Abstract
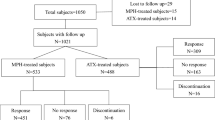
Attention Deficit/Hyperactivity Disorder (ADHD) is the most prevalent neurodevelopmental disorder diagnosed in the scholar age. It is associated with significant impairment in global functioning, and in moderate/severe presentations the outcome is critically dependent on pharmacological optimization of the multi-modal treatment. Methylphenidate (MPH) is the first-choice pharmacological treatment in children and adolescents with ADHD, with substantial evidence of significant efficacy and effectiveness on global functioning and symptoms’ severity. There is some evidence supporting a few clinical and socio-demographic variables as predictors of pharmacological treatment prescription in children with ADHD independently of ADHD symptoms severity. However, it is warranted to investigate clinical and general psychopathological characteristics potentially associated with negative outcomes and the need for pharmacological treatment to inform appropriate prescription strategies. In this context, we compared 268 children and adolescents who were prescribed MPH (ADHD/MPH) for the first time after their first diagnostic assessment at our center, and 444 children and adolescents with ADHD (ADHD/noMPH) who were recommended non-pharmacological evidence-based interventions alone. ADHD/MPH group had higher severity of non-ADHD psychopathological symptoms compared to the ADHD/noMPH group, as documented by higher scores on the Child Behavior Checklist (CBCL) subscales, higher severity of ADHD symptoms, lower average IQ and lower adaptive levels independently of IQ. More specifically, beside externalizing symptoms, also internalizing symptoms were significantly higher in the ADHD/MPH group. The presence of significant non-ADHD psychopathology should be considered as a clinical factor associated with the need for MPH prescription in children and adolescents with ADHD.
Similar content being viewed by others
Availability of data and material
Not applicable.
Code availability
Not applicable.
References
Polanczyk G, de Lima MS, Horta BL et al (2007) The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry 164:942–948
Polanczyk GV, Willcutt EG, Salum GA et al (2014) ADHD prevalence estimates across three decades: An updated systematic review and meta-regression analysis. Int J Epidemiol 43:434–442
Donfrancesco R, Marano A, Calderoni D et al (2015) Prevalence of severe ADHD: an epidemiological study in the Italian regions of Tuscany and Latium. Epidemiol Psychiatr Sci 24:525–533
Arnold LE, Hodgkins P, Caci H et al (2015) Effect of treatment modality on long-term outcomes in attention-deficit/hyperactivity disorder: A systematic review. PLoS ONE 10(2):e0116407
Cortese S, Adamo N, Del Giovane C et al (2018) Comparative efficacy and tolerability of medications for attention-deficit hyperactivity disorder in children, adolescents, and adults: a systematic review and network meta-analysis. Lancet Psychiatry 5(9):727–738
Leucht S, Helfer B, Gartlehner G, Davis JM (2015) How effective are common medications: a perspective based on meta-analyses of major drugs. BMC Med 13:253
Casadei G, Cartabia M, Reale L et al (2017) Italian regional health service costs for diagnosis and 1-year treatment of ADHD in children and adolescents. Int J Ment Health Syst 11:33
Germinario AEP, Arcieri R, Marzi M, et al (2016) ADHD (Attention-Deficit/Hyperactivity Disorder) National Register (Italy): data 2007–2016. 34 p. Rapporti ISTISAN 16/37 (in Italian)
Russell AE, Ford T, Russell G (2019) Barriers and predictors of medication use for childhood ADHD: findings from a UK population-representative cohort. Soc Psychiatry Psychiatr Epidemiol 54:1555–1564
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders (5th ed.) https://doi.org/10.1176/appi.books.9780890425596
Kaufman J, Birmaher B, Brent D et al (1997) Schedule for affective disorders and schizophrenia for school-age children present and lifetime version (K-SADS-PL): Initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 36:980–988
National Institute for Health and Care Excellence (2018) Attention deficit hyperactivity disorder: diagnosis and management. https://www.nice.org.uk/guidance/ng87
Shaffer D, Gould MS, Brasic J et al (1983) A children’s global assessment scale (CGAS). Arch Gen Psychiatry 40:1228–1231
Grizzle R (2011) Wechsler Intelligence Scale for Children, Fourth Edition. In: Goldstein S, Naglieri JA (eds) Encyclopedia of Child Behavior and Development. Springer, US, Boston, MA, pp 1553–1555
Raven J (1981) Manual for Raven’s Progressive Matrices and Vocabulary Scales. Research Supplement No.1: The 1979 British Standardisation of the Standard Progressive Matrices and Mill Hill Vocabulary Scales, Together With Comparative Data From Earlier Studies in the UK, San Antonio, Texas
Oakland T (2011) Adaptive Behavior Assessment System – Second Edition BT - Encyclopedia of Clinical Neuropsychology. In: Kreutzer JS, DeLuca J, Caplan B (eds) Springer. New York, NY, New York, pp 37–39
Sparrow SS (2011) Vineland Adaptive Behavior Scales BT - Encyclopedia of Clinical Neuropsychology. In: Kreutzer JS, DeLuca J, Caplan B (eds) Springer. New York, NY, New York, pp 2618–2621
Conners CK, Sitarenios G, Parker JDA, Epstein JN (1998) the revised conners’ parent rating scale (CPRS-R): factor structure, reliability, and criterion validity. J Abnorm Child Psychol 26:257–268
Volkmar FR (2013) Child Behavior Checklist for Ages 6–18 BT - Encyclopedia of Autism Spectrum Disorders. Springer New York, New York, NY, p 581
Katsuki D, Yamashita H, Yamane K et al (2020) Clinical subtypes in children with attention-deficit hyperactivity disorder according to their child behavior checklist profile. Child Psychiatry Hum Dev 51(6):969–977
Frazier TW, Demaree HA, Youngstrom EA (2004) Meta-analysis of intellectual and neuropsychological test performance in attention-deficit/hyperactivity disorder. Neuropsychology 18(3):543–555
Katusic MZ, Voigt RG, Colligan RC et al (2011) Attention-deficit hyperactivity disorder in children with high intelligence quotient: Results from a population-based study. J Dev Behav Pediatr 32(2):103–109
Mahone EM, Hagelthorn KM, Cutting LE et al (2002) Effects of IQ on executive function measures in children with ADHD. Child Neuropsychol 8(1):52–65
He XX, Qian Y, Wang YF (2013) Practical executive function performance in high intelligence quotient children and adolescents with attention-deficit/hyperactivity disorder. Natl Med J China 93(3):172–176
Daviss WB (2008) A review of co-morbid depression in pediatric ADHD: Etiology, phenomenology, and treatment. J Child Adolesc Psychopharmacol 18(6):565–571
Mannuzza S, Klein RG, Moulton JL 3rd (2008) Lifetime criminality among boys with attention deficit hyperactivity disorder: a prospective follow-up study into adulthood using official arrest records. Psychiatry Res 160:237–246
Shaw M, Hodgkins P, Caci H et al (2012) A systematic review and analysis of long-term outcomes in attention deficit hyperactivity disorder: Effects of treatment and non-treatment. BMC Med 10:99
Frazzetto G, Keenan S, Singh I (2007) ‘I Bambini e le Droghe’: The Right to Ritalin vs the Right to Childhood in Italy. BioSocieties 2(4):393–412
Biederman J, DiSalvo M, Vaudreuil C et al (2020) Can the Child Behavior Checklist (CBCL) help characterize the types of psychopathologic conditions driving child psychiatry referrals? Scand J Child Adolesc Psychiatry Psychol 8:157–165
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
DM performed the statistical analyses. PDR wrote the first draft of the manuscript. IP, SDV and BDA assisted in the literature search and preparation of the manuscript. SV supervised research activities and provided the final revision of the manuscript. All the authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
Not applicable.
Ethics approval
See methods’ section.
Consent to participate
See methods’ section.
Consent for publication
See methods’ section.
Rights and permissions
About this article
Cite this article
De Rossi, P., Pretelli, I., Menghini, D. et al. Clinical characteristics of children and adolescents with ADHD with or without methylphenidate prescription at their first diagnostic assessment. Eur Arch Psychiatry Clin Neurosci 272, 1437–1442 (2022). https://doi.org/10.1007/s00406-022-01386-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-022-01386-9