Abstract
The objective of this study was to document persistent pulmonary symptoms and pulmonary function abnormalities in adults surviving hantavirus pulmonary syndrome (HPS). Acute infection by most hantaviruses result in mortality rates of 25–35%, while in Panama the mortality rate of 10% is contrasted by an unusually high incidence. In all types of HPS, the viral prodrome, cardiopulmonary phase due to massive pulmonary capillary leak syndrome, and spontaneous diuresis are followed by a convalescent phase with exertional dyspnea for 3–4 weeks, but the frequency of persistent symptoms is not known. In this observational study of a convenience sample, 14 survivors of HPS caused by Choclo virus infection in Panama and 9 survivors of HPS caused by Sin Nombre virus infection in New Mexico completed a questionnaire and pulmonary function tests up to 8 years after infection. In both groups, exertional dyspnea persisted for 1–2 years after acute infection in 43% (Panama) and 77% (New Mexico) of survivors surveyed. Reduction in midexpiratory flows (FEF25–75%), increased residual volume (RV), and reduced diffusion capacity (DLCO/VA) also were common in both populations; but the severity of reduced expiratory flow did not correlate with exertional dyspnea. Symptoms referable to previous hantavirus infection had resolved within 3 years of acute infection in most but not all patients in the Panama group. Temporary exertional dyspnea and reduced expiratory flow are common in early convalescence after HPS but resolves in almost all patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since its first discovery in the American Southwest in 1993, hantavirus pulmonary syndrome (HPS) has been described in most countries of the Western hemisphere and is due to acute self-limited infection by a variety of hantaviruses hosted by wild sigmodontine rodents [1]. More than 400 individuals with HPS in North America and more than 2000 in South America have experienced mortality rates of 25–35%. Pulmonary capillary endothelial cells express higher densities of infection [2] compared with other organs associated with a pneumonitis characterized by mononuclear cell infiltration and pulmonary edema [3]. The clinical disease is manifested by a viral prodrome of 1–8 days, followed by the precipitous onset of pulmonary edema with or without cardiogenic shock [4–6]. The cardiopulmonary phase persists for up to 1 week, followed by spontaneous diuresis and a convalescent phase characterized by weakness and exertional dyspnea for 3–4 weeks in almost all survivors.
Some survivors of HPS in New Mexico reported exertional dyspnea and other symptoms persisting for longer than 6 months. Similar residual symptoms were commonly noted also in Panama, where Choclo virus infection is associated with a lower mortality rate of 16% among hospitalized patients with HPS [7]. Infection with Choclo virus frequently results in mild infection without pulmonary complications, and seroprevalence rates over 20% are common in the adult population without a history of hospitalization for HPS [8]. This report documents exertional dyspnea and decreased expiratory flow rates in late convalescence among small groups of patients in Panama infected in 2000 and in New Mexico infected in 1993–1995.
Materials and Methods
Acute HPS Adults—New Mexico
In 1993 through 1994 in New Mexico, 23 adults were diagnosed with HPS by immunoblot serology and reverse transcriptase-polymerase chain reaction (RT–PCR) [9]. Nine patients (average age = 35 years) returned for routine follow-up exam 2–14 months after admission. Patients self-reporting respiratory symptoms not present before acute hantavirus infection underwent a brief structured questionnaire and pulmonary function testing. Three and 8 years after acute infection, the patients were contacted by phone to repeat the questionnaire but spirometry was not obtained. None were active smokers and one woman had quit smoking 16 years earlier after a 10-pack-year history. None had underlying chronic disease, and all were employed before the acute hantavirus infection. Five of the nine required mechanical ventilation, and one received extracorporeal membrane oxygenation (ECMO) treatment.
Acute HPS Adults—Panama
In 2000 in Panama, 22 adults and 1 adolescent were diagnosed by serology with HPS which was confirmed as Choclo infection by RT–PCR of RNA extracted from an acute blood specimen. Five of these patients died within 48 h of diagnosis and four were lost to follow-up. The 14 remaining patients consented to be interviewed by two of the authors (FG and FK) for residual pulmonary symptoms using the same questionnaire 10–14 months after hospitalization for HPS. Interviewed subjects included 8 women and 6 men aged 27–56 years (mean = 38 years). Pulmonary function tests were requested and obtained on 11 of the 14 subjects. Interviews were conducted with the same questionnaire 2 and 8 years later from 11 and 5 of the 14 patients, respectively, and pulmonary function tests were repeated when considered clinically appropriate by the attending physician. All subjects were employed and active previous to hantavirus infection; none were active smokers and one male had quit smoking 10 years prior to infection. One patient in each of the 2- and 8-year-follow-up groups had essential hypertension, depression, chronic back pain, and a history of drug abuse, but none were ever diagnosed or treated for an acute or chronic respiratory disease. Five had HPS requiring mechanical ventilation (MV); two of the five also required intravenous fluids for hypotension. Nine required oxygenation using only nasal cannula or mask.
Hantavirus-Seropositive Adults—Panama
In 2000, the Ministry of Health in Panama conducted serosurveys of household and neighborhood contacts of the above-mentioned HPS patients. Among the 48 people surveyed, 5 adults were seropositive for hantavirus-specific serum IgG antibody as detected by both strip immunoblot and EIA assays. Specificity for previous Choclo virus infection was confirmed by focus assay that neutralizes Choclo virus in Vero E6 cells in a titer greater than 1:200 (Koster, unpublished data). These contacts reported no previous hospitalization or treatment for an acute severe respiratory illness, none had underlying disease, and none reported a history of smoking cigarettes. Ten to 16 months after HPS in the family member, the contacts were interviewed once by questionnaire and spirometry was performed. The clinical protocols and informed consent were approved by the Ministry of Health of Panama, the University of New Mexico Human Research Review Committee, and the ICIDR Review Committee of the National Institute of Allergy and Infectious Diseases.
Questionnaire
The symptom survey instrument of 20 open-ended questions was designed for this study to elicit self-reported symptoms and included 7 questions on respiratory complaints, 8 on nonrespiratory functions including sleep, and 5 on general health. New medical diagnoses were sought, as well as recent and remote history of smoking, alcohol use, and recreational drug use. The degree of respiratory difficulty that was new since the diagnosis of hantavirus infection was graded as 4+ if dyspnea prevented sedentary occupation, 3+ if the subject was unable to walk more than 50 m on level ground, 2+ if the subject was unable to climb a flight of stairs or a hill more than 10 m in height, and 1+ if the subject was unable to engage in physical sport requiring running or jumping but was unaffected by normal daily activity. Although the questions were the same for each population, use of English and Spanish prevented meaningful internal validation.
Spirometry
Pulmonary function testing in Panama and in the United States was performed by a computerized wedge spirometer to obtain lung volumes, inspiratory and expiratory flow rates, and carbon monoxide diffusion capacity (DLCO). Standardization of spirometry was achieved by using ATS criteria [10] and a minimum of four forced expiratory efforts and inspection of the flow volume loop to ensure best effort results. Results were compared to normal middle-aged North American adults [11].
Results
Symptoms
Six of the 14 (43%) Panamanian subjects reported exertional dyspnea, graded as 3+ in two patients, 2+ in two patients, and 1+ in two patients, persisting for 1 year after acute infection. The four subjects reporting grade 2+ and 3+ dyspnea also reported sleep disturbance with nocturnal dry cough and fatigue on rising in the morning. No subject reported wheezing, orthopnea, daytime cough, or sputum production. Three of the six dyspneic subjects had been treated by MV during acute HPS, compared to two of eight subjects without dyspnea (not significant by Fisher’s exact test). The five seropositive neighborhood contacts studied by questionnaire and spirometry reported no respiratory symptoms, including exertional dyspnea. Among the nine New Mexican subjects surveyed 10–14 months after admission for acute HPS, seven (77%) reported exertional dyspnea manifested as either difficulty in engaging in hiking or bicycling (grade 1+ in three subjects) or difficulty climbing stairs (grade 2+ in four subjects). Two subjects reported fatigue on rising in the morning, but none reported sleep disturbance or nocturnal cough.
When interviewed 3 years after acute hantavirus infection in Panama, only two of six subjects reported dyspnea when climbing stairs (grade 2+). A third man reported continued exertional dyspnea; spirometry identified severe restrictive lung disease consistent with his history of crack inhalation. One woman had developed disseminated malignant melanoma and new exertional dyspnea with cachexia. When interviewed 8 years after HPS, four individuals reported exertional dyspnea (grade 2+), and two of these also reported sleep interruption due to nocturnal cough. The four seropositive household contacts in Panama continued to report no respiratory symptoms. Among nine New Mexican subjects, only one reported increased exertional dyspnea at 3 and 8 years after acute infection.
Pulmonary Function
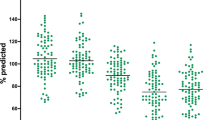
In 11 Panamanian survivors tested 1 year after HPS, the FEV1/FVC ratio was a mean of 103 (range = 0.61–1.31). The one individual below 98% predicted (ratio = 0.61) was the active smoker. The average FEV1/FVC ratio of the seropositive controls was 0.98 (range = 0.88–1.08). In New Mexican survivors 6–12 months after HPS, the average FVC was 102% predicted (range = 88–115%) and the average FEV1 was 97% predicted (range = 84–111%). These convalescence values contrasted with the previous discharge values in three survivors measured (FVC mean = 74% predicted, range = 67–76%; FEV1 mean = 70%, range = 62–73%). In contrast, FEF25–75% values were modestly to markedly reduced in most subjects of both populations (Fig. 1). Among the six dyspneic Panamanians, four of five studied had abnormal FEF25–75%, mean = 63% predicted (range = 55–93%). Six of the eight subjects without exertional dyspnea were tested and four had significantly reduced FEF25–75% values, with a mean of 60.7% predicted. There was no relationship between exertional dyspnea and abnormal expiratory flow rates (not significant by Mann–Whitney rank sum test). Among the five asymptomatic seropositive contacts, the four without asthma had a mean FEF25–75% of 82% predicted (range = 59–102%).
Pulmonary function testing in late convalescence in 9 adult survivors of Sin Nombre virus infection in New Mexico tested at hospital discharge and/or 3–6 months later, and in 14 adult survivors of Choclo virus infection in Panama tested 10–14 months after hospital discharge. Left panel FEF25–75% as % predicted for gender, age, and weight. Middle panel RV/TLC ratio as % predicted for gender, age, and weight. Right panel DLCO/VA as % predicted. Group A: 9 subjects studied within 1 month after discharge with HPS due to Sin Nombre virus infection in New Mexico. Group B: 3 of the 9 subjects studied 3–6 months later. Group C: 14 subjects studied 10–14 months after HPS due to Choclo virus infection in Panama. Group D: 4 subjects seropositive for previous hantavirus infection in Panama
Residual volume/total lung capacity ratio (RV/TLC) was increased in most New Mexican survivors tested at discharge (mean = 148% of expected, N = 3) but appeared to improve in three subjects (mean = 101%) by 2–10 months later (Fig. 1). Only two Panamanian survivors had increased RV when tested 1 year after discharge. Among the New Mexican survivors, four of seven had diminished DLCO at discharge, but these values improved upon retesting in three subjects (Fig. 1). All but one Panamanian survivor had normal DLCO at testing 1 year after discharge (Fig. 1). There was no apparent relationship in these small groups between DLCO/VA values and prior MV or persistent symptoms of exertional dyspnea.
Discussion
This preliminary descriptive study was initiated to assess the prevalence of persistent dyspnea after hantavirus infection in Panama and the U.S. Southwest. Results indicate that while exertional dyspnea and expiratory flow abnormalities may commonly persist for up to 1 year, the residual clinical effects of hantavirus lung infection appear to resolve in most individuals among the Panamanian and North American groups studied 3 and 8 years after acute infection. While HPS is caused by different hantaviruses in the two regions, the pattern of persistent pulmonary function abnormalities, expiratory flow reduction, and increased residual volume was similar in both groups, likely due to the common pathogenetic features of HPS seen throughout the Americas. The persistence of respiratory symptoms was not correlated with either the severity of acute disease or the use of MV. Furthermore, in this small study respiratory symptoms did not correlate with persistent respiratory dysfunction detected by simple spirometry. Reduced gas transport capacity of the lung is not predictive of exertional dyspnea in survivors of Legionella pneumonia [12]. Moreover, discordance between respiratory symptoms and evidence for small-airway flow impairment is found among middle-aged nonsmoking Americans without a history of severe respiratory infection [13].
The possible mechanism of exertional dyspnea and persistent small-airway airflow obstruction resulting from hantavirus pneumonitis is not known. Acute respiratory distress syndrome is associated with decreased DLCO but with normal lung volumes [14]. Acute influenza A induced gas transport abnormality in the lung for up to 6 months in healthy adults, although resolution was documented in all survivors [15]. Small-airway flow also was temporarily reduced in acute influenza, while other spirometric measures of pulmonary function were unaffected [16]. Caution should be taken in making direct comparisons between hantavirus pneumonitis and other viral pneumonitides because, unlike the infected epithelial cells seen in influenza pneumonitis, acute hantavirus pneumonitis is characterized by an intense viral infection of pulmonary capillary endothelial cells [2].
Measures of neuropsychological health were not sought in this preliminary survey, although disruption of sleep was commonly reported during the first year of convalescence. Survivors of severe acute lung injury perceived a decline in general physical health [17], and post-traumatic stress disorder may be induced by acute Legionella pneumonia [18]. Three HPS survivors in Panama reported persistent general health impairment attributable to Choclo virus infection 8 years later, but a larger study with controls is required to distinguish HPS from other causes. Recovery from HPS due to SN virus may lead to general health impairment [19] or renal dysfunction years after infection [20].
This small study does not rule out the persistence of disability for years after acute infection in a small number of survivors, nor does it rule out the persistence of lung structural injury that may synergize with other lung insults such as ventilator-induced lung injury to induce chronic respiratory disability in this population. Our study is limited by the small patient population, the lack of ambulatory pulse oximetry, and pulmonary function testing at the time of symptom resolution. Nonetheless, it is unlikely that hantavirus infection contributes significantly to the prevalence of chronic respiratory dysfunction in either country.
Abbreviations
- DLCO:
-
Diffusing capacity of the lung for carbon monoxide
- DLCO/VA:
-
Diffusion capacity/volume alveolar
- EIA:
-
Enzyme-linked immunoassay
- ECMO:
-
Extracorporeal membrane oxygenation
- FEF:
-
Forced expiratory flow
- FEV1/FVC:
-
Forced expiratory volume in 1 s/forced vital capacity ratio
- HPS:
-
Hantavirus pulmonary syndrome
- MV:
-
Mechanical ventilation
- RT–PCR:
-
Reverse transcriptase-polymerase chain reaction
- RV:
-
Residual volume
- SN:
-
Sin Nombre virus
- TLC:
-
Total lung capacity
References
Koster FT, Hjelle B (2004) Hantaviruses. In: Gorbach SL, Bartlett JG, Blacklow NR (eds) Infectious diseases. Lippincott Williams & Wilkins, Philadelphia, PA, pp 2023–2031
Zaki SR, Greer PW, Coffield LM, Goldsmith CS, Nolte KR, Foucar K, Feddersen R, Zumwalt RE, Miller GL, Khan AS, Rollin PE, Ksiazek TG, Nichol ST, Mahy BWJ, Peters CJ (1995) Hantavirus pulmonary syndrome. Pathogenesis of an emerging infectious disease. Am J Pathol 146:552–579
Nolte KB, Feddersen RM, Foucar K, Zaki SR, Koster FT, Madar D, Merlin TL, McFeeley PJ, Umland ET, Zumwalt RE (1995) Hantavirus pulmonary syndrome in the United States: a pathological description of a disease caused by a new agent. Hum Pathol 26(1):110–120
Duchin JS, Koster FT, Peters CJ, Simpson GL, Tempest B, Zaki SR, Ksiazek TG, Rollin PE, Nichol S, Umland ET, Moolenaar RL, Reef S, Nolte K, Gallaher M, Butler JC, Breiman RF (1994) Hantavirus pulmonary syndrome: a clinical description of 17 patients with a newly recognized disease. N Engl J Med 330(14):949–955
Levy H, Simpson SQ (1994) Hantavirus pulmonary syndrome. Am J Respir Crit Care Med 149:1710–1713
Castillo C, Naranjo J, Sepúlveda A, Ossa G, Levy H (2001) Hantavirus pulmonary syndrome due to Andes virus in Temuco, Chile: clinical experience with 16 adults. Chest 120:548–554
Vincent MJ, Quiroz E, Gracia F, Sanchez AJ, Ksiazek TG, Kitsutani PT, Ruedas LA, Tinnin DS, Caceres L, Garcia A, Rollin PE, Mills JN, Peters CJ, Nichol ST (2000) Hantavirus pulmonary syndrome in Panama: identification of novel hantaviruses and their likely reservoirs. Virology 277:14–19
Armien B, Pascale JM, Bayard V, Munoz C, Mosca I, Guerrero G, Armien A, Quiroz E, Castillo Z, Zaldivar Y, Gracia F, Hjelle B, Koster F (2004) High seroprevalence of hantavirus infection on the Azuero peninsula of Panama. Am J Trop Med Hyg 70(6):682–687
Hjelle B, Jenison S, Torrez-Martinez N, Herring B, Quan S, Polito A, Pichuantes S, Yamada T, Morris C, Elgh F, Lee HW, Artsob H, Dinello R (1997) Rapid and specific detection of Sin Nombre virus antibodies in patients with hantavirus pulmonary syndrome by a strip immunoblot assay suitable for field diagnosis. J Clin Microbiol 35(3):600–608
American Thoracic Society (1994) Standardization of spirometry 1994 update. Am J Respir Crit Care Med 152:1107–1136
American Thoracic Society (1991) Lung function testing: selection of reference values and interpretative strategies. Am Rev Respir Dis 144:1202–1218
Jonkers RE, Lettinga KD, Pels Rijcken TH, Prins JM, Roos CM, van Delden OM, Verbon A, Bresser P, Jansen HM (2004) Abnormal radiological findings and a decreased carbon monoxide transfer factor can persist long after the acute phase of Legionella pneumophila pneumonia. Clin Infect Dis 38(5):605–611
Mannino DM, Etzel RA, Flanders WD (1993) Do the medical history and physical examination predict low lung function? Arch Intern Med 153:1892–1897
Herridge MS, Cheung AM, Tansey CM, Matte-Martyn A, Diaz-Granados N, Al-Saidi F, Cooper AB, Guest CB, Mazer CD, Mehta S, Stewart TE, Barr A, Cook D, Slutsky AS (2003) One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med 348(8):683–693
Horner GJ, Gray FD Jr (1973) Effect of uncomplicated, presumptive influenza on the diffusing capacity of the lung. Am Rev Respir Dis 108(4):866–869
Ledder SR, Gill PW, Peat JK (1974) Short and long term effects of influenza A on lung function. Med J Aust 2(22):812–814
Weinert CR, Gross CR, Kangas JR, Bury CL, Marinelli WA (1997) Health-related quality of life after acute lung injury. Am J Respir Crit Care Med 156:1120–1128
Lettinga KD, Verbon A, Nieuwkerk PT, Jonkers RE, Gersons BPR, Prins JM, Speelman P (2002) Health-related quality of life and posttraumatic stress disorder among survivors of an outbreak of Legionnaire’s disease. Clin Infect Dis 35(1):11–17
Hopkins RO, Larson-Lohr V, Weaver LK, Bigler ED (1998) Neuropsychological impairments following hantavirus pulmonary syndrome. J Int Neuropsychol Soc 4(2):190–196
Pergam SA, Schmidt DW, Nofchissey RA, Hunt WC, Harford AH, Goade DE (2009) Potential renal sequelae in survivors of hantavirus cardiopulmonary syndrome. Am J Trop Med Hyg 80(2):279–285
Acknowledgments
We thank the health-care services and personnel and referring physicians at the Los Santos Regional Hospital in Las Tablas, Panama, and the University of New Mexico Health Science Center, Albuquerque, NM, USA. This work was funded through an Opportunity Pool grant and annual supplements from the International Centers for Infectious Disease Research (ICIDR) program (P01 AI45452) and from the Ministry of Health, Republic of Panama.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Gracia, F., Armien, B., Simpson, S.Q. et al. Convalescent Pulmonary Dysfunction Following Hantavirus Pulmonary Syndrome in Panama and the United States. Lung 188, 387–391 (2010). https://doi.org/10.1007/s00408-010-9245-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-010-9245-4