheral nervous system. J Histochem Cytochem 37:209–215. https://doi.org/10.1177/37.2.2492045
Longnecker MP, Clapp RW, Sheahan K (1989) Associations between smoking status and stage of colorectal cancer at diagnosis in Massachusetts between 1982 and 1987. Cancer 64:1372–1374. https://doi.org/10.1002/1097-0142(19890915)64:6%3c1372::aid-cncr2820640633%3e3.0.co;2-i
Schoonenboom NS, Mulder C, Vanderstichele H et al (2005) Effects of processing and storage conditions on amyloid beta (1–42) and tau concentrations in cerebrospinal fluid: implications for use in clinical practice. Clin Chem 51:189–195. https://doi.org/10.1373/clinchem.2004.039735
Öst M, Nylen K, Csajbok L et al (2006) Initial CSF total tau correlates with 1-year outcome in patients with traumatic brain injury. Neurology 67:1600–1604. https://doi.org/10.1212/01.wnl.0000242732.06714.0f
Liliang PC, Liang CL, Weng HC et al (2010) Tau proteins in serum predict outcome after severe traumatic brain injury. J Surg Res 160:302–307. https://doi.org/10.1016/j.jss.2008.12.022
Andreasen N, Vanmechelen E, Van de Voorde A et al (1998) Cerebrospinal fluid tau protein as a biochemical marker for Alzheimer’s disease: a community based follow up study. J Neurol Neurosurg Psychiatry 64:298–305. https://doi.org/10.1136/jnnp.64.3.298
Maeda H, Zhu BL, Ishikawa T, Quan L, Michiue T (2009) Significance of postmortem biochemistry in determining the cause of death. Leg Med (Tokyo) 11(Suppl 1):S46–S49. https://doi.org/10.1016/j.legalmed.2009.01.048
O’Connell GC, Smothers CG, Winkelman C (2020) Bioinformatic analysis of brain-specific miRNAs for identification of candidate traumatic brain injury blood biomarkers. Brain Inj 34:965–974. https://doi.org/10.1080/02699052.2020.1764102
Bohnert S, Reinert C, Trella S, Schmitz W, Ondruschka B, Bohnert M (2021) Metabolomics in postmortem cerebrospinal fluid diagnostics: a state-of-the-art method to interpret central nervous system-related pathological processes. Int J Legal Med 135:183–191. https://doi.org/10.1007/s00414-020-02462-2
Szeremeta M, Pietrowska K, Niemcunowicz-Janica A, Kretowski A, Ciborowski M (2021) Applications of metabolomics in forensic toxicology and forensic medicine. Int J Mol Sci 22.https://doi.org/10.3390/ijms22063010
Ludwig N, Leidinger P, Becker K et al (2016) Distribution of miRNA expression across human tissues. Nucleic Acids Res 44:3865–3877. https://doi.org/10.1093/nar/gkw116
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zwirner, J., Kulakofsky, R., Fitzek, A. et al. Forensic biomarkers of lethal traumatic brain injury. Int J Legal Med 136, 871–886 (2022). https://doi.org/10.1007/s00414-022-02785-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00414-022-02785-2