Abstract
Introduction
Previously described methodologies for detecting laryngopharyngeal reflux (LPR) have limitations. Symptoms alone are non-diagnostic, and pH-impedance studies have poor sensitivity. Pulmonary micro-aspiration is under-recognised in LPR and gastro-esophageal reflux disease (GERD). The present study aimed to describe the results of a modified technique for scintigraphic reflux studies in two groups with severe reflux: those with typical reflux symptoms and those with laryngopharyngeal manifestations of reflux.
Methods
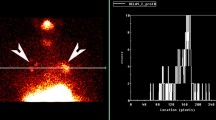
A prospective database of severely symptomatic, treatment-resistant reflux patients was grouped based upon predominant symptom profile of typical GERD or LPR. All patients underwent reflux scintigraphy. Results were obtained for early scintigraphic reflux contamination of the pharynx and proximal esophagus, and delayed contamination of the pharynx and lungs after 2 h.
Results
187 patients were studied (82 GERD, 105 LPR). The LPR patients were predominantly female (70.5% vs. 56.1%; p = 0.042) and older than the GERD group (median age 60 years vs. 55.5 years; p = 0.002). Early scintigraphic reflux was seen at the pharynx in 89.2% (GERD 87.7%, LPR 90.4%; p = 0.133), and at the proximal esophagus in 89.7% (GERD 88.9%, LPR 90.4%; p = 0.147). Delayed contamination of the pharynx was seen in 95.2% (GERD 93.9%, LPR 96.2%; p = 0.468). Delayed pulmonary aspiration was seen in 46% (GERD 36.6%, LPR 53.3%; p = 0.023).
Conclusion
Reflux scintigraphy demonstrated a high rate of reflux-related pulmonary aspiration. Contamination of the proximal esophagus and pharynx was observed frequently in both groups of severe disease. The likelihood of pulmonary aspiration and potential pulmonary disease needs to be entertained in severe GERD and LPR.


Similar content being viewed by others
References
Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R, The Global Consensus Group (2006) The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol 10(8):1900–1920. https://doi.org/10.1111/j.1572-0241.2006.00630.x
Houghton LA, Lee AS, Badri H, DeVault KR, Smith JA (2016) Respiratory disease and the oesophagus: reflux, reflexes and microaspiration. Nat Rev Gastroenterol Hepatol 13(8):445–460. https://doi.org/10.1038/nrgastro.2016.91
Lee BE et al (2010) Combined dual channel impedance/pH-metry in patients with suspected laryngopharyngeal reflux. J Neurogastroenterol Motil 16(2):157–165. https://doi.org/10.5056/jnm.2010.16.2.157
Harrell SP, Koopman J, Woosley S, Wo JM (2007) Exclusion of pH artifacts is essential for hypopharyngeal pH monitoring. Laryngoscope 117(3):470–474. https://doi.org/10.1097/MLG.0b013e31802d344c
Zerbib F et al (2013) Normal values of pharyngeal and esophageal 24-hour pH impedance in individuals on and off therapy and interobserver reproducibility. Clin Gastroenterol Hepatol 11(4):366–372. https://doi.org/10.1016/j.cgh.2012.10.041
Ummarino D, Vandermeulen L, Roosens B, Urbain D, Hauser B, Vandenplas Y (2013) Gastroesophageal reflux evaluation in patients affected by chronic cough: restech versus multichannel intraluminal impedance/pH metry. Laryngoscope 123(4):980–984. https://doi.org/10.1002/lary.23738
Khoma O, Burton L, Falk MG, Van der Wall H, Falk GL (2020) Predictors of reflux aspiration and laryngo-pharyngeal reflux. Esophagus 17(3):355–362. https://doi.org/10.1007/s10388-020-00726-9
Ruth M, Carlsson S, Månsson I, Bengtsson U, Sandberg N (1993) Scintigraphic detection of gastro-pulmonary aspiration in patients with respiratory disorders. Clin Physiol 13(1):19–33. https://doi.org/10.1111/j.1475-097X.1993.tb00314.x
Burton L, Falk GL, Parsons S, Cusi M, Van Der Wall H (2018) Benchmarking of a simple scintigraphic test for gastro-oesophageal reflux disease that assesses oesophageal disease and its pulmonary complications. Mirt 27(3):113–120. https://doi.org/10.4274/mirt.10438
Burton L, Falk GL, Beattie J, Novakovic D, Simpson S, Van der Wall H (2020) Findings from a novel scintigraphic gastroesophageal reflux study in asymptomatic volunteers. Am J Nucl Med Mol Imaging 10(6):342–348
Falk GL (2015) Scintigraphy in laryngopharyngeal and gastroesophageal reflux disease: a definitive diagnostic test? WJG 21(12):3619. https://doi.org/10.3748/wjg.v21.i12.3619
Lechien JR et al (2019) Evaluation and management of laryngopharyngeal reflux disease: state of the art review. Otolaryngol Head Neck Surg 160(5):762–782. https://doi.org/10.1177/0194599819827488
Amarasiri DL, Pathmeswaran A, de Silva HJ, Ranasinha CD (2013) Response of the airways and autonomic nervous system to acid perfusion of the esophagus in patients with asthma: a laboratory study. BMC Pulm Med 13(1):33. https://doi.org/10.1186/1471-2466-13-33
Belafsky PC, Postma GN, Koufman JA (2001) The validity and reliability of the reflux finding score (RFS). Laryngoscope 111(8):1313–1317. https://doi.org/10.1097/00005537-200108000-00001
Milstein CF, Charbel S, Hicks DM, Abelson TI, Richter JE, Vaezi MF (2005) Prevalence of laryngeal irritation signs associated with reflux in asymptomatic volunteers: impact of endoscopic technique (rigid vs. flexible laryngoscope). Laryngoscope 115(12):2256–2261. https://doi.org/10.1097/01.mlg.0000184325.44968.b1
Chen M, Hou C, Chen T, Lin Z, Wang X, Zeng Y (2018) Reflux symptom index and reflux finding score in 91 asymptomatic volunteers. Acta Otolaryngol 138(7):659–663. https://doi.org/10.1080/00016489.2018.1436768
Hicks DM, Ours TM, Abelson TI, Vaezi MF, Richter JE (2002) The prevalence of hypopharynx findings associated with gastroesophageal reflux in normal volunteers. J Voice 16(4):564–579. https://doi.org/10.1016/S0892-1997(02)00132-7
Branski RC, Bhattacharyya N, Shapiro J (2002) The reliability of the assessment of endoscopic laryngeal findings associated with laryngopharyngeal reflux disease. Laryngoscope 112(6):1019–1024. https://doi.org/10.1097/00005537-200206000-00016
Anandasabapathy S, Jaffin BW (2006) Multichannel intraluminal impedance in the evaluation of patients with persistent globus on proton pump inhibitor therapy. Ann Otol Rhinol Laryngol 115(8):563–570
Bestetti A, Carola F, Carnevali-Ricci P, Sambataro G, Tarolo GL (2000) 99mTc-sulfur colloid gastroesophageal scintigraphy with late lung imaging to evaluate patients with posterior laryngitis. J Nucl Med 41(10):1597–1602
Galli J, Volante M, Parrilla C, Rigante M, Valenza V (2005) Oropharyngoesophageal scintigraphy in the diagnostic algorithm of laryngopharyngeal reflux disease: a useful exam? Otolaryngol Head Neck Surg 132(5):717–721. https://doi.org/10.1016/j.otohns.2005.01.043
Fass R (2002) Functional heartburn: the stimulus, the pain, and the brain. Gut 51(6):885–892. https://doi.org/10.1136/gut.51.6.885
Trimble KC, Pryde A, Heading RC (1995) Lowered oesophageal sensory thresholds in patients with symptomatic but not excess gastro-oesophageal reflux: evidence for a spectrum of visceral sensitivity in GORD. Gut 37(1):7–12. https://doi.org/10.1136/gut.37.1.7
Koufman JA, Amin MR, Panetti M (2000) Prevalence of reflux in 113 consecutive patients with laryngeal and voice disorders. Otolaryngol Head Neck Surg 123(4):385–388. https://doi.org/10.1067/mhn.2000.109935
Lin M, Gerson LB, Lascar R, Davila M, Triadafilopoulos G (2004) Features of gastroesophageal reflux disease in women. Off J Am Coll Gastroenterol 99(8):1442–1447
Funding
The authors have no relevant financial or non-financial interests to disclose.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Park, Js., Burton, L., Van der Wall, H. et al. Modified Reflux Scintigraphy Detects Pulmonary Microaspiration in Severe Gastro-Esophageal and Laryngopharyngeal Reflux Disease. Lung 199, 139–145 (2021). https://doi.org/10.1007/s00408-021-00432-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-021-00432-y