Abstract
Introduction
The main goal of the present study was the development of a survival scoring system for patients treated with stereotactic body radiation therapy (SBRT) for very few lung metastases. Such an instrument would be of value when selecting the optimal dose for individual patients with a limited number of pulmonary lesions.
Methods
Forty-six patients receiving SBRT for 1–3 lung metastases were retrospectively analyzed. The biologically effective dose plus nine characteristics [gender, age, performance score, interval from tumor diagnosis to SBRT, primary tumor type, additional (extra-pulmonary) metastases, major location of lung metastases, number of pulmonary lesions, and volume treated with SBRT] were evaluated. Characteristics significantly associated with the survival on Cox regression analysis were incorporated in the scoring system. Scoring points were received from 1-year survival rates divided by 10. Sums of these scoring points represented the scores for the individual patients.
Results
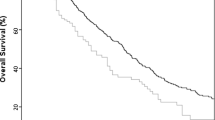
Survival rates at 1 and 2 years were 66 and 56 %, respectively. On Cox regression analysis, performance score (p = 0.025), the type of primary tumor (p = 0.013) and the additional metastases (p = 0.032) had a significant impact on survival. Scores for patients ranged from 15 to 25 points. Three groups were designed: 15 points, 16–20 points, and 21–25 points. One-year survival rates were 0, 52, and 83 %, respectively (p = 0.005); 2-year survival rates were 0, 52, and 66 %, respectively.
Conclusion
A survival scoring system for patients receiving SBRT for very few lung metastases was developed. This score allowed us to estimate the survival prognosis of these patients and can aid physicians when aiming to choose the optimal SBRT dose for individual patients.


Similar content being viewed by others
References
Ashworth AB, Senan S, Palma DA et al (2014) An individual patient data metaanalysis of outcomes and prognostic factors after treatment of oligometastatic non-small-cell lung cancer. Clin Lung Cancer 15:346–355
Scorsetti M, Clerici E, Navarria P et al (2015) The role of stereotactic body radiation therapy (SBRT) in the treatment of oligometastatic disease in the elderly. Br J Radiol 88:20150111
De Rose F, Cozzi L, Navarria P et al (2016) Clinical outcome of stereotactic ablative body radiotherapy for lung metastatic lesions in non-small cell lung cancer oligometastatic patients. Clin Oncol (R Coll Radiol) 28:13–20
García-Cabezas S, Bueno C, Rivin E et al (2015) Lung metastases in oligometastatic patients: outcome with stereotactic body radiation therapy (SBRT). Clin Transl Oncol 17:668–672
Wang Z, Kong QT, Li J et al (2015) Clinical outcomes of cyberknife stereotactic radiosurgery for lung metastases. J Thorac Dis 7:407–412
Frakulli R, Salvi F, Balestrini D et al (2015) Stereotactic radiotherapy in the treatment of lung metastases from bone and soft-tissue sarcomas. Anticancer Res 35:5581–5586
Carvajal C, Navarro-Martin A, Cacicedo J et al (2015) Stereotactic body radiotherapy for colorectal lung oligometastases: preliminary single-institution results. J BUON 20:158–165
Hayes JT, David EA, Qi L et al (2015) Risk of pneumonitis after stereotactic body radiation therapy in patients with previous anatomic lung resection. Clin Lung Cancer 16:379–384
Janssen S, Kaesmann L, Rudat V et al (2016) Stereotactic body radiotherapy (SBRT) with lower doses for selected patients with stage I non-small-cell lung cancer (NSCLC). Lung 194:291–294
Joiner MC, Van der Kogel AJ (1997) The linear-quadratic approach to fractionation and calculation of isoeffect relationships. In: Steel GG (ed) Basic clinical radiobiology. Oxford University Press, New York, pp 106–112
Rades D, Douglas S, Veninga T et al (2010) Validation and simplification of a score predicting survival in patients irradiated for metastatic spinal cord compression. Cancer 116:3670–3673
Dziggel L, Segedin B, Podvrsnik NH et al (2013) Validation of a survival score for patients treated with whole-brain radiotherapy for brain metastases. Strahlenther Onkol 189:364–666
Qiu H, Katz AW, Chowdhry AK et al (2015) Stereotactic body radiotherapy for lung metastases from colorectal cancer: prognostic factors for disease control and survival. Am J Clin Oncol, in press, PMID: 26270442
Fode MM, Høyer M (2015) Survival and prognostic factors in 321 patients treated with stereotactic body radiotherapy for oligo-metastases. Radiother Oncol 114:155–160
Kress MA, Collins BT, Collins SP et al (2012) Scoring system predictive of survival for patients undergoing stereotactic body radiation therapy for liver tumors. Radiat Oncol 7:148
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Janssen, S., Kaesmann, L., Rudat, V. et al. A scoring system for predicting the survival prognosis of patients receiving stereotactic body radiation therapy (SBRT) for 1–3 lung metastases. Lung 194, 631–635 (2016). https://doi.org/10.1007/s00408-016-9906-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-016-9906-z