Abstract
Psychiatric symptoms have been frequently reported in patients affected by COVID-19, both as new occurring and recurrences of pre-existing diseases. Depressive symptoms are estimated to affect at least 30% of patients following infection, with specific physical and cognitive features and relevant immune-inflammatory alterations. This study aimed to retrospectively characterize post-COVID-19 first-onset and recurrent major depressive episodes (MDE) and to evaluate the effects of antidepressants on physical and cognitive correlates of depression, in addition to mood, anxiety, and underlying inflammatory status. We evaluated 116 patients (44.8% males, 51.1 ± 17 years) with post-COVID-19 first-onset (38.8%) and recurrent (61.2%) MDE at baseline and after one- and three-month treatment with antidepressants (31% SSRIs, 25.9% SNRIs, 43.1% others). We assessed sociodemographic and clinical features and psychopathological dimensions through: Hamilton Depression and Anxiety Rating Scales; Short Form-36 Health Survey Questionnaire; Perceived Deficits Questionnaire-Depression 5-items. The systemic immune-inflammatory index was calculated to measure inflammation levels. Alongside the reduction of depression and anxiety (p < 0.001), physical and cognitive symptoms improved (p < 0.001) and inflammatory levels decreased (p < 0.001) throughout treatment in both groups. Post-COVID-19 recurrent MDE showed a significantly more severe course of physical and cognitive symptoms and persistently higher levels of inflammation than first-onset episodes. Antidepressants proved to be effective in both post-COVID-19 first-onset and recurrent MDE. However, a sustained inflammatory status might blunt treatment response in patients with recurrent depression in terms of physical correlates and cognition. Therefore, personalized approaches, possibly involving combinations with anti-inflammatory compounds, could promote better outcomes in this clinical population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has largely affected mental health worldwide [1], and the long-term sequelae of SARS-CoV-2 infection have increasingly raised attention because of their high prevalence and healthcare and socioeconomic impact [2]. It is estimated that about one-third of patients recovering from COVID-19 display a wide range of symptoms enduring after the acute phase, with frequent neuropsychiatric manifestations [3,4,5].
A bidirectional relationship between COVID-19 and psychiatric diseases has been suggested, with SARS-CoV-2 infection predisposing to subsequent psychiatric symptoms and previous diagnoses of mental illness being a risk factor for worse COVID-19 outcomes, higher mortality rates, and long-term residual symptoms [6, 7].
Depressive symptoms are among the most frequently reported sequelae of infection, affecting approximately 30–40% of patients at different follow-ups [8], and are characterized by prominent cognitive and physio-somatic correlates, with a detrimental impact on overall functioning and quality of life [9]. Specifically, post-COVID-19 depressive symptoms have been found to strongly correlate with cognitive impairments (e.g., attention/concentration, memory, and processing speed) and fatigue, and all these features were associated with increased inflammatory markers at least at baseline assessment [10].
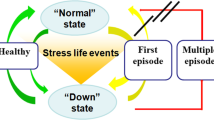
Among the mechanisms underlying COVID-19-related neuropsychiatric alterations, such as the indirect damage to the nervous system and/or a potential direct neurotropism of SARS‑CoV‑2 [11, 12], the virus-induced systemic immune-inflammatory response has been proposed as the main underpinning of post-COVID-19 long-term symptomatology, including depression and anxiety [5]. Growing evidence described the association between mood disorders and immune-inflammatory activation manifested through increased levels of inflammatory indexes [13], and inflammatory processes have been, to some extent, correlated with recurrence of episodes [14,15,16]. Thus, according to the involvement of neuroinflammation in the pathophysiology of mental illnesses, it has been proposed that a psychiatric history could further promote inflammation during and after SARS-CoV-2 infection and result in more severe depressive and anxious symptoms and a greater unlikelihood of recovery in the short time [6].
Immune-modulatory effects have been reported for most antidepressants and emerging literature described the anti-inflammatory and antiviral properties of these compounds in the treatment of SARS-CoV-2 infection [17, 18]. Consistently, several antidepressants were shown to be effective in treating post-COVID-19 depression at short- and medium-term follow-up [17, 19], with similar improvements in both first-onset and recurrent depressive episodes [20]. These observations led to hypothesize that response to antidepressants in this clinical population could be mediated, at least in part, by their ability to modulate neuroinflammation triggered by SARS-CoV-2 [9].
Despite increasing evidence on post-COVID-19 depression, less is known about the clinical course and treatment response of physical and cognitive correlates that represent a critical issue in the management of this condition and hinder full functional recovery [4, 9, 10]. Also, whether the course of post-COVID-19 depression, especially of physical and cognitive symptoms, differs between subjects with and without a psychiatric history still needs further clarification [6].
In this study, we assumed that subjects diagnosed with post-COVID-19 recurrent depression would display more severe clinical features than patients at their first occurrence. Also, we hypothesized that first-onset and recurrent episodes would differentially respond to pharmacological treatment. Therefore, we aimed to retrospectively investigate differences in the symptomatic course and the response to antidepressants between patients with post-COVID-19 first-onset and recurrent major depressive episodes (MDE), primarily focusing on physical and cognitive symptoms. The underlying inflammatory levels were also investigated.
Methods
Participants
Patients referred to the Fondazione Policlinico Universitario “Agostino Gemelli” IRCCS in Rome between April 2020 and June 2022 were retrospectively evaluated. Inclusion criteria were: age ≥ 18 years; fluency in spoken and written Italian; primary diagnosis of a major depressive episode (MDE) according to DSM-5 criteria (APA, 2013) emerged within the first 6 months following SARS-CoV-2 infection as confirmed by a positive polymerase chain reaction test; at least moderate symptoms according to Hamilton Depression Rating Scale (HDRS) total score ≥ 14 (APA, 2000); at least a three-months treatment with a target dose of antidepressant, flexibly dosed. Patients with recurrent MDE were considered eligible if being recovered from the last episode when contracting SARS-CoV-2 infection. Exclusion criteria were: current primary psychiatric diagnoses other than MDE; psychotic features; current alcohol and/or substance abuse, except for smoking; organic brain syndromes, neurocognitive disorders, or significant cognitive impairment based on a Mini-Mental State Examination (MMSE) score < 26; any major medical conditions known to contribute to systemic inflammation and that were not under maintenance pharmacological treatment (i.e., not in remission and/or with significant alterations of monitoring parameters).
Data collection: psychometric assessment and clinical measurements
Data were obtained from measurements and assessments performed at baseline and after 1 and 3 months of treatment (endpoint) according to routine clinical practice.
Physical symptomatology was evaluated through a combination of items of HDRS [21] and Hamilton Anxiety Rating Scale, HARS [22] referred to as “Physical Symptoms”, and subscales of Short Form-36 Health Survey Questionnaire, SF-36 [23].
The physical symptoms of depression were assessed through items 4, 5, 6 (early, middle, late insomnia), 11 (somatic anxiety), 12 (gastrointestinal), 13 (general somatic, including muscular pain, headache, and lack of energy), 14 (genital—both loss of libido and menstrual disturbances), and 16 (loss of weight) of HDRS, and 7 (muscular pain), 8 (sensory), 9 (cardiovascular), 10 (respiratory), 11 (gastrointestinal), 12 (genitourinary) and 13 (autonomic) of HARS, respectively [24].
SF-36 is a 36-item, self-reported survey of patients’ health consisting of eight scaled sections, each one rated from 0 (worst health) to 100 (best health): bodily pain (BP); general health perceptions (GHP); mental health (MH); physical functioning (PF); role emotional, i.e., limitation due to emotional problems (RE); role physical, i.e., limitation due to physical health problems (RP); social functioning (SF); vitality (VT). SF-36 subdomain scores were aggregated into the summary measure physical component score (PCS) to evaluate physical symptomatology, with higher scores indicating less disability and a cut-off lower than 50 indicative of poor functioning [25,26,27].
Cognitive performance was assessed through the Perceived Deficits Questionnaire-Depression 5-items, PDQ-D5 [28]. PDQ-D5 served as a subjective measure of cognition, with the total score ranging 0–20, wherein higher scores indicate greater impairment in patients with depression in the following domains: attention/concentration, planning/organization, retrospective and prospective memory.
Additional assessment included the evaluation of depressive symptoms and anxiety levels through the clinician-rated 17-item HDRS and HARS. Patients were considered responders when obtaining an improvement of at least 50% of HDRS baseline scores and remitters when achieving a total score ≤ 7 at the endpoint. Mood relapses were defined as a new exacerbation of depressive symptoms (HDRS total score ≥ 14) after initial improvement.
Finally, white blood cell count was extracted from charts and systemic immune-inflammatory index (SII, i.e., platelets X neutrophils/lymphocytes) was calculated to measure inflammation levels before and after one and three months of treatment [10].
Statistical analysis
We subdivided our sample into patients with post-COVID-19 first-onset and recurrent MDE. Our primary outcome was to evaluate the effect of antidepressant treatments on physical symptomatology and cognitive performances with potential differences between post-COVID-19 first-onset and recurrent MDE. Secondary outcome measures included the course of depressive symptoms and anxiety levels alongside changes in inflammatory indexes during the treatment period and comparisons between the two groups of patients.
Descriptive data were summarized as the number of patients and percentage (%) or mean ± standard deviation (M ± SD) for categorical and continuous variables, respectively. Comparisons between groups were obtained using independent samples t test for continuous variables or Chi-square test/Fisher’s exact test for dichotomous variables. The outcome measures—the mean changes from baseline to 1 and 3 months of each efficacy variable—were analyzed using a mixed model for repeated measurements (MMRM), including the baseline score as a continuous covariate, and time, psychiatric diagnosis (first-onset vs. recurrent MDE), the baseline score-by-time interaction, and diagnosis-by-time interaction as fixed effects, based on all available observations. Analyses were performed on all patients with at least one valid post-baseline assessment of the variables (full-analysis set, FAS). A significance level of p < 0.05 was used for each test.
All analyses were performed using IBM SPSS Statistics for Windows, v. 25 (IBM Corp., Armonk, New York, USA).
Results
A total of 116 Caucasian subjects (51.1 ± 17 years old) were included. Seventy-one (61.2%) patients had been diagnosed with a recurrent MDE and 45 (38.8%) with a first-onset MDE following COVID-19. Patients were treated for three months with the following classes of antidepressants: SSRIs: 31%; SNRIs: 25.9%; others: 43.1%. Concomitant psychopharmacological treatment with mood stabilizers/anticonvulsants, second-generation antipsychotics, or sedative-hypnotics/anxiolytics (variously combined) was assumed by 63.8% of patients, and continuous psychoeducational support was provided. No between-groups differences were detected for antidepressants (p = 0.096) nor for other psychopharmacotherapies (p = 0.062).
Most patients (64.6%) in the sample had been vaccinated for SARS-CoV-2 when contracting the infection and all subjects developed a symptomatic COVID-19 (mild, moderate, or severe according to signs and symptoms referred by patients and rated by clinicians at the time of the infection following WHO recommendations). Compared to post-COVID-19 recurrent MDE, patients with first-onset affective episodes were on average less vaccinated (54.3 vs. 70.7%) and showed a moderate-to-severe course of COVID-19 (71.8 vs. 34.4%), with higher rates of pharmacotherapies and hospitalization, including intensive care units’ admissions.
Sociodemographic, clinical, and psychometric characteristics are summarized in Table 1.
At the endpoint, data were available for 94 patients. Results from MMRM for each efficacy variable are reported hereafter and in Table 2. Means ± SD for all variables at each time point is summarized in Table S1 (Online Resource 1).
Primary outcome measures
Physical symptomatology significantly reduced throughout treatment in both groups as rated by HDRS and HARS “Physical Symptoms” subscales and SF-36 PCS (Table 2).
No significant differences in HDRS Physical Symptoms were found between post-COVID-19 first-onset and recurrent MDE in the overall scores (mean difference: − 0.265 ± 0.29, p = 0.369) nor at given time-points, despite patients with recurrent MDE displaying higher mean scores than first MDE at one-month follow-up (3.87 ± 0.25 vs. 3.72 ± 0.39) and at the endpoint (1.57 ± 0.22 vs. 0.95 ± 0.36).
Conversely, the two groups significantly differed in overall HARS Physical Symptoms scores (mean difference: − 1.43 ± 0.39, p = 0.002) and at one and three months of treatment (Table 2), with post-COVID-19 recurrent MDE showing higher mean scores than first-onset MDE at both time-points (one-month follow-up: 5.27 ± 0.32 vs. 3.17 ± 0.5; endpoint: 1.97 ± 0.29 vs. 0.17 ± 0.46) (Fig. 1a).
Changes of HARS Physical Symptoms (a), SF-36 PCS (b), PDQ-D5 (c) and SII (d) scores throughout treatment in post-COVID-19 first-onset and recurrent MDE. Changes were always significant over time, with significant differences between groups at given time points (see Table 2)
Improvement in physical symptomatology assessed by SF-36 PCS was significant throughout treatment in both groups (p < 0.001). We observed significant differences between post-COVID-19 first-onset and recurrent MDE in the overall scores (mean difference: 3.63 ± 0.89, p < 0.001) and at the endpoint (Table 2), with patients with recurrent episodes showing lower mean scores than first-onset episodes at both time-points (43.9 ± 0.83 vs. 48.8 ± 1.35; 47.4 ± 0.73 vs. 52.9 ± 1.15) (Fig. 1b).
Cognitive performance improvements were detected by PDQ-D5 (p < 0.001) with significant differences between groups in overall scores (− 1.34, p = 0.017) and at the endpoint (Table 2). Mean PDQ-D5 scores were higher in the recurrent group both at one-month (7.73 ± 0.38 vs. 6.23 ± 0.68) and three-month treatment (5.46 ± 0.36 vs. 2.98 ± 0.63) (Fig. 1c).
Secondary outcome measures
Depressive symptoms significantly decreased (p < 0.001) without differences between groups in overall scores (− 0.55, p = 0.435) and at given time-points (Table 2). After one month of treatment, 1 (1.6%) and 4 (6.5%) patients were classified as remitters and responders, respectively, while 22 (23.4%) had a significant response and 68 (71.9%) reached remission at the endpoint. Only 4 (4.7%) patients were classified as non-responders after three months. No patient experienced a mood relapse throughout treatment.
Improvements in anxiety levels were significant as indicated by mean HARS total score reduction (p < 0.001), with overall significant differences between patients with first-onset and recurrent episodes (mean difference: − 1.28, p = 0.048) and higher mean scores in patients with recurrences at one-month (14.45 ± 0.51 vs. 12.37 ± 0.79) and three-months follow-up (6.27 ± 0.46 vs. 4.66 ± 0.73). However, no significant between-group differences were found at given time-points (Table 2).
Inflammatory levels assessed through SII had a significant reduction throughout treatment (p < 0.001) and significant differences between groups were found in the overall score (first-onset vs. recurrent MDE mean difference: − 122, p = 0.002) and at endpoint (Table 2). Post-COVID-19 recurrent MDE displayed higher SII values at both time-points (467 ± 47.3 vs. 281 ± 41.7; 402 ± 42.5 vs. 218 ± 39.8) (Fig. 1d).
Discussion
In this retrospective study, patients with both post-COVID-19 first-onset and recurrent MDE obtained a significant reduction of physical and cognitive correlates of depression over a three-month naturalistic treatment with different classes of antidepressants. Changes occurred alongside the decrease of depressive symptoms, with a substantial rate of clinical remission at the endpoint, and anxiety. Similar reductions were observed on the systemic inflammatory index. Post-COVID-19 first-onset and recurrent MDE showed a differential course in the response regarding physical and cognitive features and in a marker of systemic inflammation (i.e., SII).
Patients who developed a recurrent MDE following COVID-19 accounted for about 60% of the sample, were mostly unmarried, and had an earlier age at onset and a longer duration of disease than first-onset MDE, with several affective episodes during their lifetime and higher hospitalization rates.
Major depression can have a relapsing–remitting course, and it has been estimated that a third of non-clinical samples and over three-quarters of subjects in clinical populations will experience at least another depressive episode after the first one, with a mean of almost four episodes per patient [29]. The risk of recurrence has been associated with early disease onset and the number of prior depressive episodes, whereas sociodemographic features tend to have a minor impact [29, 30]. Our results are in line with these data.
Patients with psychiatric disorders, especially depression, have been particularly affected by the COVID-19 pandemic, showing a worsening of pre-existing symptomatology, newly emerging symptoms, and substantial treatment impairment [31, 32]. Also, these patients show a greater vulnerability to the infection and its worse outcomes, which has been recently linked to shared pro-inflammatory responses and cytokine regulation pathways [33]. Indeed, results from a meta-analysis revealed an increased risk of COVID-19 severity and mortality in individuals with a pre-existing diagnosis of mental illness [34].
Here, a more severe COVID-19 was found in subjects with first-onset MDE, who experienced more intense symptoms, higher rates of pharmacotherapies, and hospitalizations in more than 40% of cases. However, this may depend on the lower vaccination rates of this group with more than half being either not vaccinated or having received only one dose of vaccine at the time of the infection.
Can a pre-existing diagnosis of depression affect the clinical picture of post-COVID-19 MDE?
Our results outlined relevant physical symptoms and cognitive impairment as per clinicians’ measures and patients’ self-reports, alongside moderate-to-severe depression and anxiety, without significant differences between post-COVID-19 first-onset and recurrent MDE at baseline.
It is known that major depression can have a heterogeneous presentation with symptoms embracing emotional, physical, and cognitive domains [35], while the most represented COVID-19 sequelae, i.e., fatigue, cognitive dysfunctions, and anxiety, seem to have a specific relation with depressive symptomatology [4, 9, 36, 37]. Self-rated depression was found to be the only significant predictor for the presence and intensity of post-COVID-19 fatigue and cognitive impairment among several demographic, clinical, and psychopathological factors [38, 39].
Results from this study showed that, despite the overall favorable outcome, patients with post-COVID-19 recurrent MDE displayed higher physical symptoms and cognitive impairment throughout the treatment period as revealed by the course of HARS Physical Symptoms, SF-36 PCS, and PDQ-D5 scores, consistently with our hypotheses.
It has been noted that post-COVID-19 depression shows a more severe course of illness in patients with a psychiatric history than in patients at first episode [6]. Aside from SARS-CoV-2 infection, somatic features and cognitive dysfunctions, together with comorbid anxiety [40], have been reported to affect the course of depression and to be associated with more chronicity, lower probability of response, and heightened recurrence risk [24]. Further, evidence from the literature has outlined differences in the clinical profile of first-onset and recurrent depressive episodes with the latter displaying overall increased severity and worse outcomes [41]. Patients diagnosed with recurrent depression have been demonstrated to have greater rates and intensity of depressive symptoms with pervasive pessimistic and suicidal thoughts [42], somatic disturbances, and cognitive dysfunction, with severity increasing alongside the number of episodes [41, 43]. Specifically, pain-related features were most prevalent in recurrent depression [41], and impaired cognitive functioning tends to persist beyond remission of mood symptoms as a consequence of multiple episodes [24, 44].
The role of inflammation
Among substrates of post-COVID-19 MDE, a chronic inflammation triggered by the peripheral immune-inflammatory response to the virus has been hypothesized in addition to the psychological burden experienced during and after the infection [9]. The interrelationship between higher pro-inflammatory markers and depressive symptoms, fatigue, and cognitive deficits has been observed in many COVID-19 survivors [4, 9] and, previously, in subjects with major depressive disorder [45, 46].
Here, a reduction of inflammatory indexes alongside symptoms improvement was observed according to SII levels. Investigating the relationship between psychiatric symptomatology and inflammation was beyond our primary aims; however, it could be presumed that the decrease of low-grade systemic inflammation might have sustained the antidepressant response. These findings seem to further support preliminary evidence about the immune-modulatory effects of SSRIs in post-COVID-19 depression [19, 20] and the anti-inflammatory and antiviral properties of antidepressants that showed to contrast COVID-19 severe outcomes [47]. Such effects could be explained through an indirect downregulation of the cytokine storm and a direct interference with the viral cell invasion exerted by some antidepressants [9, 18, 48, 49].
It should also be noted that, in this sample, post-COVID-19 recurrent MDE showed higher inflammatory levels. This finding is intriguing given that patients with recurrent and first-onset MDE did not differ for medical comorbidities and that subjects at their first episode had experienced a more severe COVID-19.
Although not generalizable to all subjects suffering from mood disorders, in a significant subgroup of patients the increase in inflammatory biomarkers and the subsequent return to almost normal levels might derive from the interrelationship of systems differentially involved in the immune-inflammatory response [15, 16, 50]. The activation of compensatory mechanisms aims to regulate primary responses and can promote remission of the acute phase both spontaneously and after treatment, being further enhanced by antidepressants [50]. However, “trait” biomarkers persist during the remitted phases of the disease suggesting a persistent activation of these pathways and no return to the original homeostasis. Since such systems might also be subject to sensitization, greater numbers of episodes have been associated with a higher increase in inflammatory biomarkers [15].
Within this background, there is evidence reporting that inflammation may correlate not only with specific subgroups of depression but also with a differential treatment response [16]. Recent findings described the association between a broad range of inflammatory markers and a different severity in specific symptom dimensions in depressed patients before starting antidepressants. During the subsequent 26-week treatment, changes in some of these markers showed to correlate with a differential response specifically on neuro-vegetative symptoms (e.g., energy levels, ache, pain) [50]. Nevertheless, whether the decrease of the inflammatory profile during antidepressant treatment can result in differential and symptom-specific response patterns needs to be further explored.
Strengths and limitations
Strengths of this study include sample size, administration of both clinician-rated and self-report questionnaires, thorough characterization of post-COVID-19 depressive episodes, and three-month follow-up. However, some limitations should be noted like the monocentric setting of the study, the lack of neuropsychological tests to assess cognitive performance, and the observational, retrospective design that might have limited the collection of all the variables potentially affecting depressive symptomatology and the inflammatory status, as well as the lack of established mean or cut-off levels of SII, that might have provided references to better stratify the sample according to inflammatory levels and to make further inferences about the association with psychic symptoms.
Conclusions
The presence of additional symptomatology in post-COVID-19 MDE could hinder remission leading to reduced occupational and psychosocial performances with poor quality of life and thus require more symptom-specific approaches to obtain a full functional recovery [9, 50, 51]. Given the well-recognized major severity and the pathophysiological mechanisms of recurrent depression, together with evidence about severe depression persisting in COVID-recovered subjects with a psychiatric history [6], patients with post-COVID-19 recurrent MDE appear to be a population specifically worthy of attention. In particular, we found that in post-COVID-19 recurrent MDE physical and cognitive symptoms showed a blunted response to antidepressant treatment possibly related, at least in part, to sustained higher levels of systemic inflammation. A prompt diagnosis and characterization of depressive episodes in COVID-19 survivors becomes necessary to deliver early interventions [20]. Considering the debated link between inflammatory processes and depression, physical and cognitive symptoms (specifically affected in post-COVID-19 MDE), combined therapies targeting patients’ inflammatory profile may be a promising strategy to improve treatment response [52, 53]. Further studies including similar therapeutic approaches and deepening the knowledge about the pathophysiology of mood disorders [54] and the potential effects of anti-inflammatory compounds are needed [55].
To our knowledge, this is the first study to differentiate between first-onset and recurrent depressive episodes and to evaluate the course of specific correlates of post-COVID-19 depression over months. Multicentric, larger studies with longer follow-ups are needed to identify personalized treatments that will be able to target the specific underlying mechanisms and manage the multidimensional nature of depressive episodes allowing a full functional recovery.
Data availability
Data that support findings of this study are available from the corresponding author, [MDN], upon reasonable request.
References
World Health Organization. World health statistics 2022: monitoring health for the SDGs, sustainable development goals. Geneva. 2022. Licence: CC BY-NC-SA 3.0 IGO.
Comelli A, Viero G, Bettini G, Nobili A, Tettamanti M, Galbussera AA, Muscatello A, Mantero M, Canetta C, Martinelli Boneschi F, Arighi A, Brambilla P, Vecchi M, Lampertico P, Bonfanti P, Contoli M, Blasi F, Gori A, Bandera A (2022) Patient-reported symptoms and sequelae 12 months after COVID-19 in hospitalized adults: a multicenter long-term follow-up study. Front Med 9:834354. https://doi.org/10.3389/fmed.2022.834354
Sani G, Janiri D, Di Nicola M, Janiri L, Ferretti S, Chieffo D (2020) Mental health during and after the COVID-19 emergency in Italy. Psychiatry Clin Neurosci 74(6):372. https://doi.org/10.1111/pcn.13004
Ceban F, Ling S, Lui LMW, Lee Y, Gill H, Teopiz KM, Rodrigues NB, Subramaniapillai M, Di Vincenzo JD, Cao B, Lin K, Mansur RB, Ho RC, Rosenblat JD, Miskowiak KW, Vinberg M, Maletic V, McIntyre RS (2022) Fatigue and cognitive impairment in Post-COVID-19 Syndrome: a systematic review and meta-analysis. Brain Behav Immun 101:93–135. https://doi.org/10.1016/j.bbi.2021.12.020
Premraj L, Kannapadi NV, Briggs J, Seal SM, Battaglini D, Fanning J, Suen J, Robba C, Fraser J, Cho SM (2022) Mid and long-term neurological and neuropsychiatric manifestations of post-COVID-19 syndrome: a meta-analysis. J Neurolo Sci 434:120162. https://doi.org/10.1016/j.jns.2022.120162
Hazumi M, Usuda K, Okazaki E, Kataoka M, Nishi D (2022) Differences in the course of depression and anxiety after COVID-19 infection between recovered patients with and without a psychiatric history: a cross-sectional study. Int J Environ Res Public Health 19(18):11316. https://doi.org/10.3390/ijerph191811316
Teixeira AL, Krause TM, Ghosh L, Shahani L, Machado-Vieira R, Lane SD, Boerwinkle E, Soares JC (2021) Analysis of COVID-19 infection and mortality among patients with psychiatric disorders, 2020. JAMA Network Open 4(11):e2134969. https://doi.org/10.1001/jamanetworkopen.2021.34969
Renaud-Charest O, Lui LMW, Eskander S, Ceban F, Ho R, Di Vincenzo JD, Rosenblat JD, Lee Y, Subramaniapillai M, McIntyre RS (2021) Onset and frequency of depression in post-COVID-19 syndrome: a systematic review. J Psychiatr Res 144:129–137. https://doi.org/10.1016/j.jpsychires.2021.09.054
Mazza MG, Palladini M, Poletti S, Benedetti F (2022) Post-COVID-19 depressive symptoms: epidemiology, pathophysiology, and pharmacological treatment. CNS Drugs 36(7):681–702. https://doi.org/10.1007/s40263-022-00931-3
Mazza MG, Palladini M, De Lorenzo R, Magnaghi C, Poletti S, Furlan R, Ciceri F, COVID-19 BioB Outpatient Clinic Study group, Rovere-Querini P, Benedetti F (2021) Persistent psychopathology and neurocognitive impairment in COVID-19 survivors: effect of inflammatory biomarkers at three-month follow-up. Brain Behav Immun 94:138–147. https://doi.org/10.1016/j.bbi.2021.02.021
Troyer EA, Kohn JN, Hong S (2020) Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain Behav Immun 87:34–39. https://doi.org/10.1016/j.bbi.2020.04.027
Wu Y, Xu X, Chen Z, Duan J, Hashimoto K, Yang L, Liu C, Yang C (2020) Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav Immun 87:18–22. https://doi.org/10.1016/j.bbi.2020.03.031
Wei Y, Feng J, Ma J, Chen D, Chen J (2022) Neutrophil/lymphocyte, platelet/lymphocyte and monocyte/lymphocyte ratios in patients with affective disorders. J Affect Disord 309:221–228. https://doi.org/10.1016/j.jad.2022.04.092
Jeenger J, Singroha V, Sharma M, Mathur DM (2018) C-reactive protein, brain-derived neurotrophic factor, interleukin-2, and stressful life events in drug-naive first-episode and recurrent depression: a cross-sectional study. Indian J Psychiatry 60(3):334–339. https://doi.org/10.4103/psychiatry.IndianJPsychiatry_169_18
Maes M, Carvalho AF (2018) The compensatory immune-regulatory reflex system (CIRS) in depression and bipolar disorder. Mol Neurobiol 55(12):8885–8903. https://doi.org/10.1007/s12035-018-1016-x
Liu CH, Zhang GZ, Li B, Li M, Woelfer M, Walter M, Wang L (2019) Role of inflammation in depression relapse. J Neuroinflammation 16(1):90. https://doi.org/10.1186/s12974-019-1475-7
Dobrodeeva V, Abdyrahmanova A, Astafeva D, Smirnova D, Cumming P, De Sousa A, Davydkin I, Yashikhina A, Shnayder N, Nasyrova R (2022) Pharmacogenetic aspects of COVID-19 management and post-COVID-19 depression treatment with fluvoxamine. Psychiatr Danub 34(Suppl 8):25–30
Xiao X, Wang C, Chang D, Wang Y, Dong X, Jiao T, Zhao Z, Ren L, Dela Cruz CS, Sharma L, Lei X, Wang J (2020) Identification of potent and safe antiviral therapeutic candidates against SARS-CoV-2. Front Immunol 11:586572. https://doi.org/10.3389/fimmu.2020.586572
Di Nicola M, Pepe M, Montanari S, Spera MC, Panaccione I, Simonetti A, Sani G (2023) Vortioxetine improves physical and cognitive symptoms in patients with post-COVID-19 major depressive episodes. Euro Neuropsychopharmacol 70:21–28. https://doi.org/10.1016/j.euroneuro.2023.02.006
Mazza MG, Zanardi R, Palladini M, Rovere-Querini P, Benedetti F (2022) Rapid response to selective serotonin reuptake inhibitors in post-COVID depression. Euro Neuropsychopharmacol 54:1–6. https://doi.org/10.1016/j.euroneuro.2021.09.009
Hamilton M (1960) A rating scale for depression. J Neurol Neurosurg Psychiatry 23(1):56–62
Hamilton M (1959) The assessment of anxiety states by rating. Br J Med Psychol 32(1):50–55
Ware JE Jr, Sherbourne CD (1992) The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 30(6):473–483
Christensen MC, Florea I, Lindsten A, Baldwin DS (2018) Efficacy of vortioxetine on the physical symptoms of major depressive disorder. J Psychopharmacol (Oxford, England) 32(10):1086–1097. https://doi.org/10.1177/0269881118788826
Ware, John & MA, Kosinski & Keller, S.D. (1993). SF-36 Physical and Mental Health Summary Scales: a User's Manual. 8 23–28.
Hewlett S, Dures E, Almeida C (2011) Measures of fatigue: bristol rheumatoid arthritis fatigue multi-dimensional questionnaire (BRAF MDQ), bristol rheumatoid arthritis fatigue numerical rating scales (BRAF NRS) for severity, effect, and coping, Chalder fatigue questionnaire (CFQ), checklist individual strength (CIS20R and CIS8R), fatigue severity scale (FSS), functional assessment chronic illness therapy (Fatigue) (FACIT-F), multi-dimensional assessment of fatigue (MAF), multi-dimensional fatigue inventory (MFI), pediatric quality of life (PedsQL) multi-dimensional fatigue scale, profile of fatigue (ProF), short form 36 vitality subscale (SF-36 VT), and visual analog scales (VAS). Arthritis Care Res 63(Suppl 11):S263–S286. https://doi.org/10.1002/acr.20579
Chen KY, Li T, Gong FH, Zhang JS, Li XK (2020) Predictors of health-related quality of life and influencing factors for COVID-19 patients, a follow-up at one month. Front Psych 11:668. https://doi.org/10.3389/fpsyt.2020.00668
van der Sar B, Talman S, Boonman-de Winter L, de Mol M, Hoefman E, van Etten RW, De Backer IC (2021) Pulmonary function and health-related quality of life after COVID-19 pneumonia. Respir Med 176:106272. https://doi.org/10.1016/j.rmed.2020.106272
Sullivan J, Edgeley K, Dehoux E (1990) A survey of multiple sclerosis. part i: perceived cognitive problems and compensatory strategy used. Can J Rehabilit 4:99–105
Buckman JEJ, Underwood A, Clarke K, Saunders R, Hollon SD, Fearon P, Pilling S (2018) Risk factors for relapse and recurrence of depression in adults and how they operate: a four-phase systematic review and meta-synthesis. Clin Psychol Rev 64:13–38. https://doi.org/10.1016/j.cpr.2018.07.005
Baez LM, Heller AS (2020) Impact of age at onset on the phenomenology of depression in treatment-seeking adults in the STAR*D trial. J Affect Disord 262:381–388. https://doi.org/10.1016/j.jad.2019.10.036
Di Nicola M, Dattoli L, Moccia L, Pepe M, Janiri D, Fiorillo A, Janiri L, Sani G (2020) Serum 25-hydroxyvitamin D levels and psychological distress symptoms in patients with affective disorders during the COVID-19 pandemic. Psychoneuroendocrinology 122:104869. https://doi.org/10.1016/j.psyneuen.2020.104869
Favreau M, Hillert A, Osen B, Gärtner T, Hunatschek S, Riese M, Hewera K, Voderholzer U (2021) Psychological consequences and differential impact of the COVID-19 pandemic in patients with mental disorders. Psychiatry Res 302:114045. https://doi.org/10.1016/j.psychres.2021.114045
Moni MA, Lin PI, Quinn JMW, Eapen V (2021) COVID-19 patient transcriptomic and genomic profiling reveals comorbidity interactions with psychiatric disorders. Transl Psychiatry 11(1):160. https://doi.org/10.1038/s41398-020-01151-3
Toubasi AA, AbuAnzeh RB, Tawileh HBA, Aldebei RH, Alryalat SAS (2021) A meta-analysis: the mortality and severity of COVID-19 among patients with mental disorders. Psychiatry Res 299:113856. https://doi.org/10.1016/j.psychres.2021.113856
Otte C, Gold SM, Penninx BW, Pariante CM, Etkin A, Fava M, Mohr DC, Schatzberg AF (2016) Major depressive disorder. Nat Rev Dis Primers 2:16065. https://doi.org/10.1038/nrdp.2016.65
Malik P, Patel K, Pinto C, Jaiswal R, Tirupathi R, Pillai S, Patel U (2022) Post-acute COVID-19 syndrome (PCS) and health-related quality of life (HRQoL)-a systematic review and meta-analysis. J Med Virol 94(1):253–262. https://doi.org/10.1002/jmv.27309
Yang T, Yan MZ, Li X, Lau EHY (2022) Sequelae of COVID-19 among previously hospitalized patients up to 1 year after discharge: a systematic review and meta-analysis. Infection 50(5):1067–1109. https://doi.org/10.1007/s15010-022-01862-3
Mazza MG, Palladini M, Poletti S, Benedetti F (2021) P.0086 Clinical and psychopathological predictors of fatigue in COVID-19 survivors: a machine learning study. Euro Neuropsychopharmacol 53:S60–S61
Poletti S, Palladini M, Mazza MG, De Lorenzo R, COVID-19 BioB Outpatient Clinic Study group, Furlan R, Ciceri F, Rovere-Querini P, Benedetti F (2022) Long-term consequences of COVID-19 on cognitive functioning up to 6 months after discharge: role of depression and impact on quality of life. Euro Arch Psychiatry Clin Neurosci 272(5):773–782. https://doi.org/10.1007/s00406-021-01346-9
McIntyre RS, Woldeyohannes HO, Soczynska JK, Vinberg M, Cha DS, Lee Y, Gallaugher LA, Dale RS, Alsuwaidan MT, Mansur RB, Muzina DJ, Carvalho A, Kennedy S (2016) The prevalence and clinical characteristics associated with diagnostic and statistical manual version-5-defined anxious distress specifier in adults with major depressive disorder: results from the International mood disorders collaborative project. Ther Adv Chronic Dis 7(3):153–159. https://doi.org/10.1177/2040622315627805
Roca M, Armengol S, García-García M, Rodriguez-Bayón A, Ballesta I, Serrano MJ, Comas A, Gili M (2011) Clinical differences between first and recurrent episodes in depressive patients. Compr Psychiatry 52(1):26–32. https://doi.org/10.1016/j.comppsych.2010.04.011
Ivanets NN, Kinkulkina MA, Tikhonova YG, Izumina TA, Lazareva AV (2020) Klinicheskaya i sotsiodemograficheskaya kharakteristika bol’nykh s pervym depressivnym epizodom i rekurrentnoi depressiei [Clinical and sociodemographic characteristics of patients with the first depressive episode and recurrent depression]. Zhurnal nevrologii i psikhiatrii imeni S.S Korsakova 120(11):33–39. https://doi.org/10.17116/jnevro202012011133
Lin J, Su Y, Shi C, Liu Q, Wang G, Wei J, Zhu G, Chen Q, Tian H, Zhang K, Wang X, Zhang N, Wang Y, Yu X, Si T (2021) Neurocognitive profiles of patients with first-episode and recurrent depression: a cross-sectional comparative study from China. J Affect Disord 286:110–116. https://doi.org/10.1016/j.jad.2021.02.068
Liu Y, Ho RC, Mak A (2012) Interleukin (IL)-6, tumour necrosis factor alpha (TNF-α) and soluble interleukin-2 receptors (sIL-2R) are elevated in patients with major depressive disorder: a meta-analysis and meta-regression. J Affect Disord 139(3):230–239. https://doi.org/10.1016/j.jad.2011.08.003
Mazza MG, Lucchi S, Tringali AGM, Rossetti A, Botti ER, Clerici M (2018) Neutrophil/lymphocyte ratio and platelet/lymphocyte ratio in mood disorders: a meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry 84(Pt A):229–236. https://doi.org/10.1016/j.pnpbp.2018.03.012
Reis G, Dos Santos Moreira-Silva EA, Silva DCM, Thabane L, Milagres AC, Ferreira TS, Dos Santos CVQ, de Souza Campos VH, Nogueira AMR, de Almeida APFG, Callegari ED, de Figueiredo Neto AD, Savassi LCM, Simplicio MIC, Ribeiro LB, Oliveira R, Harari O, Forrest JI, Ruton H, Sprague S, TOGETHER investigators (2022) Effect of early treatment with fluvoxamine on risk of emergency care and hospitalisation among patients with COVID-19: the TOGETHER randomised, platform clinical trial. Lancet Global health 10(1):e42–e51. https://doi.org/10.1016/S2214-109X(21)00448-4
Hoertel N, Sánchez-Rico M, Cougoule C, Gulbins E, Kornhuber J, Carpinteiro A, Becker KA, Reiersen AM, Lenze EJ, Seftel D, Lemogne C, Limosin F (2021) Repurposing antidepressants inhibiting the sphingomyelinase acid/ceramide system against COVID-19: current evidence and potential mechanisms. Mol Psychiatry 26(12):7098–7099. https://doi.org/10.1038/s41380-021-01254-3
Talmon M, Rossi S, Pastore A, Cattaneo CI, Brunelleschi S, Fresu LG (2018) Vortioxetine exerts anti-inflammatory and immunomodulatory effects on human monocytes/macrophages. Br J Pharmacol 175(1):113–124. https://doi.org/10.1111/bph.14074
Kofod J, Elfving B, Nielsen EH, Mors O, Köhler-Forsberg O (2022) Depression and inflammation: correlation between changes in inflammatory markers with antidepressant response and long-term prognosis. Euro Neuropsychopharmacol 54:116–125. https://doi.org/10.1016/j.euroneuro.2021.09.006
Malhi GS, Mann JJ (2018) Depression. Lancet (London, England) 392(10161):2299–2312. https://doi.org/10.1016/S0140-6736(18)31948-2
Fourrier C, Sampson E, Mills NT, Baune BT (2018) Anti-inflammatory treatment of depression: study protocol for a randomised controlled trial of vortioxetine augmented with celecoxib or placebo. Trials 19(1):447. https://doi.org/10.1186/s13063-018-2829-7
Bai S, Guo W, Feng Y, Deng H, Li G, Nie H, Guo G, Yu H, Ma Y, Wang J, Chen S, Jing J, Yang J, Tang Y, Tang Z (2020) Efficacy and safety of anti-inflammatory agents for the treatment of major depressive disorder: a systematic review and meta-analysis of randomised controlled trials. J Neurol Neurosurg Psychiatry 91(1):21–32. https://doi.org/10.1136/jnnp-2019-320912
Richardson B, MacPherson A, Bambico F (2022) Neuroinflammation and neuroprogression in depression: effects of alternative drug treatments. Brain Behav Immun–Health 26:100554. https://doi.org/10.1016/j.bbih.2022.100554
Vasiliu O (2022) Investigational drugs for the treatment of depression (part 1): monoaminergic, orexinergic, GABA-ergic, and anti-inflammatory agents. Front Pharmacol 13:884143. https://doi.org/10.3389/fphar.2022.884143
Funding
No funds, grants, or other external support was received for conducting this study.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to conception and design of the work, acquisition, analysis, and interpretation of data, as well as in drafting the work and revising it critically for important intellectual content. All authors have read and approved the final version of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors confirm that there is no conflict of interest related to the manuscript. MDN is/has been a consultant and/or a speaker and/or has received research grants from: Angelini, Janssen, Lundbeck, Neuraxpharma, and Otsuka. GS is/has been a consultant and/or a speaker and/or has received research grants from: Angelini, Janssen, Lundbeck, Neuraxpharma, and Otsuka.
Ethical approval
The study protocol was conducted in accordance with Good Clinical Practice guidelines and the Declaration of Helsinki (1964) and subsequent revisions and was approved by the Ethics Committee of the Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Università Cattolica del Sacro Cuore, Rome (Italy).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Di Nicola, M., Pepe, M., De Mori, L. et al. Physical and cognitive correlates, inflammatory levels, and treatment response in post-COVID-19 first-onset vs. recurrent depressive episodes. Eur Arch Psychiatry Clin Neurosci 274, 583–593 (2024). https://doi.org/10.1007/s00406-023-01617-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-023-01617-7