Abstract
Purpose
The aim of this study was to evaluate prognostic factors in patients with lung metastases who undergo lung stereotactic body radiotherapy (SBRT).
Materials and methods
A total of 87 patients with 129 lung metastases who underwent SBRT between November 2004 and May 2012 were enrolled in this retrospective study. The patient collective consisted of 54 men (62.1%) and 33 women (37.9%); the median age was 65 years (range 36–88). The Karnofsky performance index was ≥70% (median 90%) for all cases, but one (60%). Adverse effects were categorized using the CTCAE 4.0 classification system. Retrospective analyses regarding patients’ characteristics, progression-free survival (PFS), overall survival (OS), disease-specific survival (DSS), and local tumor control rates (LTC) were performed.
Results
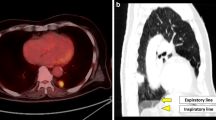
On univariate and multivariate analysis OS, DSS, and PFS were significantly (p < 0.05) better for patients with ≤3 lung metastases; no extrathoracic metastases at the time of the SBRT; a gross tumor volume (GTV) <7.7 cm3 and patients that received a staging that included positron emission tomography with fluorine 18 fluorodeoxyglucose/computed tomography (FDG-PET/CT) imaging. Furthermore, a longer OS was observed if newly diagnosed metastases during follow-up were limited to the lung (median survival: 43.7 months versus 21.7 months; p = 0.023).
Conclusion
The number and pattern of metastases, and the size of the target volume are strong predictors for the outcome of patients receiving SBRT of lung tumors. FDG-PET/CT should be part of pretherapeutic staging before SBRT.
Zusammenfassung
Hintergrund
Ziel dieser Studie war es, prognostische Faktoren bei Patienten mit Lungenmetastasen zu evaluieren, die mit einer stereotaktischen Strahlentherapie (SBRT) behandelt wurden.
Material und Methoden
In dieser retrospektiven Studie wurden 87 Patienten mit insgesamt 129 Lungenmetastasen, die zwischen November 2004 und Mai 2012 in unserem Institut mit einer SBRT behandelt wurden, untersucht. Das Patientenkollektiv setzte sich aus 54 Männern (62,1%) und 33 Frauen (37,9%) zusammen; das mediane Alter betrug 65 Jahre (Spanne 36–88 Jahre). Mit einer Ausnahme (60%) war der Karnofsky-Index ≥70% (median 90%). Die Nebenwirkungen wurden entsprechend CTCAE V. 4.0. klassifiziert. Das progressionsfreie Überleben (PFÜ), das Gesamtüberleben (GÜ), das krankheitsspezifische Überleben (KSÜ) und die lokale Tumorkontrolle (LTK) wurden unter Berücksichtigung prognostischer Einflussfaktoren analysiert.
Ergebnisse
Patienten mit maximal 3 Lungenmetastasen ohne extrathorakale Metastasierung mit einem Gesamttumorvolumen (GTV) <7,7 cm3 und Patienten, die ein Staging mittels FDG-PET (18 Fluordesoxyglukose-Positronenemissionstomographie) vor Beginn der Behandlung erhalten hatten, zeigten ein signifikant längeres GÜ, PFÜ und KSÜ. Des Weiteren wurde für Patienten, bei denen neue Metastasen während des Follow-ups auf die Lunge begrenzt waren, ein längeres GÜ verzeichnet (median: 43,7 Monate vs. 21,7 Monate; p = 0,023)
Schlussfolgerung
Die Anzahl der Metastasen, das Metastasierungsmuster und die Größe des Zielvolumens sind wesentliche Prädiktoren hinsichtlich der Prognose bei der SBRT von Lungentumoren. Ein FDG-PET ist ein wichtiger Bestandteil des prätherapeutischen Stagings vor SBRT.



Similar content being viewed by others
References
Saito Y et al (2002) Pulmonary metastasectomy for 165 patients with colorectal carcinoma: a prognostic assessment. J Thorac Cardiovasc Surg 124(5):1007–1013
Pfannschmidt J et al (2003) Prognostic factors and survival after complete resection of pulmonary metastases from colorectal carcinoma: experiences in 167 patients. J Thorac Cardiovasc Surg 126(3):732–739
Corbin KS, Hellman S, Weichselbaum RR (2013) Extracranial oligometastases: a subset of metastases curable with stereotactic radiotherapy. J Clin Oncol 31(11):1384–1390
Rusthoven KE et al (2009) Multi-institutional phase I/II trial of stereotactic body radiation therapy for lung metastases. J Clin Oncol 27(10):1579–1584
Stera S et al (2017) Breathing-motion-compensated robotic guided stereotactic body radiation therapy. Patterns of failure analysis. Strahlenther Onkol 194(2):143–155
Wulf J et al (2005) Dose-response in stereotactic irradiation of lung tumors. Radiother Oncol 77(1):83–87
Hof H et al (2007) Stereotactic single-dose radiotherapy of lung metastases. Strahlenther Onkol 183(12):673–678
De Rose F et al (2016) Clinical outcome of stereotactic ablative body radiotherapy for lung metastatic lesions in non-small cell lung cancer oligometastatic patients. Clin Oncol (R Coll Radiol) 28(1):13–20
Rieber J et al (2017) Influence of institutional experience and technological advances on outcome of stereotactic body radiation therapy for oligometastatic lung disease. Int J Radiat Oncol Biol Phys 98(3):511–520
Tanadini-Lang S et al (2017) Nomogram based overall survival prediction in stereotactic body radiotherapy for oligo-metastatic lung disease. Radiother Oncol 123(2):182–188
Navarria P et al (2014) Stereotactic body radiotherapy (sbrt) in lung oligometastatic patients: role of local treatments. Radiat Oncol 9(1):91
Okunieff P et al (2006) Stereotactic Body Radiation Therapy (SBRT) for lung metastases. Acta Oncol 45(7):808–817
Ricardi U et al (2012) Stereotactic body radiation therapy for lung metastases. Lung Cancer 75(1):77–81
Nuyttens JJ et al (2015) Stereotactic body radiation therapy for oligometastases to the lung: a phase 2 study. Int J Radiat Oncol Biol Phys 91(2):337–343
Onishi H et al (2004) Stereotactic hypofractionated high-dose irradiation for stage I nonsmall cell lung carcinoma: clinical outcomes in 245 subjects in a Japanese multiinstitutional study. Cancer 101(7):1623–1631
Norihisa Y et al (2008) Stereotactic body radiotherapy for oligometastatic lung tumors. Int J Radiat Oncol Biol Phys 72(2):398–403
Inoue T et al (2013) Stereotactic body radiotherapy for pulmonary metastases. Prognostic factors and adverse respiratory events. Strahlenther Onkol 189(4):285–292
Tree AC et al (2013) Stereotactic body radiotherapy for oligometastases. Lancet Oncol 14(1):e28–e37
Salama JK et al (2012) Stereotactic body radiotherapy for multisite extracranial oligometastases: final report of a dose escalation trial in patients with 1 to 5 sites of metastatic disease. Cancer 118(11):2962–2970
Zhang Y et al (2011) Stereotactic body radiation therapy favors long-term overall survival in patients with lung metastases: five-year experience of a single-institution. Chin Med J (Engl) 124(24):4132–4137
Kang JK et al (2010) Oligometastases confined one organ from colorectal cancer treated by SBRT. Clin Exp Metastasis 27(4):273–278
Thibault I et al (2014) Predictive factors for local control in primary and metastatic lung tumours after four to five fraction stereotactic ablative body radiotherapy: a single institution’s comprehensive experience. Clin Oncol (R Coll Radiol) 26(11):713–719
Dhami G et al (2017) Framework for radiation pneumonitis risk stratification based on anatomic and perfused lung dosimetry. Strahlenther Onkol 193(5):410–418
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
K.J. Borm, M. Oechsner, K. Schiller, J.C. Peeken, H. Dapper, S. Münch, L. Kroll, S.E. Combs and M.N. Duma declare that they have no competing interests.
Ethical standards
The ethics committee of the Technical University Munich approved this retrospective study (84/16S). All patients gave their informed consent both informed and written before starting the radiotherapy that they will undergo CT radiotherapy treatment planning. Data from the CT radiotherapy treatment planning were retrospectively analyzed.
Rights and permissions
About this article
Cite this article
Borm, K.J., Oechsner, M., Schiller, K. et al. Prognostic factors in stereotactic body radiotherapy of lung metastases. Strahlenther Onkol 194, 886–893 (2018). https://doi.org/10.1007/s00066-018-1335-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-018-1335-x