Abstract
Background
As a biomarker of alveolar-capillary basement membrane injury, Krebs von den Lungen-6 (KL-6) is involved in the occurrence and development of pulmonary diseases. However, the role of the KL-6 in patients with acute exacerbation of chronic obstructive pulmonary disease (AECOPD) has yet to be elucidated. This prospective study was designed to clarify the associations of the serum KL-6 with the severity and prognosis in patients with AECOPD.
Methods
This study enrolled 199 eligible AECOPD patients. Demographic data and clinical characteristics were recorded. Follow-up was tracked to evaluate acute exacerbation and death. The serum KL-6 concentration was measured via an enzyme-linked immunosorbent assay.
Results
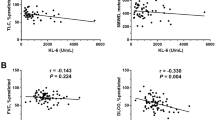
Serum KL-6 level at admission was higher in AECOPD patients than in control subjects. The serum KL-6 concentration gradually elevated with increasing severity of AECOPD. Pearson and Spearman analyses revealed that the serum KL-6 concentration was positively correlated with the severity score, monocyte count and concentrations of C-reactive protein, interleukin-6, uric acid, and lactate dehydrogenase in AECOPD patients during hospitalization. A statistical analysis of long-term follow-up data showed that elevated KL-6 level at admission was associated with longer hospital stays, an increased risk of future frequent acute exacerbations, and increased severity of exacerbation in COPD patients.
Conclusion
Serum KL-6 level at admission is positively correlated with increased disease severity, prolonged hospital stay and increased risk of future acute exacerbations in COPD patients. There are positive dose–response associations of elevated serum KL-6 with severity and poor prognosis in COPD patients. The serum KL-6 concentration could be a novel diagnostic and prognostic biomarker in AECOPD patients.



Similar content being viewed by others
References
Song Q, Lin L, Zhou A et al (2023) The effects of different inhalation therapies on less symptomatic chronic obstructive pulmonary disease patients in a Chinese population: a real-world study. Ann Med 55(1):1317–1324. https://doi.org/10.1080/07853890.2023.2192519
Wang C, Xu J, Yang L et al (2018) Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China Pulmonary Health [CPH] study): a national cross-sectional study. Lancet 391(10131):1706–1717. https://doi.org/10.1016/S0140-6736(18)30841-9
Zhou M, Wang H, Zeng X et al (2019) Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 394(10204):1145–1158. https://doi.org/10.1016/S0140-6736(19)30427-1
Lou P, Zhu Y, Chen P et al (2012) Vulnerability, beliefs, treatments and economic burden of chronic obstructive pulmonary disease in rural areas in China: a cross-sectional study. BMC Public Health. https://doi.org/10.1186/1471-2458-12-287
Boers E, Barrett M, Su JG et al (2023) Global burden of chronic obstructive pulmonary disease through 2050. JAMA Netw Open 6(12):e2346598. https://doi.org/10.1001/jamanetworkopen.2023.46598
Crapo RO (1994) Pulmonary-function testing. N Engl J Med 331(1):25–30. https://doi.org/10.1056/NEJM199407073310107
Xiao C, Cheng S, Li R et al (2021) Isoforskolin alleviates AECOPD by improving pulmonary function and attenuating inflammation which involves downregulation of Th17/IL-17A and NF-κB/NLRP3. Front Pharmacol. https://doi.org/10.3389/fphar.2021.721273
Weber B, Sturm R, Henrich D et al (2023) Diagnostic and prognostic potential of exosomal cytokines IL-6 and IL-10 in polytrauma patients. Int J Mol Sci 24(14):11830. https://doi.org/10.3390/ijms241411830
Vitacca M, Malovini A, Paneroni M et al (2024) Predicting response to in-hospital pulmonary rehabilitation in individuals recovering from exacerbations of chronic obstructive pulmonary disease. Arch Bronconeumol 60(3):153–160. https://doi.org/10.1016/j.arbres.2024.01.001
Lee HW, Lee JK, Hwang YI et al (2024) Spirometric interpretation and clinical relevance according to different reference equations. J Korean Med Sci. https://doi.org/10.3346/jkms.2024.39.e20
Chung C, Lee JW, Lee SW et al (2024) Clinical efficacy of mobile app-based, self-directed pulmonary rehabilitation for patients with chronic obstructive pulmonary disease: systematic review and meta-analysis. JMIR Mhealth Uhealth 12:e41753. https://doi.org/10.2196/41753
Ishikawa N, Hattori N, Yokoyama A et al (2012) Utility of KL-6/MUC1 in the clinical management of interstitial lung diseases. Respir Investig 50(1):3–13. https://doi.org/10.1016/j.resinv.2012.02.001
Guan X, Zhao B, Guan X et al (2023) A benzochalcone derivative synchronously induces apoptosis and ferroptosis in pancreatic cancer cells. PeerJ. https://doi.org/10.7717/peerj.16291
Endo S, Nishimura N, Kawano Y et al (2018) MUC1/KL-6 expression confers an aggressive phenotype upon myeloma cells. Biochem Biophys Res Commun 507(1–4):246–252. https://doi.org/10.1016/j.bbrc.2018.11.016
Park HK, Yoon CS, Na YO et al (2023) Serum KL-6 levels predict the occurrence and severity of treatment-related interstitial lung disease in lung cancer. Sci Rep. https://doi.org/10.1038/s41598-023-45170-8
Fields A, Potel KN, Cabuhal R et al (2023) Mediators of systemic sclerosis-associated interstitial lung disease (SSc-ILD): systematic review and meta-analyses. Thorax 78(8):799–807. https://doi.org/10.1136/thorax-2022-219226
Wang Y, Chen S, Zheng S et al (2021) The role of lung ultrasound B-lines and serum KL-6 in the screening and follow-up of rheumatoid arthritis patients for an identification of interstitial lung disease: review of the literature, proposal for a preliminary algorithm, and clinical application to cases. Arthritis Res Ther. https://doi.org/10.1186/s13075-021-02586-9
Sokai A, Tanizawa K, Handa T et al (2017) Importance of serial changes in biomarkers in idiopathic pulmonary fibrosis. ERJ Open Res 3(3):00019–02016. https://doi.org/10.1183/23120541.00019-2016
Bessa V, Bonella F, Ohshimo S et al (2019) Changes in serum KL-6 levels are associated with the development of chronic lung allograft dysfunction in lung transplant recipients. Transpl Immunol 52:40–44. https://doi.org/10.1016/j.trim.2018.10.006
d’Alessandro M, Cameli P, Refini RM et al (2020) Serum KL-6 concentrations as a novel biomarker of severe COVID-19. J Med Virol 92(10):2216–2220. https://doi.org/10.1002/jmv.26087
d’Alessandro M, Bergantini L, Cameli P et al (2021) Serum concentrations of KL-6 in patients with IPF and lung cancer and serial measurements of KL-6 in IPF patients treated with antifibrotic therapy. Cancers (Basel) 13(4):689. https://doi.org/10.3390/cancers13040689
Cheng W, Zhou A, Zeng Y et al (2023) Prediction of hospitalization and mortality in patients with chronic obstructive pulmonary disease with the new global initiative for chronic obstructive lung disease 2023 group classification: a prospective cohort and a retrospective analysis. Int J Chron Obstruct Pulmon Dis 18:2341–2352. https://doi.org/10.2147/COPD.S429104
Agustí A, Celli BR, Criner GJ et al (2023) Global initiative for chronic obstructive lung disease 2023 report: GOLD executive summary. Am J Respir Crit Care Med 207(7):819–837. https://doi.org/10.1164/rccm.202301-0106PP
Zheng L, Fei J, Feng CM et al (2021) Serum 8-iso-PGF2α predicts the severity and prognosis in patients with community-acquired pneumonia: a retrospective cohort study. Front Med (Lausanne). https://doi.org/10.3389/fmed.2021.633442
Fei J, Fu L, Cao W et al (2019) Low vitamin D status is associated with epithelial-mesenchymal transition in patients with chronic obstructive pulmonary disease. J Immunol 203(6):1428–1435. https://doi.org/10.4049/jimmunol.1900229
Xu Z, Wang XM, Cao P et al (2022) Serum IL-27 predicts the severity and prognosis in patients with community-acquired pneumonia: a prospective cohort study. Int J Med Sci 19(1):74–81. https://doi.org/10.7150/ijms.67028
Feng CM, Cheng JY, Xu Z et al (2021) Associations of serum resistin with the severity and prognosis in patients with community-acquired pneumonia. Front Immunol. https://doi.org/10.3389/fimmu.2021.703515
Fu L, Chen YH, Bo QL et al (2019) Lipopolysaccharide downregulates 11β-hydroxysteroid dehydrogenase 2 expression through inhibiting peroxisome proliferator-activated receptor-γ in placental trophoblasts. J Immunol 203(5):1198–1207. https://doi.org/10.4049/jimmunol.1900132
Fu L, Zhao H, Xiang Y et al (2021) Reactive oxygen species-evoked endoplasmic reticulum stress mediates 1-nitropyrene-induced epithelial-mesenchymal transition and pulmonary fibrosis. Environ Pollut. https://doi.org/10.1016/j.envpol.2021.117134
Ohnishi H, Yokoyama A, Kondo K et al (2002) Comparative study of KL-6, surfactant protein-A, surfactant protein-D, and monocyte chemoattractant protein-1 as serum markers for interstitial lung diseases. Am J Respir Crit Care Med 165(3):378–381. https://doi.org/10.1164/ajrccm.165.3.2107134
Oyama T, Kohno N, Yokoyama A et al (1997) Detection of interstitial pneumonitis in patients with rheumatoid arthritis by measuring circulating levels of KL-6, a human MUC1 mucin. Lung 175(6):379–385. https://doi.org/10.1007/pl00007584
Nathani N, Perkins GD, Tunnicliffe W et al (2008) Kerbs von Lungren 6 antigen is a marker of alveolar inflammation but not of infection in patients with acute respiratory distress syndrome. Crit Care 12(1):R12. https://doi.org/10.1186/cc6785
Ishikawa N, Hattori N, Kohno N et al (2015) Airway inflammation in Japanese COPD patients compared with smoking and nonsmoking controls. Int J Chron Obstruct Pulmon Dis. https://doi.org/10.2147/COPD.S74557
Kwok WC, Tam TCC, Ho JCM et al (2024) Hospitalized acute exacerbation in chronic obstructive pulmonary disease - impact on long-term renal outcomes. Respir Res. https://doi.org/10.1186/s12931-023-02635-8
Liu H, Xie Y, Huang Y et al (2024) The association between blood eosinophils and clinical outcome of acute exacerbations of chronic obstructive pulmonary disease: a systematic review and meta-analysis. Respir Med 222:107501. https://doi.org/10.1016/j.rmed.2023.107501
Vogelmeier C, Anzueto A, & Barnes P (2020) The global strategy for diagnosis, management and prevention of COPD 2021 UPDATE.GOLD science committee members.
Vianello A, Guarnieri G, Achille A et al (2023) Serum biomarkers of remodeling in severe asthma with fixed airway obstruction and the potential role of KL-6. Clin Chem Lab Med 61(10):1679–1687. https://doi.org/10.1515/cclm-2022-1323
Kambe M, Ohshimo S, Kohno N (2007) Immunity tests for respiratory diseases--SP-A, SP-D, KL-6. Rinsho Byori 55(4):381–387
Brightling C, Greening N (2019) Airway inflammation in COPD: progress to precision medicine. Eur Respir J 54(2):1900651. https://doi.org/10.1183/13993003.00651-2019
Barnes PJ (2017) Cellular and molecular mechanisms of asthma and COPD. Clin Sci 131(13):1541–1558. https://doi.org/10.1042/CS20160487
Funding
This work was supported by the National Natural Science Foundation of China (82100078, 82270071), Anhui Provincial Clinical Research Transformation Project (202204295107020014, 202204295107020056), Research Funds of Center for Big Data and Population Health of IHM (JKS2022007), the Scientific Research of Health Commission in Anhui Province (AHWJ2021b091) and the University Natural Science Research Project of Anhui Province (2023AH030117), Anhui Medical University Foundation (2021xkj159), Talent Project of Colleges and Universities in Anhui Province (gxyp2021169) and National Natural Science Foundation Incubation Program of the Second Affiliated Hospital of Anhui Medical University (2019GQFY06).
Author information
Authors and Affiliations
Contributions
LF, HZ, and JY contributed to its design and conception. YW, and JF drafted the manuscript. JX, Z-YC, Y-CM, and J-HW contributed to study design and carried out the studies. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare no competing interests.
Ethical Approval
This study was performed in compliance with the Declaration of Helsinki and was approved by the Ethics Committee of the Second Affiliated Hospital of Anhui Medical University (YX2021-146).
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, Y., Fei, J., Xu, J. et al. Associations of the Serum KL-6 with Severity and Prognosis in Patients with Acute Exacerbation of Chronic Obstructive Pulmonary Disease. Lung 202, 245–255 (2024). https://doi.org/10.1007/s00408-024-00702-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-024-00702-5