Abstract
Disorganization is a nuclear dimension of psychosis, especially in schizophrenia. Despite its relevant association with poor prognosis and negative outcomes, it is still under-investigated compared to positive and negative symptoms, in particular at the onset of illness. This study explored disorganization in youth at Clinical High Risk for Psychosis (CHR-P) over a 2-year period. A sample of 180 CHR-P participants (50% males; 51.1% with baseline second-generation antipsychotic medication) recruited within a specialized CHR-P service completed the Positive and Negative Syndrome Scale (PANSS) and the Global Assessment of Functioning (GAF) scale. Across the follow-up, we examined key associations of disorganization with other domains of psychopathology, functioning, and treatment response using Spearman’s rank correlation coefficients and linear regression analyses. Our results showed a significant longitudinal reduction in disorganization severity levels across the follow-up. This decrease was significantly associated with improvements in negative symptoms and daily functioning, with a shorter duration of untreated psychiatric symptoms, and with baseline equivalent dose of antipsychotic medication. No significant longitudinal associations with other treatment component of the PARMS program were found. Our findings suggest a longitudinal improvement in disorganization dimension in CHR-P individuals, especially in the context of early interventions targeting reduction in the duration of untreated psychiatric symptoms and favoring a prompt antipsychotic therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Disorganization is a common and easily misused term in everyday clinical practice [1] As a symptom mostly associated with schizophrenia spectrum disorders, it is currently used for the description of a broad range of manifestations, concerning disturbances in behavior, thought and speech [2]. Dating back to Bleuler [3], the core definition of schizophrenia itself was built around the recognition of a disease where thought (associations), emotions and behavior (abnormal affect and ambivalence) lost coordination and coherence. Consequently, the term “disorganized” acquired mildly different meanings, as a descriptor.
However, the first conceptualization of the now-called “disorganization” features in psychosis can be found in the classical descriptions of “heboidophrenia” [4] and “hebephrenia” [5], two forms of psychosis classically having their first appearance during puberty. Their clinical presentation was characterized by silly behavior, inappropriate affect, hardly systematized delusions/hallucinations, and thought disorder (especially in heboidophrenia) [6, 7]. Within a decade, hebephrenia and heboidophrenia were firmly embedded concepts of adolescent insanity [8].
Some years later, Kraepelin [9] included hebephrenia as a specific subgroup of his “dementia praecox”. His effort to create a unitary model of psychosis inevitably led to the loss of what the term “hebephrenia” was meant to describe in a specific way (e.g., the close link to puberty and adolescence), yet determined the first relevant conceptualization of the disorganization syndrome [10]. In line with Kraepelin, hebephrenia was included among schizophrenia subtypes until the 5th edition of Diagnostic and Statistical Manual of mental disorder (DSM-5) [11], where all the subgroups were eliminated. What led to the removal of these categories was the increasing evidence that, despite their historical and theoretical meaning, they had low stability and reliability [12].
However, although considered by classical psychopathology as a “core” feature of psychosis (especially schizophrenia), disorganization more recently drew less attention than positive and negative symptoms [13]. This was probably because of early models of schizophrenia psychopathology incorporating disorganization with “reality distortion” features (i.e., delusions and hallucinations) to establish a positive domain [14]. To date, the conflation of positive and disorganized symptoms still persists, as can be observed in the most commonly used psychopathological instruments for assessing psychosis psychopathology (such as the Positive and Negative Syndrome Scale [PANSS]) [15, 16]. Additionally, most of the current measures of disorganization in psychosis research were derived from factor analyses based on the dichotomic (positive vs. negative) model of symptoms [17] and were extrapolated within psychometric tools not specifically developed for the assessment of disorganization. Indeed, some items of these statistical dimensions are not focused on disorganized features (e.g., the PANSS “Disorientation” item) [18].
Lastly, as evidence reported that disorganization in psychosis is a clinical predictor of poor prognosis and daily functioning deterioration [19], first-line treatments in “Early Intervention in Psychosis” (EIP) programs should also consider this crucial psychopathological target, especially at the illness onset [20]. In this respect, most research on disorganization was carried out in clinical populations with prolonged psychosis, having cross-sectional design. Empirical investigations on disorganized symptoms in early stages of psychosis (including at-risk mental states) are scarce, and a lack of knowledge still affects their longitudinal course and their treatment response.
Based on this background, the aims of this study were: (a) to investigate the longitudinal stability of disorganization in young individuals at Clinical High Risk for Psychosis (CHR-P) across a 2-year follow-up period, and (b) to examine any significant association of disorganization with sociodemographic characteristics, clinical features, and the specialized treatment components of an EIP program across the follow-up. As differences in disorganization and treatment outcome could be just a proxy of those CHR-P individuals who has been on Antipsychotic (AP) drug at the time of inclusion or how much medication someone already received, we also decided to compare CHR-P subjects with and without baseline medication in terms of sociodemographic and outcome information, and most importantly, symptomatology, especially disorganization. To the best of knowledge, no longitudinal investigation specifically examining disorganization in CHR-P individuals has been reported in the literature to date.
Methods
Subjects and setting
All participants were consecutively recruited within the “Parma At-Risk Mental States” (PARMS) program from January 2016 to December 2020. The PARMS program was a specialized “Early Intervention in Psychosis” infrastructure diffusely implemented in all adult and adolescent mental healthcare services of the Parma Department of Mental Health (Northern Italy) [21].
Inclusion criteria were: (1) specialized help-seeking request; (2) age 12–25 years, (3) to meet CHR-P criteria at entry, as defined by the “Comprehensive Assessment of At-Risk Mental States” (CAARMS): i.e, “Genetic Vulnerability” (GV), “Attenuated Psychotic Symptoms” (APS), or “Brief Limited Intermittent Psychotic Symptoms” (BLIPS) [22].
Exclusion criteria were: (1) past full-blown (non-affective or affective) psychotic episodes; (2) past exposure to AP medication or current AP prescription for more than four weeks, (3) known intellectual disability (IQ < 70); (d) neurological or other somatic disorder with psychiatric manifestations (including traumatic brain injury). Past AP use (i.e., in past illness episode before the PARMS enrollment) was considered as a proxy for a past psychotic episode, consistently with the original CAARMS criteria for psychosis threshold [23]. A current AP use for more than four weeks (i.e., in the present illness episode at the PARMS enrollment) was required to minimize pharmacological interference with baseline assessment within our EIP program [21]. However, no dosage threshold was selected.
All CHR-P participants and their parents (if minors) agreed to participate in the research and gave their written informed consent prior to their inclusion in the study. Local relevant ethical approval was obtained for the research (AVEN Ethics Committee: protocol n. 559/2020/OSS*/AUSLPR). This investigation was carried out in accordance with the Code of Ethics of the World Medical Association (1964 Declaration of Helsinki and its later amendments). The data supporting the findings of this research are available on reasonable request from the corresponding author. The data are not publicly available due to privacy and/or ethical restrictions.
Assessment
The psychopathological assessment included the CAARMS, the PANSS, and the “Global Assessment of Functioning” (GAF) scale [11].
The CAARMS is a semi-structured clinical interview developed to cover various aspects of attenuated psychopathology. The CAARMS “Positive Symptoms” subscale was used to define both CHR-P and psychosis threshold criteria. Specifically trained PARMS team members conducted CAARMS interviews at entry, using the approved Italian version (CAARMS-ITA) [24]. Regular CAARMS supervision sessions and scoring workshops were implemented and maintained to ensure good interrater reliability values [25].
The PANSS is a widely used structured clinical interview for assessing psychopathology in patients with psychosis, including young individuals with early psychosis [26, 27].
As for how to measure disorganization, we preliminarily examined the goodness of fit of two different PANSS “Disorganization” factor solutions previously identified in the literature on individuals with psychosis or at CHR-P, using a Confirmatory Factor Analysis (CFA): (1) the 8-item “disorganization” factor model (including PANSS P2, N5, N7, G5, G10, G11, G13, and G15 items) proposed in a meta-analysis on the PANSS by Shafer and Dazzi [18], and (2) the 5-item factor model (including PANSS P2, P5, G9, G11, and G13 items) identified by Yang and co-workers [28] in a specific CHR-P population in Singapore.
The GAF is a widely used scale to assess clinical and socio-occupational outcomes in individuals with severe mental disorders, including young individuals with early psychosis [29] and CHR-P populations as well [30].
A sociodemographic and clinical chart (including information on ethnic group, gender, age, years of education, past specialist contact, family history of psychosis, current substance abuse, and “Duration of Untreated Psychiatric Symptoms” [DUPS, defined as the time interval [in weeks] between the onset of any psychiatric symptom in need of specialist treatment and initiation of an adequate, specialized psychopharmacological/psychosocial intervention]) [31] was completed at entry. Specifically, the DUPS was based on interviews with the individual and at least one key informant (usually a close relative), and was specifically referring to the time interval before the first psychiatric contact and before the first psychotropic prescription.
The initial DSM-5 diagnosis was formulated through assessments conducted by a minimum of two trained PARMS team members, using the Structured Clinical Interview for DSM-5 disorders (SCID-5) [32]. All psychopathological instruments were administered both at entry and every 12 months during the 2-year follow-up period. Information on AP dose and intensity of the different components of PARMS psychosocial interventions was collected both at baseline and every 12 months across the follow-up.
Procedures
After CAARMS interviews and baseline psychopathological assessment, CHR-P participants were assigned to a multi-disciplinary team (consisting of a clinical psychologist, an early rehabilitation case manager, and a psychiatrist) within 3–4 weeks (see Supplementary Materials [Table S1] for details on treatment components of the PARMS program). In accordance with current official guidelines on EIP [33, 34], AP drug prescription should be proposed when individuals at CHR-P (a) showed a sudden decline in daily functioning, (b) had a rapid escalation to overt psychotic symptoms, (c) showed an immediate risk of suicide or severe violence, or (d) did not adequately respond to any other psychosocial interventions. As a first-line pharmacological treatment, low-dose second-generation AP medication was indicated [35]. Antidepressant and benzodiazepine medication could be prescribed for anxiety, depressive symptoms, and/or insomnia.
After having examined the goodness of fit for both PANSS “Disorganization” factor solutions in the CHR-P total sample using CFA, we investigated any relevant associations of disorganized dimension with sociodemographic, clinical and other psychopathological parameters both at baseline (T0) and across the follow-up. Finally, we examined any significant longitudinal changes in disorganization severity levels over time and their potential associations with treatment components of the PARMS program. As baseline and longitudinal changes in disorganization severity levels could be simply confounded by the fact of how far along CHR-P subjects was in the treatment trajectory, we also conducted our statistical analyses in baseline AP medicated and unmedicated CHR-P subgroups separately.
Statistical analysis
Data were analyzed using the Statistical Package for Social Science (SPSS) for Windows, version 15.0 [36] and the R “Lavaan” package [37]. All tests were two-tailed, with significance level set at 0.05. Categorical variables were reported as frequencies and percentages, while continuous parameters as median and interquartile range.
In our CFA, we used the Robust Weighted Least Squares (RWLS) estimator, which does not assume normally distributed variables and offers the best option for modeling ordinal data in moderately large populations [38]. According to Brown [39], the following four common indices to assess fit of the overall model and to calculate the model adjustment were used: Comparative Fit Index (CFI), Tucker-Lewis Index (TLI), Root Mean Square Error of Approximation (RMSEA), and Standardized Root Mean Square Residual (SRMR). In accordance with the recommendations of Hu and Bentler [40], the following criteria were used: TLI/CFI > 0.90 (accepted fit), RMSEA < 0.08 (accepted fit) and SRMR < 0.08 (good fit). The best fitness of the overall model was represented by higher TLI/CFI values and lower RMSA/SRMR values [40]. Moreover, we calculated the Akaike Information Criterion (AIC), a parsimony correction index to identify the most parsimonious model which fitted the data. Smaller AIC scores indicate the preferred model in terms of comparison to fit and parsimony [41]. We also repeated CFA after 1 year of follow-up (T1) to assess the longitudinal stability of the fit indices for both “Disorganization” factor models investigated.
As no CHR-P participants had a baseline PANSS “Disorganization” dimension score of 0, our statistical analyses were conducted in the CHR-P total sample, as well as in baseline AP medicated and unmedicated subgroups separately. Specifically, Spearman’s rank correlation coefficients and Mann-Whitney U tests were used to examine significant associations of PANSS “disorganization” factor scores with sociodemographic, clinical and psychopathological parameters both at baseline and during the 2-year follow-up period (T2). The Wilcoxon test for repeated measures was also performed to assess the longitudinal stability of PANSS “Disorganization” factor scores across the 2 years of follow-up. Finally, multiple linear regression analyses with PANSS “Disorganization” factor scores as dependent variables and intensity of the specialized PARMS intervention components as independent variables were carried out. In our longitudinal examinations, we used the differences (deltas [Δ]) between T0 and T1 or T2 PANSS scores as primary psychopathological parameters to examine overtime. According to Ver Hoef [42], the delta scores better describe the longitudinal changes and temporal dynamics of psychosis psychopathology compared to T0, T1 and T2 single scores.
Results
Over the course of the study, 180 CHR-P individuals (90 males, 159 white Caucasians, median age = 20 years old [interquartile range = 16–23 years old]) were recruited. At baseline, 92 (51.1%) of them were taking AP medication. The clinical and sociodemographic characteristics of the total sample and the two subgroups are shown in the Table 1. According to the CAARMS definitions, 140 participants met APS criteria, 30 met BLIPS criteria, and 10 met “Genetic Vulnerability” criteria. In accordance with the DSM-5 diagnostic criteria, the most common primary psychiatric diagnoses were: depressive disorders (n = 67), schizotypal personality disorder (n = 30), anxiety disorders (n = 28), and brief psychotic disorder (n = 24) (see Supplementary Materials [Table S1] for details). According to DSM-5 diagnostic criteria [32], psychosis Not Otherwise Specified (NOS) (n = 6) was used as a “diagnosis of exclusion” that was applied to clinical manifestations where psychotic symptoms were present without meeting the full criteria for any specific psychotic disorder. This category was also used in presentations in which the clinician did not choose to communicate the specific reason that the manifestation did not meet the criteria for any specific psychotic disorder, including presentations in which there was insufficient or contradictory information to make a more specific diagnosis and cases with psychosis-like symptoms under the threshold of frank psychosis but considered to be of particular high risk for developing a psychotic disorder [43].At baseline, the CHR-P/AP + subgroup showed older age (z = −4.772; p = .0001), higher PANSS “Positive Symptoms” factor score (z = −2.099; p = .045), and higher prevalence rates of BLIPS (X2 = 9.409; p = .002) and brief psychotic disorder (X2 = 4.311; p = .038) in comparison with CHR-P/AP- participants. No inter-group difference in disorganization levels was found.
Compared to the 5-item factor model identified by Yang and colleagues [28], the 8-item “Disorganization” factor model (18) showed the best fit indices in our population, both at baseline (T0) and after 1 year of follow-up (T1) (see the Table 2 for details on CFA tests and values). Therefore, we used this PANSS factor structure configuration in the remaining statistical analyses of the current research.
As for baseline characteristics of the CHR-P total sample, the PANSS “Disorganization” factor subscore positively correlated with PANSS total score and PANSS “Positive Symptoms” (ρ = 0.284; 0.004), “Negative Symptoms” (ρ = 0.531; p = .0001), and “Affect” (ρ = 0.322; p = .0001) factor subscores. Moreover, it also negatively correlated with GAF score at entry (ρ = − 0.266; p = .003) (Table 3). In the CHR-P/AP + subgroup, PANSS “Disorganization” factor subscore positively correlated with PANSS total score (ρ = 0.841; p = .0001) and all the other PANSS factor subscores (see the Table 3 for details). Differently, in CHR-P/AP- participants, it exclusively correlated with PANSS total score (ρ = 0.728; p = .0001) and PANSS “Negative Symptoms” factor subscore (ρ = 0.546; p = .0001), as well as negatively with GAF score at entry (ρ = − 0.339; p = .006).
As for attrition rate, 5 (2.8%) CHR-P participants dropped out in the first year of treatment (1 in the CHR-P/AP + subgroup and 4 in the CHR-P/AP- subgroup), actively refusing further contact with the treatment staff and being no longer traceable, while 22 (12.2%) did not complete the second year of intervention (10 in the CHR-P/AP + subgroup and 14 in the CHR-P/AP- subgroup): specifically, 6 of them voluntarily dropped out the PARMS program and 11 prematurely left EIP treatments according to their clinicians (see also Supplementary Materials [Table S2] for further details).
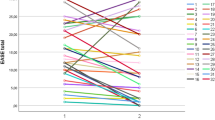
Across the 2 years of our follow-up (Table 4), we found a significant decrease in the PANSS “Disorganization” factor scores in the CHR-P total sample (z = −4.206; p = .0001), more relevant between T0 and T1 (z = −3.105; p = .002). Notably, this statistically significant longitudinal reduction was confirmed exclusively in the CHR-P/AP + subgroup (T0-T2 z = −4.274, p = .0001; T0-T1 z = −3.357, p = .001).
In the CHR-P total sample, such decrease in disorganization severity levels correlated positively with improvement in GAF score (ρ = − 0.382; p = .0001) and in all the other PANSS factor scores, yet negatively with DUPS (ρ = − 0.260; p = .004) (see the Table 5 for details on statistic tests and values). This correlation pattern was substantially confirmed in both CHR-P/AP + and CHR-P/AP- subgroups, with the exception of the association with DUPS (see the Table 5 for details). Notably, in all the three CHR-P groups here examined, the most statistically robust correlation coefficients were with improvements in negative symptom levels over time.
Finally, our multiple linear regression analysis results in the CHR-P total sample showed that longitudinal improvement in disorganization severity levels during the follow-up was predicted by equivalent doses of AP medication (both at baseline [T0B = 1.444; p = .0001] and during the follow-up period [T2B = 1.192; p = .023]), and shorter DUPS (B = − 0.027; p = .00in3) (Table 6), especially in the first year of treatment. A further negative predictive factor was represented by equivalent doses of benzodiazepine (particularly at entry). This prediction pattern was substantially confirmed in the CHR-P/AP + subgroup (see Supplementary Materials [Table S3] for details), together with evidence of the total number of family psychoeducation sessions showing a statistically significant positive association with the reduction in disorganization levels during the first year of intervention (B coefficient = 0.383; Standard Error = 0.149; p = .013).
Although statistically not significant, longitudinal improvement in disorganization among CHR-P/AP- participants was similarly predicted by shorter DUPS and lower equivalent doses of benzodiazepine (see Supplementary Materials [Table S4] for details), as well as by the total number of case management sessions offered during the first year of treatment (B = 0.041; Standard Error = 0.018; p = .025). In the CHR-P/AP- subgroup, no predictive role was observed in terms of AP medication prescribed over time. In this respect, only 15 CHR-P/AP- individuals were taken AP drug at the end of our follow-up period.
Discussion
Although considered as a “core” feature of psychosis, disorganization drew less attention than positive and negative symptoms [13], probably because of early modern models of psychosis psychopathology incorporating disorganized features with “reality distortion” characteristics to establish a positive domain. However, as evidence reported that disorganization in psychosis is an important clinical predictor of poor prognosis and daily functioning deterioration (including in subjects with early psychosis) [19], the aims of this research were to investigate the longitudinal stability of disorganization in a CHR-P population treated within an EIP service along a 2-year follow-up period, and to assess any significant longitudinal association of disorganized dimension with sociodemographic, clinical, and treatment features across the follow-up (also through a comparison between AP medicated and unmedicated CHR-P subgroups). To our knowledge, no perspective research specifically examining disorganization in CHR-P individuals has been reported in the literature to date, especially in terms of treatment response.
First of all, the results of this research suggest that disorganization in CHR-P individuals is closely related to other dimensions of psychosis psychopathology (particularly negative symptoms rather than positive ones) and these connections remain relevant over time. In particular, the privileged and temporally stable link of disorganization with negative features is clearly supported by the evidence of their most statistically robust correlation coefficients observed in all the three CHR-P groups here examined, both at baseline and across the 2 years of follow-up. This seems recall the Bleulerian conceptualization of “loosening of association” as one of the most important (“fundamental”) symptoms in psychosis (especially in schizophrenia), together with other clinical features currently classified as negative symptoms (i.e., volitional indeterminacy, affective incongruence, and withdrawal from reality) [3]. In the author’s thinking, these psychopathological characteristics were considered as “nuclear” in the psychotic disorder, being stably present (right from the onset of psychotic disorder) [44, 45]. Moreover, as reported in young patients with first episode psychosis [1, 2], the contextual decrease of all these PANSS factor subscores (and PANSS total scores) further supports the validity of disorganization as a general severity index both at presentation (i.e., already from the first specialist contact with CHR-P services [also in adolescence]) and over the 2 years of our follow-up. Indeed, in our research, this appeared longitudinally evident both in the CHR-P total sample and in the two subgroups.
The findings of this investigation also suggest a significant, enduring association between disorganization and daily functioning decline, already at the enrollment time in specialized CHR-P services (particularly evident in CHR-P/AP- individuals). This further supports the evidence that the most severely disorganized patients with early psychosis have greater difficulties in real-world performance [13, 14]. Moreover, when coupled with the statistically relevant inverse correlation between improvement in disorganized symptoms and DUPS observed in the CHR-P total sample, our results indicate that disorganization could be associated with clinical severity at entry and poorer clinical and functioning remission overtime. These findings suggest that disorganization can be considered as one of the most useful psychopathological indicators to monitor clinical evolution and treatment response in CHR-P individuals (together with negative symptoms and functioning decline). It is therefore necessary to pay special attention to the severity of disorganized symptoms right from the prodromal stage of psychosis, as well as it is urgent to develop specific tools for adequately assessing this relevant dimension in CHR-P samples. Furthermore, our findings confirm the priority of shortening the DUPS to improve prognosis and outcomes in the CHR-P population [46, 47].
The results of this investigation showed a longitudinal reduction in disorganization severity levels across the follow-up period in the CHR-P total sample, but exclusively in the CHR-P/AP + subgroup. Indeed, although observed also in CHR-P/AP- participants, this decrease did not reach a statistical significance. As for intervention response in our CHR-P total population, the findings of this research indicate that the longitudinal mitigation of disorganized symptoms is primarily related to shorter DUPS and pharmacological interventions with AP medication (both at entry and across the follow-up). This prediction pattern was substantially confirmed in the CHR-P/AP + subgroup, with the addition of the evidence that the total number of family psychoeducation sessions showed a statistically significant positive association with the reduction in disorganization levels during the first year of intervention. Indeed, it is noteworthy that the relevant effects on this clinical improvement occurred within the first year of treatment (with no relevant additional result observed between T1 and T2). This finding may be related to the fact that the greater intensity of PARMS interventions for CHR-P individuals was provided in the first 12 months. Maintaining at least the same treatment intensity and clinical monitoring during the second year of intervention could thus longitudinally extent its beneficial effects [48, 49].
Despite the recommendations by most international CHR-P guidelines that would substantially avoid the AP use in young individuals at CHR-P [50], our findings suggest a potential usefulness of their prescription for attenuating disorganized features, as well as the importance of starting treatment as soon as indicated and then try to get the most out of the first year of intervention [51]. However, further confirmation studies will be necessary to validate the obtained results, especially on larger CHR-P populations. In particular, these findings should also be interpreted in the light of the evidence that baseline AP exposure in CHR-P population could suggest a condition of immanent risk of transition to psychosis [52,53,54]. Indeed, as baseline severity illness and DUPS appeared to be actually relevant factors in reduction of disorganization in our CHR-P population, individuals could be already in different disease trajectories to begin. Anyway, the predictive role of shorter DUPS and AP medication in disorganization improvement is substantially confirmed also in the CHR-P/AP + subgroups. Moreover, in all our three CHR-P groups, another predictive factor in disorganization reduction is represented by lower equivalent doses of benzodiazepine (both at baseline and across the first year of treatment). Although not immediately intuitive, these findings could be due to a common prescription pattern that favors AP medications over benzodiazepines in CHR-P individuals with predominant disorganized symptoms or more severe general psychopathology. In this respect, compared to CHR-P/AP- at baseline, CHR-P/AP + participants showed higher prevalence of BLIPS, brief psychotic disorder, and emergency room as source of referral.
Finally, an interesting role in predicting disorganization reduction (at least during the first year of treatment) seems also to be played by some psychosocial interventions offered within the PARMS program (specifically by family psychoeducation in the CHR-P/AP + subgroup and case management in the CHR-/AP- subgroup). Overall considered, these results confirm the potential usefulness of combining pharmacological and psychosocial treatments in young individuals with early psychosis.
Limitations
Strength of this investigation was that we examined CHR-P subjects within a real-world setting, primarily aimed at delivering optimal clinical care pathways within community mental healthcare services. However, our results are mainly generalizable to similar samples. Another limitation that should also be acknowledged was that this investigation was conducted within a CHR-P program that did not specifically focus on disorganization. Psychometric assessment of major psychopathology was performed with the PANSS and the CAARMS, which are clinical interviews frequently used in individuals with early psychosis, but not originally developed for evaluating the disorganization dimension of psychosis. Lacking instruments to specifically assess disorganization in the early stage of psychosis and consequently having to use psychopathological domains derived from factor analysis methods, future research aimed at developing and validating specific psychometric scales for disorganized features are absolutely desirable and necessary. However, given the widespread use of the PANSS in CHR-P populations [20], our findings have the potential to be replicated in other CHR-P samples and offer a lead to further evaluate disorganization and its treatment response in the early phase of psychosis. This is of primary importance, since research on this topic is still scarce and disorganized symptoms have detrimental effects both on daily functioning and real-world performance.
Another limitation is that we could not evaluate the potential link between disorganization and neurocognitive functioning (although recent evidence seems to suggest that they are separate dimensions in patients with first episode psychosis) [13]. Thus, further investigations examining this potential association in CHR-P subjects are needed. However, in the current study, known intellectual disability was among exclusion criteria.
A final limitation of this study is related to the restrictions on AP medication. Indeed, we exclusively used a time restriction on AP medication (i.e., less than 4 weeks) to select our CHR-P participants and to classify them into the two pharmacological subgroups. No dosage restriction was used, but having received 20 mg/day of olanzapine for 2 weeks is probably something different than having received 25 mg/day of quetiapine for 5 weeks. Therefore, a detailed prospective analysis on AP prescription and medication in larger CHR-P populations is needed.
Conclusions
Disorganization is a clinically relevant dimension in CHR-P individuals (as well as it is in young patients with first episode psychosis) [2]. In particular, it represents a longitudinally stable psychopathological index of general clinical severity (right from the recruitment in specialized CHR-P programs) and maintains significant enduring relationships especially with daily functioning decline and negative symptoms. However, longitudinal improvement in disorganization severity levels seems to be related to shorter DUPS and AP prescription at baseline, especially during the first year of treatment. More clinical attention and targeted interventions on disorganized symptoms in young individuals at CHR-P are thus recommended, especially in order to reach better clinical outcomes and prognosis. Future studies based on longer-term observation are needed to progress and replicate our findings, as well as to investigate any misuse/overuse of antipsychotic medications [55]. In particular, the time has come when the problem of disorganization should be observed by paying attention to its potential inflammatory effect [56].
References
Pelizza L, Leuci E, Maestri D, Quattrone E, Azzali S, Paulillo G, Pellegrini P (2022) Examining disorganization in patients with first episode psychosis: findings from a 1-year follow-up of the Parma early psychosis program. Early Interv Psychiatry 16:552–560. https://doi.org/10.1111/eip.13198
Pelizza L, Leuci E, Maestri D, Quattrone E, Azzali S, Paulillo G, Pellegrini P, Raballo A (2021) Disorganization in first episode schizophrenia: treatment response and psychopathological findings from the 2-year follow-up of the Parma Early psychosis program. J Psychiatr Res 141:293–300. https://doi.org/10.1016/j.jpsychires.2021.07.015
Bleuler E (1911) Dementia Praecox Oder Gruppe Der Schizophrenien., Leipzig
Kahlbaum KL (1863) Die gruppierung Der Psychischen Krankheiten Und die Einteilung Der seelenstörungen., Danzig
Hecker E (1871) Die Hebephrenie. Arch Pathol Anat Physiol Klin Med 52:394–429. https://doi.org/10.1007/BF02329963
Kraam A, Phillips P (2012) Hebephrenia: a conceptual history. Hist Psychiatry 23:387–403. https://doi.org/10.1177/0957154X11428416
De Page L, Englebert J (2018) Heboidophrenia and pseudo-psychopathic schizophrenia: current knowledge and critical perspective. Psychopathology 51:227–233. https://doi.org/10.1159/000488768
Kraam A, Berrios GE (2002) On heboidophrenia, by K.L. Kahlbaum (translation with an introduction). Hist Psychiatry 13:197–201. https://doi.org/10.1177/0957154X0201305005
Kraepelin E (1899) Psychiatrie: ein lehrbuch für studirende und aerzte., Leipzig
Kendler KS (2020) The development of Kraepelin’s mature diagnostic concept of Hebephrenia: a close reading of relevant texts of Hecker, Daraszkiewicz, and Kraepelin. Mol Psychiatry 25:180–193. https://doi.org/10.1038/s41380-019-0411-7
American Psychiatric Association (APA) (2013) Diagnostic and Statistical Manual of mental disorders, 5th Edition (DSM-5). APA Press, Arlington (VA)
Tandon R, Gaebel W, Barch DM, Bustillo J, Gur RE, Heckers S, Malaspina D, Owen MJ, Schultz S, Tsuang M, Van Os J, Carpenter W (2013) Definition and description of schizophrenia in the DSM-5. Schizophr Res 150:3–10. https://doi.org/10.1016/J.SCHRES.2013.05.028
Rocca P, Galderisi S, Rossi A, Bertolino A, Rucci P, Gibertoni D, Montemagni C, Bellino S, Aguglia E, Amore M, Bellomo A, Biondi M, Carpiniello B, Cuomo A, D’Ambrosio E, dell’Osso L, Girardi P, Marchesi C, Monteleone P, Montemitro C, Oldani L, Pacitti F, Roncone R, Siracusano A, Tenconi E, Vita A, Zeppegno P, Steardo LJr, Vignapiano A, Maj M Italian Network for Research on psychoses (2018) disorganization and real-world functioning in schizophrenia: results from the multicenter study of the Italian Network for Research on psychoses. Schizophr Res 201: 105–112. https://doi.org/10.1016/j.schres.2018.06.003
Pelizza L, Leuci E, Maestri D, Quattrone E, Azzali S, Paulillo G, Pellegrini P (2021) Disorganization in first episode affective psychosis: treatment response and clinical considerations from a 2-year follow-up study in a real world setting. Rev Psiquiatr Salud Ment. 17th Decemberhttps://doi.org/10.1016/j.rpsm.2021.12.003
Kay SR, Fiszbein A, Opler LA (1987) The positive and negative syndrome scale (PANSS) for Schizophrenia. Schizophr Bull 13:261–276. https://doi.org/10.1093/schbul/13.2.261
Touskova TP, Bob P, Pec O, Raboch J, Lysaker P (2018) Conceptual disorganization and dissociative symptoms in women with first episode psychosis. Schizophr Res 197:609–610. https://doi.org/10.1016/j.schres.2018.02.014
Liddle PF (1987) The symptoms of chronic schizophrenia. Br J Psychiatry 151:145–151. https://doi.org/10.1192/bjp.151.2.145
Shafer A, Dazzi F (2019) Meta-analysis of the positive and negative syndrome scale (PANSS) factor structure. J Psychiatr Res 115:113–120. https://doi.org/10.1016/j.jpsychires.2019.05.008
Prasad K, Rubin J, Iyengar S, Cape J (2023) Global network disorganization underlying psychosis high risk states. Schizophr Res 255:67–68. https://doi.org/10.1016/j.schres.2023.03.033
Leuci E, Pelizza L, Landi G, Quattrone E, Maestri D, Azzali S, Pelosi A, Ceroni P, Soncini C, Daolio MC, Paulillo G, Raballo A, Pellegrini P (2022) Personal health budget in patients with first episode psychosis: a new rehabilitation model based on a community care system in Italy. Early Interv Psychiatry 16:221–230. https://doi.org/10.1111/eip.13145
Pelizza L, Leuci E, Quattrone E, Paulillo G, Pellegrini P (2023) The Parma At-Risk mental states (PARMS) program: general description and process analysis after 5 years of clinical activity. Early Interv Psychiatry 17:625–635. https://doi.org/10.1111/eip.13399
Yung AR, Yuen HP, McGorry PD, Phillips LJ, Kelly D, Dell’Olio M, Francey SM, Cosgrave EM, Killackey E, Stanford C, Godfrey K, Buckby J (2005) Mapping the onset of psychosis: the Comprehensive Assessment of At-Risk Mental States. Aust N Z J Psychiatry 39:964–971. https://doi.org/10.1080/j.1440-1614.2005.01714.x
Raballo A, Poletti M, Preti A (2020) Attenuated psychosis syndrome or pharmacologically attenuated first-episode psychosis? An undesirably widespread confounder. JAMA Psychiatry 77:1213–1214. https://doi.org/10.1001/jamapsychiatry.2020.1634
Raballo A, Semrov E, Bonner Y, Simmons M (2013) Traduzione E Adattamento Italiano Del Comprehensive Assessment of At-Risk Mental States (CAARMS). Centro Stampa della Regione Emilia-Romagna, Bologna
Paterlini F, Pelizza L, Galli G, Azzali S, Scazza I, Garlassi S, Chiri LR, Poletti M, Pupo S, Raballo A (2019) Interrater reliability of the authorized Italian version of the Comprehensive Assessment of At-Risk Mental States (CAARMS-ITA). J Psychopathol 25:24–28. https://old.jpsychopathol.it/wp-content/uploads/2019/02/05_Raballo-1.pdf
Pelizza L, Raballo A, Semrov E, Azzali S, Scazza I, Garlassi S, Paterlini F, Fontana F, Favazzo R, Pensieri L, Fabiani M, Chiri LR, Cioncolini L (2016) Identification of young people at Ultra-high Risk (UHR) of developing psychosis: validation of the Checklist per la valutazione dell’esordio psicotico for use in primary care setting. J Psychopathol 22:172–179. https://old.jpsychopathol.it/wp-content/uploads/2016/12/02_Pelizza-1.pdf
Poletti M, Pelizza L, Azzali S, Garlassi S, Scazza I, Paterlini F, Chiri LR, Pupo S, Raballo A (2022) Subjective experience of aberrant salience in young people at Ultra-high Risk (UHR) for psychosis: a cross-sectional study. Nord J Psychiatry 76:129–137. https://doi.org/10.1080/08039488.2021.1942547
Yang Z, Lim K, Lam M, Keefe R, Lee J (2018) Factor structure of the positive and negative syndrome scale (PANSS) in people at ultra-high risk (UHR) for psychosis. Schizophr Res 201:85–90. https://doi.org/10.1016/j.schres.2018.05.024
Ventura J, Hellemann GS, Thames AD, Koellner V, Nuechterlein KH (2009) Symptoms as mediators of the relationship between neurocognition and functional outcome in schizophrenia: a meta-analysis. Schizophr Res 113:189–199. https://doi.org/10.1016/j.schres.2009.03.035
Zhang T, Wang J, Xu L, Wei Y, Tang X, Hu Y, Cui H, Tang Y, Hui L, Li C, Wang J (2021) Subtypes of clinical high risk for psychosis that predict antipsychotic effectiveness in long-term remission, vol 54. Pharmacopsychiatry, pp 23–30. https://doi.org/10.1055/a-1252-2942
Bhullar G, Norman RMG, Klar N, Anderson KK (2018) Untreated illness and recovery in clients of an early psychosis intervention program: a 10-year prospective cohort study. Soc Psychiatry Psychiatr Epidemiol 53:171–182. https://doi.org/10.1007/s00127-017-1464-z
First MB, Williams JB, Karg RS, Spitzer RL (2016) Structured clinical interview for DSM-5 disorders – clinical version (SCID-5-CV). New York State Psychiatric Institute, New York (NY)
Schmidt SJ, Schultze-Lutter F, Schimmelmann BG, Maric NP, Salokangas RK, Riecher-Rössler A, van der Gaag M, Meneghelli A, Nordentoft M, Marshall M, Morrison A, Raballo A, Klosterkötter J, Ruhrmann S (2015) EPA guidance on the early intervention in clinical high-risk states of psychoses. Eur Psychiatry 30:388–404. https://doi.org/10.1016/j.eurpsy.2015.01.013
Regione Emilia-Romagna (RER) (2023) Raccomandazioni regionali per la promozione della salute e del benessere in persone all’esordio psicotico, II edition. Centro Stampa della Regione Emilia-Romagna, Bologna
Raballo A, Poletti M, Preti A (2021) Antipsychotic treatment in clinical high risk for psychosis: protective, iatrogenic or further risk flag? Aust N Z J Psychiatry 55:442–444. https://doi.org/10.1177/0004867420984836
SPSS Inc (2010) Statistical package for social science (SPSS) for windows, version 15.0. SPSS Inc, Chicago (IL)
Rosseel Y (2012) Lavaan: a R package for structural equation modelling. J Stat Softw 48:1–36. https://doi.org/10.18637/jss.v048.i02
DiStefano C, Morgan GB (2014) A comparison of diagonal weighted least squares robust estimation techniques for ordinal data. Struct Equ Model 21:425–438. https://doi.org/10.1080/10705511.2014.915373
Brown TA (2006) Confirmatory factor analysis for applied research. Guilford Press, New York (NY)
Hu L, Bentler PM (1999) Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Model 6:1–55. https://doi.org/10.1080/10705519909540118
Portet S (2020) A primer on model selection using the Akaike Information Criterion. Infect Dis Modelling 5:111–128. https://doi.org/10.1016/j.idm.2019.12.010
Ver Hoef JM (2012) Who invented the Delta method? Am Stat 66:124–127. https://doi.org/10.1080/00031305.2012.687494
Fusar-Poli P, De Micheli A, Cappucciati M, Rutigliano G, Davies C, Ramella-Cravaro V, Oliver D, Bonoldi I, Rocchetti M, Gavaghan L, Patel R, McGuire P (2018) Diagnostic and prognostic significance of DSM-5 attenuated psychosis syndrome in services for individuals at Ultra-high Risk for psychosis. Schizophr Bull 44:264–275. https://doi.org/10.1093/schbul/sbx055
Peralta V, Cuesta MJ (2011) Eugen Bleuler and the schizophrenias: 100 years after. Schizophr Bull 37:1118–1120. https://academic.oup.com/schizophreniabulletin/article/37/6/1118/1895092
McNally K (2016) Myth and forgetting: Bleuler’s four as. McMillan, London
Cocchi A, Lora A, Meneghelli A, La Greca E, Pisano A, Cascio MT, Preti A, Programma 2000 Team (2014) Sex differences in first-episode psychosis and in people at ultra-high risk. Psychiatry Res 215:314–322. https://doi.org/10.1016/j.psychres.2013.11.023
Azzali S, Pelizza L, Scazza I, Paterlini F, Garlassi S, Chiri LR, Poletti M, Pupo S, Raballo A (2022) Examining subjective experience of aberrant salience in young individuals at ultra-high risk (UHR) of psychosis: a 1-year longitudinal study. Schizophr Res 241:52–58. https://doi.org/10.1016/j.schres.2021.12.025
Pelizza L, Azzali S, Garlassi S, Scazza I, Paterlini F, Chiri LR, Poletti M, Pupo S, Raballo A (2019) Examining subjective experience of social cognition in early psychosis: validation of the Italian version of the GEOPTE scale in an adolescent and young adult clinical sample. J Psychopathol 25:220–230. https://old.jpsychopathol.it/wp-content/uploads/2019/12/06_Pelizza-1.pdf
Pelizza L, Leuci E, Landi G, Quattrone E, Azzali S, Pelosi A, Ceroni P, Soncini C, Daolio MC, Dall’Aglio R, Paulillo G, Pellegrini C, Raballo A, Pellegrini P (2020) The Personal Health Budget intervention model in early psychosis: preliminary findings from the Parma experience. J Psychopathol 26:209–217. https://doi.org/10.36148/2284-0249-359
Di Lisi A, Pelizza L (2023) Antipsychotic medication in individuals at Clinical High Risk for psychosis: what recommendations for clinicians? J Psychopathol 29:110–116. https://doi.org/10.36148/2284-0249-N331
Ficarelli ML, Troisi E, Vignali E, Artoni S, Franzini MC, Montanaro S, Andreoli MV, Marangoni S, Ciampà E, Erlicher D, Pupo S, Pelizza L (2021) Implementing individual and placement support for patients with severe mental illness: findings from the real world. J Psychopathol 27:71–80. https://doi.org/10.36148/2284-0249-346
Raballo A, Poletti M, Preti A (2020) Meta-analyzing the prevalence and prognostic effect of antipsychotic exposure in clinical high-risk (CHR): when things are not what they seem. Psychol Med 50:2673–2681. https://doi.org/10.1017/S0033291720004237
Pelizza L, Leuci E, Quattrone E, Azzali S, Paulillo G, Pupo S, Poletti M, Raballo A, Pellegrini P, Menchetti M (2023) Baseline antipsychotic prescription and short-term outcome indicators in individuals at clinical high-risk for psychosis: findings from the Parma At-Risk Mental States (PARMS) program. Early Interv Psychiatry 2023 May 16. https://doi.org/10.1111/eip.13434
Pelizza L, Di Lisi A, Leuci E, Quattrone E, Azzali S, Pupo S, Paulillo G, Pellegrini P, Menchetti M (2024) Subgroups of clinical high risk for psychosis based on baseline antipsychotic exposure: clinical and outcome comparisons across a 2-year follow-up period. Schizophr Bull March 29:sbae029. https://doi.org/10.1093/schbul/sbae029
Lee JH (2022) The listed, delisted, and sustainability of therapeutic medicines for dementia patients: the study is specific to South Korea. Naunyn-Schmiedebergs Arch Pharmacol 395:535–546. https://doi.org/10.1007/s00210-022-02209-3
Shaygan M, Sheibani Negad S, Motazedian S (2022) The effect of combined sertraline and positive psychotherapy on hopelessness and suicidal ideation among patients with major depressive disorder: a randomized controlled trial. J Posit Psychol 17:655–664. https://doi.org/10.1080/17439760.2021.1913636
Acknowledgements
For their facilitating technical and administrative support in the Pr-EP program, the authors gratefully acknowledge the “Early Psychosis Facilitators Group” members (Sabrina Adorni, Andrea Affaticati, Anahi Alzapiedi, Paolo Ampollini, Patrizia Caramanico, Maria Teresa Gaggiotti, Tiziana Guglielmetti, Mauro Mozzani, Matteo Rossi, Lucilla Maglio, Matteo Tonna, Fabio Vanni and Matteo Zito) and the “Quality Staff Group” members (Patrizia Ceroni, Stefano Giovanelli, Leonardo Tadonio) of the Parma Department of Mental Health and Pathological Addictions. The authors also wish to thank all the patients and family members who actively participated to the PARMS program.
Funding
This research received no specific grant from any funding agencies in the public, commercial or not-for-profit sectors. The “Parma At-Risk Mental States” (PARMS) program was partly financed through a special, treatment-oriented regional fund (“Progetto Esordi Psicotici della Regione Emilia Romagna”) from 2013 to 2018.
Open access funding provided by Alma Mater Studiorum - Università di Bologna within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
Study conception and design: Lorenzo Pelizza and Emanuela Leuci; Literature search and analysis: Arianna Biancalani, Michele Occhionero and Simona Pupo; Data collection: Emanuela Leuci, Emanuela Quattrone and Silvia Azzali: Formal analysis and investigation: Lorenzo Pelizza; Writing – original draft preparation: Arianna Biancalani, Michele Occhionero and Lorenzo Pelizza; writing – review and editing: all authors.
Corresponding author
Ethics declarations
Ethical approval
Local ethical approval was obtained for the research (AVEN Ethics Committee: protocol n. 559/2020/OSS*/AUSLPR). This investigation was conducted in accordance with the ethical standards of the 1964 Declaration of Helsinki and its later amendments.
Consent to participate
All individuals and their parents (if minors) gave their written informed consent prior to their inclusion in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Biancalani, A., Occhionero, M., Leuci, E. et al. Disorganization in individuals at clinical high risk for psychosis: psychopathology and treatment response. Eur Arch Psychiatry Clin Neurosci (2024). https://doi.org/10.1007/s00406-024-01855-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00406-024-01855-3