Abstract
The past 20 years of research on EEG microstates has yielded the hypothesis that the imbalance pattern in the temporal dynamics of microstates C (increased) and D (decreased) is specific to schizophrenia. A similar microstate imbalance has been recently found in obsessive–compulsive disorder (OCD). The aim of the present high-density EEG study was to examine whether this pathological microstate pattern is co-specific to schizophrenia and OCD. We compared microstate temporal dynamics using Bayesian analyses, transition probabilities analyses and the Topographic Electrophysiological State Source-Imaging method for source reconstruction in 24 OCD patients and 28 schizophrenia patients, respectively, free of comorbid psychotic and OCD symptoms, and 27 healthy controls. OCD and schizophrenia patients exhibited the same increased contribution of microstate C, decreased duration and contribution of microstate D and greater D → C transition probabilities, compared with controls. A Bayes factor of 4.424 for the contribution of microstate C, 4.600 and 3.824, respectively, for the duration and contribution of microstate D demonstrated that there was no difference in microstate patterns between the two disorders. Source reconstruction further showed undistinguishable dysregulations between the Salience Network (SN), associated with microstate C, and the Executive Control Network (ECN), associated with microstate D, and between the ECN and cognitive cortico-striato-thalamo-cortical (CSTC) loop in the two disorders. The ECN/CSTC loop dysconnectivity was slightly worsened in schizophrenia. Our findings provide substantial evidence for a common aetiological pathway in schizophrenia and OCD, i.e. microstate co-specificity, and same anomalies in salience and external attention processing, leading to co-expression of symptoms.


Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author (BT) upon reasonable request.
References
Sui J, Jiang R, Bustillo J, Calhoun V (2020) Neuroimaging-based individualized prediction of cognition and behaviour for mental disorders and health: methods and promises. Biol Psychiatry 88:818–828. https://doi.org/10.1016/j.biopsycj.2020.02.016
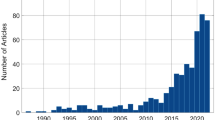
Michel CM, Koenig T (2018) EEG microstates as a tool for studying the temporal dynamics of whole-brain neuronal networks: A review. Neuroimage. https://doi.org/10.1016/j.neuroimage.2017.11.062
Lehmann D, Pal OH (1987) EEG alpha map series: brain microstates by space-oriented adaptive segmentation. Electroencephalogr Clin Neurophysiol. https://doi.org/10.1016/0013-4694(87)90025-3
Koenig T, Lehmann D, Merlo MC, Koukkou KK (1999) Deviant EEG brain microstate in acute, neuroleptic-naïve schizophrenics at rest. Eur Arch Psychiatry Clin Neurosci 249:205–211. https://doi.org/10.1007/s004060050088
Lehmann D, Faber PL, Galderisi S, Hermann WH, Kinoshita T, Koukkou M, Mucci A, Pascual-Marqui RD, Saito N, Wackerman J, Winterer G, Koenig T (2005) EEG microstate duration and syntax in acute, medication-naïve, first-episode schizophrenia: a multi-center study. Psychiatry Res 138:141–156. https://doi.org/10.1016/j.psychresns.2004.05.007
Da Cruz JR, Favrod O, Roinishvili M, Chkonia E, Brand A, Mohr C, Figueiredp P, Herzog M (2020) EEG microstates are candidate endophenotype for schizophrenia. Nat Commun 11:3086. https://doi.org/10.1038/s41467-020-16914-1
Schwab S, Koenig T, Morishima Y, Dierks T, Federspiel A, Jann K (2015) Discovering frequency sensitive thalamic nuclei from EEG microstate informed resting state fMRI. Neuroimage 118:386–375. https://doi.org/10.1016/j.neuroimage.2015.06.001
Custo A, Van de Ville D, Wells WM, Tomescu MI, Brunet D, Michel CM (2017) Electroencephalographic Resting-State Networks: Source Localizations of Microstates. Brain Connect 7:671–682. https://doi.org/10.1089/brain.2016.0476
Thirioux B, Langbour N, Bokam P, Renaudin L, Wassouf I, Harika-Germaneau G, Jaafari N (2023) Microstates imbalance is associated with a functional dysregulation of the Resting-State Networks in Obsessive–Compulsive Disorder: a high-density electrical neuroimaging study using the TESS method. Cereb Cortex 33:2593–2611. https://doi.org/10.1096/cercor/bhac.229
Britz J, Van de Ville D, Michel CM (2010) BOLD correlates of EEG topography reveal rapid resting-state networks dynamics. Neuroimage 52:1162–1170. https://doi.org/10.1016/j.neuroimage.2010.02.052
Menon V (2011) Large-scale brain networks and psychopathology: a unifying triple network model. Trends Cogn Sci 15:483–506. https://doi.org/10.1016/j.tics.2011.08.003
Rieger K, Diaz Hernandez L, Baenninger A, Koenig T (2016) 15 years of microstate research in schizophrenia – where are we? A meta-analysis Front Psychiatry 7:22. https://doi.org/10.3389/fpsyt.2016.00022
Tomescu M, Rihs TA, Becker R, Britz J, Custo A, Grouiller F, Schneider M, Debbané M, Eliez S, Michel CM (2014) Deviant dynamics of EEG resting state pattern in 22q11.2 deletion syndrome adolescents: A vulnerability marker of schizophrenia? Schizophr Res 157:175–181. https://doi.org/10.1016/J.schres.2014.05.036
Tait L, Tamagnini F, Stothart G, Barvas E, Monaldini C, Frusciante R, Volpini M, Guttman S, Coulthard E, Brown TJ, Kazanina N, Goodfellow M (2020) EEG microstates complexity for aiding early diagnosis of Alzheimer’s disease. Sci Rep 10:17627. https://doi.org/10.1038/s41598-020-74790-7
Murphy M, Whitton AE, Deccy S, Ironside ML, Rutherford A, Beltzer M, Sacchet M, Pizzaglia DA (2020) Abnormalities in electroencephalographic microstates are state and trait markers of major depressive disorder. Neuropsychopharmacology 45:2030–2037. https://doi.org/10.1038/s41386-020-0749-1
Tomescu M, Rihs TA, Roinishvili M, Karahanoglu FI, Schneider M, Menghetti S, Van De Ville D, Brand A, Chkonia, E, Eliez S, Herzog MH, Michel CM, Cappe C (2015) Schizophrenia patients and 22q11.2 deletion syndrome adolescents at risk express the same deviant pattern of resting state EEG microstates: a candidate endophenotype of schizophrenia. Schizophr Res Cogn 10.1016.j.scog.2015.04.005.
Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC (1998) The Mini-International Neuropsychiatric Interview (M.I.N.I): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 59:22–33
Goodman WK, Price LH, Rasmussen SA, Mazure C, Delgado P, Heninger GR, Charney DS (1989) The Yale–Brown Obsessive–Compulsive Scale. II Validity Arch Gen Psychiatry 46:1012–1016. https://doi.org/10.1001/archpsyc.199.01810110054008
Kay SR, Fiszbein A, Opler LA (1987) The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull 13:261–276. https://doi.org/10.1093/schbul/13.2.261
Ruggeri P, Meziane HB, Koenig T, Brandner CA (2019) A fine-grained time course investigation of brain dynamics during conflict monitoring. Sci Report 9:3667. https://doi.org/10.1038/s41598-019-40277-3
Perrin F, Pernier J, Bertrand O, Giard MH, Echallier JF (1987) Mapping of scalp potentials by surface spline interpolation. Electroencephalogr Clin Neurophysiol 66:75–81. https://doi.org/10.1016/0013-4694(87)901414-6
Koenig T, Kottlow M, Stein M, Melie-García L (2011) Ragu: a free tool for the analysis of EEG and MEG event-related scalp field data using global randomization statistics. Comput Intell Neurosci. https://doi.org/10.1155/2011/938925
Koenig T, Stein M, Grieder M, Kottlow M (2014) A tutorial on data-driven methods for statistically assessing ERP topographies. Brain Topogr 27:72–83. https://doi.org/10.1007/s10548-013-0310-1
Delorme A, Makeig S (2004) EEGLAB: an open source toolbox for analysis of single-trial EEG dynamics including independent component analysis. J Neurosci Methods 134:9–21. https://doi.org/10.1016/j.neumeth.2003.10.009
Pascual-Marqui RD, Michel CM, Lehmann D (1995) Segmentation of brain electrical activity into microstates: model estimation and validation. IEEE Trans Biomed Eng 42:658–665. https://doi.org/10.1109/10.391164
Lehmann D, Skrandies W (1980) Reference-free identification of components of checkerboard-evoked multichannel potential fields. Electrocencephalogr Clin Neurophysiol 48:609–621. https://doi.org/10.1016/0013-4694(80)90419-8
Koenig T, Prichep L, Lehmann D, Sosa PV, Braeker E, Kleinlogel H, Isenhart R, John ER (2002) Millisecond by millisecond, year by year: normative EEG microstates and developmental stages. Neuroimage 16:41–48. https://doi.org/10.1006/nimg.2002.1070
Quitana DS, Williams DR (2018) Bayesian alternatives for common null-hypothesis significance tests in psychiatry: a non-technical guide using JASP. BMC Psychiatry 18:178. https://doi.org/10.1186/s12888-018-1761-4
Pascual-Marqui RD (2002) Standardized low-resolution brain electromagnetic tomography (sLORETA): technical details. Methods Find Exp Clin Pharmacol 24:5–12
Michel CM, Murray MM, Lantz G, Gonzales G, Spinelli L, Grave de Peralta R (2004) EEG source imaging. Clin Neurophysiol 115:2195–2222. https://doi.org/10.1016/j.clinph.2004.06.001
Brodbeck V, Kuhn A, von Wegner F, Morzelewski A, Tagliazucchi E, Borisov S, Michel CM, Laufs H (2012) EEG microstates of wakefulness and NREM sleep. Neuroimage 62:2129–2139. https://doi.org/10.1016/j.neuroimage.2012.05.060
Meier SM, Petersen L, Pedersen MG, Arendt MC, Nielsen PR, Mattheisen M, Mors O, Mortensen PB (2014) Obsessive–compulsive disorder as a risk factor for schizophrenia: a nationwide study. JAMA Psychiat 71:1215–1221. https://doi.org/10.1001/jamapsychiatry.2014.1011
Tibbo P, Warnecke L (1999) Obsessive–compulsive disorder in schizophrenia: epidemiological and biologic overlap. J Psychiatry Neurosci 24:15–24
Katayama H, Gianotti LRR, Isotani T, Faber PL, Sasada K, Kinoshita T, Lehmann D (2007) Classes of multichannel EEG microstates in light and deep hypnotic conditions. Brain Topogr 20:7–14. https://doi.org/10.1007/s10548-007-0024-3
Kindler J, Hubl D, Strik WK, Dierks T, Koenig T (2011) Resting-state EEG in schizophrenia: auditory verbal hallucinations are related to shortening of specific microstates. Clin Neurophysiol 112:1179–1182. https://doi.org/10.1016/j.clinph.2010.10.042
Gottesman II, Gould TD (2003) The endophenotype concept in psychiatry: etymology and strategic intentions. Am J Psychiatry 160:636–645. https://doi.org/10.1176/appi.ajp.160.4.636
Nishida K, Morishima Y, Yoshimura M, Isotani T, Irisawa S, Jann K, Dierks T, Strik W, Kinoshita T, Koenig T (2013) EEG microstates associated with salience and frontoparietal networks in frontotemporal dementia, schizophrenia, and Alzheimer’s disease. Clin Neurophysiol 124:1106–1114. https://doi.org/10.1016/j.clinph.2013.01.005
Kikuchi M, Koenig T, Wada Y, Higashima M, Koshino Y, Strik W, Dierks T (2007) Native EEG and treatment effects in neuroleptic-naïve schizophrenic patients: time and frequency domain approaches. Schizophr Res 97:163–172. https://doi.org/10.1016/j.schres.2007.07.012
Stahl SM (2013) Stahl’s Essential Psychopharmacology. Cambridge University Press, Cambridge
Yoshimura M, Koenig T, Irisawa S, Isotani T, Yamada K, Kikuchi M, Okugawa G, Yagyu T, Kinoshita T, Strik W, Strik W, Dierks T (2007) A Pharmaco-EEG study on antipsychotic drugs in healthy volunteers. Psychopharmacology 191:995–1004. https://doi.org/10.1007/s00213-007-0737-8
Mackintosh A, Borgwardt S, Studerus E, Riecher-Rössler A, de Bock R, Andreou C (2020) EEG microstates differences in medicated vs. medication-naïve first-episode psychosis patients. Front Psychiatry https://doi.org/10.3389/fpsyt.2020.600606
Achim AM, Maziade M, Raymond E, Olivier D, Mérette C, Roy MA (2011) How prevalent are anxiety disorders in schizophrenia? A meta-analysis and critical review on a significant association. Schizophr Bull 37:811–821. https://doi.org/10.1093/schbul/sbp148
Buckley PF, Miller BJ, Lehrer DS, Castle DJ (2009) Psychiatric comorbidities and schizophrenia. Schizophr Bull 35:383–402. https://doi.org/10.1093/schbul/sbn135
Lykouras L, Alevizos B, Michalopoulou P, Rabavilas A (2003) Obsessive–compulsive symptoms induced by atypical antipsychotics. A review of the reported cases. Prog Neuropsychopharmacol Bio Psychiatry 27:333–346. https://doi.org/10.1016/S0278-5846(03)00039-3
Lopes da Silva F (1991) Neural mechanisms underlying brain waves: from neural membranes to networks. Electroencephalogr Clin Neurophysiol. https://doi.org/10.1016/0013-4694(91)90044-5
Gross-Isseroff R, Hermesch H, Zohar J, Weizman A (2003) Neuroimaging communality between schizophrenia and obsessive compulsive disorder: a putative basis for schizo-obsessive disorder? World J Biol Psychiatry 4:129–134. https://doi.org/10.1080/15622970310029907
Gürsel DA, Avram M, Sorg C, Brandl F, Koch K (2018) Frontoparietal areas link impairments of large-scale intrinsic brain networks with aberrant fronto-striatal interactions in OCD: a meta-analysis of resting-state functional connectivity. Neurosci Biobehav Rev 87:151–160. https://doi.org/10.1016/j.neurobiorev.2018.01.016
Moritz S, Peters MJ, Laroi F, Lincoln TM (2010) Metacognitive beliefs in obsessive–compulsive patients: a comparison with healthy and schizophrenia participants. Cogn Neuropsychiatry 15:531–548. https://doi.org/10.1080/13546801003783508
Forbes MK, Sunderland M, Rapee RM, Batterham PJ, Calear AL, Carragher N, Ruggero C, Zimmerman M, Baillie AJ, Lynch SJ, Mewton L, Slade T, Krueger RF (2021) A detailed hierarchical model of psychopathology: from individuals symptoms up to the general factor of psychopathology. Clin Psychol Sci 9:139–168. https://doi.org/10.1177/2167702620954799
Costas J, Carrera N, Alonso P, Gurriarán X, Segalás C, Real E, Lopez-Sola C, Mas S, Gasso P, Domenech L, Morell M, Quintela I, Lazaro L, Menchon JM, Estivill X, Carracedo A (2016) Exon-focused genome-wide association study of obsessive–compulsive disorder and shared polygenic risk with schizophrenia. Transl Psychiatry. https://doi.org/10.1038/tp.2016.34
Gürsel DA, Reinholz L, Bremer B, Schmitz-Koep B, Franzmeier N, Avram M, Koch K (2020) Frontoparietal and salience network alterations in obsessive–compulsive disorder: insights from independent component and sliding time window analyses. J Psychiatry Neurosci 45:214–221. https://doi.org/10.1503/jpn.190038
Posner J, Marsh R, Maia TV, Peterson BS, Gruber A, Simpson HB (2014) Reduced functional connectivity within the limbic cortico-striato-thalamo-cortical loop in unmedicated adults with obsessive–compulsive disorder. Hum Brain Mapp 35:2852–2860. https://doi.org/10.1002/hbm.22371
Rotgé JY, Guehl D, Dilharreguy B, Tignol J, Bioulac B, Allard M, Burbaud P, Aouizerate B (2009) Meta-analysis of brain volume changes in obsessive–compulsive disorder. Biol Psychiatry 65:75–83. https://doi.org/10.1016/j.biopsych.2008.06.019
White TP, Joseph V, Francis ST, Liddle P (2010) Aberrant salience network (bilateral insula and anterior cingulate cortex) connectivity during information processing in schizophrenia. Schizophr Res 123:105–115. https://doi.org/10.1016/j.schres.2010.07.020
Dong D, Wang Y, Chang X, Luo C, Yao D (2018) Dysfunction of large-scale brain networks in schizophrenia: a meta-analysis of resting-state functional connectivity. Schizophr Bull 44:168–181. https://doi.org/10.1093/schbul/sbx034
Menon V, Uddin LQ (2010) Saliency, switching, attention and control: a network model of insula function. Brain Struct Funct 214:655–667. https://doi.org/10.1007/s00429-010-0262-0
Lavallé L, Brunelin J, Bation R, Mondino M (2020) Review of source-monitoring in obsessive–compulsive disorder. World J Psychiatry 10:12–20. https://doi.org/10.5498/wjp.v10.i2.12
O’Connor K, Aardema F (2003) Fusion or confusion in obsessive–compulsive disorder. Psychol Rep 93:2227–2232. https://doi.org/10.2466/pr0.2003.93.1.227
Rotgé JY, Langbour N, Guehl D, Bioulac B, Jaafari N, Allard M, Aouizerate B, Burbaud P (2010) Gray matter alterations in obsessive–compulsive disorder: an anatomic likelihood estimation meta-analysis. Neuropsychopharmacology 35:686–691. https://doi.org/10.1038/npp.2009.175
Kapur S (2003) Psychosis as a state of aberrant salience: a framework linking biology, phenomenology, and pharmacology in schizophrenia. Am J Psychiatry 160:13–23. https://doi.org/10.1176/appi.ajp.160.1.13
Menzies L, Chamberlain SR, Laird AR, Thelen SM, Sahakian BJ, Bullmore ET (2007) Integrative evidence from neuroimaging and neuropsychological studies of obsessive–compulsive disorder: the orbitofronto-striatal model revisited. Neurosci Biobehav Rev 10.1016.j.neubiorev.2007.09.005.
Voegler R, Becker MI, Nitsch A, Straube MWHRT (2016) Aberrant network connectivity during error processing in patients with schizophrenia. J Psychiatry Neurosci 41:E3-12. https://doi.org/10.1503/jpn.150092
Fan J, Gan J, Liu W, Zhong M, Liao H, Zhang H, Jinyao Yi, Chan RCK, Tan C, Zhu X (2018) Resting-state default mode network related functional connectivity is associated with sustained attention deficits in schizophrenia and obsessive–compulsive disorder. Front Behav Neurosci 12:319. https://doi.org/10.3389/fnbeh.2018.00319
Zermatten A, Van der Linden M, Laroi F, Ceschi G (2006) Reality monitoring and motor memory in checking-prone individuals. J Anxiety Disord 20:580–596. https://doi.org/10.1016/j.janxdis.2005.08.001
Rehn S, Eslick GD, Brakoulias V (2018) A meta-analysis of the effectiveness of different cortical targets used in repetitive transcranial magnetic stimulation (rTMS) for the treatment of obsessive–compulsive disorder (OCD). Psychiatry Q 89:645–665. https://doi.org/10.1007/s11126-018-9566-7
Bonini F, Burle B, Liégeois-Chauvel C, Régis J, Chauvel P, Vidal F (2014) Action monitoring and medial frontal cortex: leading role of supplementary motor area. Science 343:888–891. https://doi.org/10.1126/science.1247412
Ning Y, Zheng S, Feng S, Zhang B, Jia H (2021) Potential locations for non-invasive brain stimulation in treating schizophrenia: a resting-state functional connectivity analysis. Front Neurol. https://doi.org/10.3389/fneur.2021.766736
Harika-Germaneau G, Rachid F, Chatard A, Lafay-Chebassier C, Solinas M, Thirioux B, Millet B, Langbour JN (2019) Continuous theta burst stimulation over the supplementary motor area in refractory obsessive–compulsive disorder treatment: A randomized sham-controlled trial. Brain Stimul 12:1565–1571. https://doi.org/10.1016/j.brs.2019.07.019
Harika-Germaneau G, Heit D, Chatard A, Thirioux B, Langbour N, Jaafari N (2020) Treating refractory obsessive–compulsive disorder with transcranial direct current stimulation: an open label study. Brain Behav. https://doi.org/10.1002/brb3.1648
Strelets V, Faber PL, Golikova J,Novototsky-Vlasov V, Koenig T, Gianotti LRRR, Gruzelier JH, Lehmann D (2003) Chronic schizophrenics with positive symptomatology have shortened EEG microstate durations. Clin Neurophysiology 10.1016./s1388-2457(03)00211-6.
Acknowledgements
The authors thank Carole Chevalier and Maxime Rollin for helping with patients’ recruitment, and Nicolas Bordères and Ryadh Benslimane for helping with patients’ evaluation
Funding
This work was supported by recurrent internal funds from the Centre Hospitalier Henri Laborit (Poitiers, France) and Agence Régionale de Santé en Nouvelle Aquitaine (France).
Author information
Authors and Affiliations
Contributions
Conceptualization: BT; data collection: BT, NL; methodology: BT, NL; data analyses: BT, NL, PB; statistical analyses: BT, NL, PB; clinical evaluation: NGB, CW, PML, GHG, BT; writing (original draft): BT; visualization: IW, DD; supervision: BT, NL, NJ; validation: BT, NL, NJ.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing financial or non-financial interests.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Thirioux, B., Langbour, N., Bokam, P. et al. EEG microstate co-specificity in schizophrenia and obsessive–compulsive disorder. Eur Arch Psychiatry Clin Neurosci 274, 207–225 (2024). https://doi.org/10.1007/s00406-023-01642-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-023-01642-6