Abstract
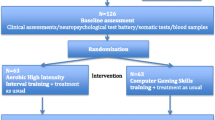
Patients with schizophrenia (SZ) have a high level of cardiovascular morbidity and some clinical symptoms of illness remain resistant to pharmacological approaches. A large number of studies support the effectiveness of physical activity (PA) in SZ. The aims of this trial is to assess the effects of a remote, web-based adapted PA program (e-APA) compared to a health education program (e-HE) on brain plasticity in SZ and healthy volunteers (HV) and on psychiatric, neurocognitive, circadian and physical variables. The study is an interventional, multicenter, randomized open-label trial. Forty-two SZ will be randomized to either the active group (e-APA, N = 21) or nonactive group (e-HE, N = 21), and 21 HV will be matched to SZ according to age, gender, and level of PA in both e-APA and e-HE groups. Interventions will consist of 32 sessions (2 × 60 min/week, for 16 weeks) via supervised home-based videoconferencing. Cerebral magnetic resonance imaging, psychiatric symptoms, neurocognitive and circadian rhythms assessments as well as physical tests and biological analyses will be assessed at baseline and 16 weeks after the intervention. To our knowledge, this is the first study aiming to evaluate the efficacy of APA delivered by supervised home-based videoconferencing in SZ. Moreover, using multimodal MRI, this study could clarify the pathophysiological mechanisms underlying the efficacy of APA. Finally, this innovative approach might also increase participation in long-term PA since PA-based programs are known to have low adherence and early dropout. Trial registration: ClinicalTrials.gov identifier: NCT03261817. Registered on 16 August 2017.

Similar content being viewed by others
References
Tréhout M, Dollfus S (2018) Physical activity in patients with schizophrenia: from neurobiology to clinical benefits. Encephale 44:538–547. https://doi.org/10.1016/j.encep.2018.05.005
Rosenbaum S, Tiedemann A, Sherrington C, Curtis J, Ward PB (2014) Physical activity interventions for people with mental illness: a systematic review and meta-analysis. J Clin Psychiatry 75:964–974. https://doi.org/10.4088/JCP.13r08765
Firth J, Cotter J, Elliott R, French P, Yung AR (2015) A systematic review and meta-analysis of exercise interventions in schizophrenia patients. Psychol Med 45:1343–1361. https://doi.org/10.1017/s0033291714003110
Dauwan M, Begemann MJ, Heringa SM, Sommer IE (2016) Exercise improves clinical symptoms, quality of life, global functioning, and depression in schizophrenia: a systematic review and meta-analysis. Schizophr Bull 42:588–599. https://doi.org/10.1093/schbul/sbv164
Firth J, Stubbs B, Rosenbaum S, Vancampfort D, Malchow B, Schuch F, Elliott R, Nuechterlein KH, Yung AR (2017) Aerobic exercise improves cognitive functioning in people with schizophrenia: a systematic review and meta-analysis. Schizophr Bull 43:546–556. https://doi.org/10.1093/schbul/sbw115
Vogel JS, van der Gaag M, Slofstra C, Knegtering H, Bruins J, Castelein S (2019) The effect of mind-body and aerobic exercise on negative symptoms in schizophrenia: a meta-analysis. Psychiatry Res 279:295–305. https://doi.org/10.1016/j.psychres.2019.03.012
Lalande D, Theriault L, Kalinova E, Fortin A, Leone M (2016) The effect of exercise on sleep quality and psychological, physiological, and biological correlates in patients with schizophrenia: a pilot study. Schizophr Res 171:235–236. https://doi.org/10.1016/j.schres.2016.01.042
Costa R, Bastos T, Probst M, Seabra A, Vilhena E, Corredeira R (2018) Sleep quality in patients with schizophrenia: the relevance of physical activity. Ment Health Phys Act 14:140–145. https://doi.org/10.1016/j.mhpa.2018.04.004
Lederman O, Ward PB, Firth J, Maloney C, Carney R, Vancampfort D, Stubbs B, Kalucy M, Rosenbaum S (2019) Does exercise improve sleep quality in individuals with mental illness? A systematic review and meta-analysis. J Psychiatr Res 109:96–106. https://doi.org/10.1016/j.jpsychires.2018.11.004
Vancampfort D, Rosenbaum S, Ward PB, Stubbs B (2015) Exercise improves cardiorespiratory fitness in people with schizophrenia: a systematic review and meta-analysis. Schizophr Res 169:453–457. https://doi.org/10.1016/j.schres.2015.09.029
Armstrong HF, Bartels MN, Paslavski O, Cain D, Shoval HA, Ballon JS, Khan S, Sloan RP, Kimhy D (2016) The impact of aerobic exercise training on cardiopulmonary functioning in individuals with schizophrenia. Schizophr Res 173:116–117. https://doi.org/10.1016/j.schres.2016.03.009
Chalfoun C, Karelis AD, Stip E, Abdel-Baki A (2016) Running for your life: a review of physical activity and cardiovascular disease risk reduction in individuals with schizophrenia. J Sports Sci 34:1500–1515. https://doi.org/10.1080/02640414.2015.1119875
Hsu CC, Liang CS, Tai YM, Cheng SL (2016) Incongruent changes in heart rate variability and body weight after discontinuing aerobic exercise in patients with schizophrenia. Int J Psychophysiol 109:132–137. https://doi.org/10.1016/j.ijpsycho.2016.08.011
Hjorth P, Davidsen AS, Kilian R, Skrubbeltrang C (2014) A systematic review of controlled interventions to reduce overweight and obesity in people with schizophrenia. Acta Psychiatr Scand 130:279–289. https://doi.org/10.1111/acps.12245
Holt RI (2015) The prevention of diabetes and cardiovascular disease in people with schizophrenia. Acta Psychiatr Scand 132:86–96. https://doi.org/10.1111/acps.12443
Kim DD, Lang DJ, Warburton DE, Barr AM, Smith GN, Thornton AE, White RF, Honer WG, Procyshyn RM (2017) Effects of exercise on serum triglycerides and symptoms of schizophrenia. J Clin Psychopharmacol 37:273–274. https://doi.org/10.1097/jcp.0000000000000648
Schmitt A, Maurus I, Rossner MJ, Röh A, Lembeck M, von Wilmsdorff M, Takahashi S, Rauchmann B, Keeser D, Hasan A, Malchow B, Falkai P (2018) Effects of aerobic exercise on metabolic syndrome, cardiorespiratory fitness, and symptoms in schizophrenia include decreased mortality. Front Psychiatry 9:690. https://doi.org/10.3389/fpsyt.2018.00690
Vancampfort D, Probst M, De Hert M, Soundy A, Stubbs B, Stroobants M, De Herdt A (2014) Neurobiological effects of physical exercise in schizophrenia: a systematic review. Disabil Rehabil 36:1749–1754. https://doi.org/10.3109/09638288.2013.874505
Firth J, Cotter J, Carney R, Yung AR (2017) The pro-cognitive mechanisms of physical exercise in people with schizophrenia. Br J Pharmacol 174:3161–3172. https://doi.org/10.1111/bph.13772
Maurus I, Hasan A, Röh A, Takahashi S, Rauchmann B, Keeser D, Malchow B, Schmitt A, Falkai P (2019) Neurobiological effects of aerobic exercise, with a focus on patients with schizophrenia. Eur Arch Psychiatry Clin Neurosci 269:499–515. https://doi.org/10.1007/s00406-019-01025-w
Farnia V, Farshchian F, Farshchian N, Alikhani M, Sadeghi Bahmani D, Brand S (2020) Comparisons of voxel-based morphometric brain volumes of individuals with methamphetamine-induced psychotic disorder and schizophrenia spectrum disorder and healthy controls. Neuropsychobiology 79:170–178. https://doi.org/10.1159/000504576
Tamminga CA, Stan AD, Wagner AD (2010) The hippocampal formation in schizophrenia. Am J Psychiatry 167:1178–1193. https://doi.org/10.1176/appi.ajp.2010.09081187
Adriano F, Caltagirone C, Spalletta G (2012) Hippocampal volume reduction in first-episode and chronic schizophrenia: a review and meta-analysis. Neuroscientist 18:180–200. https://doi.org/10.1177/1073858410395147
Pajonk FG, Wobrock T, Gruber O et al (2010) Hippocampal plasticity in response to exercise in schizophrenia. Arch Gen Psychiatry 67:133–143. https://doi.org/10.1001/archgenpsychiatry.2009.193
Malchow B, Keeser D, Keller K et al (2016) Effects of endurance training on brain structures in chronic schizophrenia patients and healthy controls. Schizophr Res 173:182–191. https://doi.org/10.1016/j.schres.2015.01.005
Scheewe TW, van Haren NE, Sarkisyan G, Schnack HG, Brouwer RM, de Glint M, Hulshoff Pol HE, Backx FJ, Kahn RS, Cahn W (2013) Exercise therapy, cardiorespiratory fitness and their effect on brain volumes: a randomised controlled trial in patients with schizophrenia and healthy controls. Eur Neuropsychopharmacol 23:675–685. https://doi.org/10.1016/j.euroneuro.2012.08.008
Firth J, Stubbs B, Vancampfort D, Schuch F, Lagopoulos J, Rosenbaum S, Ward PB (2018) Effect of aerobic exercise on hippocampal volume in humans: a systematic review and meta-analysis. Neuroimage 166:230–238. https://doi.org/10.1016/j.neuroimage.2017.11.007
Haukvik UK, Tamnes CK, Söderman E, Agartz I (2018) Neuroimaging hippocampal subfields in schizophrenia and bipolar disorder: a systematic review and meta-analysis. J Psychiatr Res 104:217–226. https://doi.org/10.1016/j.jpsychires.2018.08.012
Baglivo V, Cao B, Mwangi B et al (2018) Hippocampal subfield volumes in patients with first-episode psychosis. Schizophr Bull 44:552–559. https://doi.org/10.1093/schbul/sbx108
Vargas T, Dean DJ, Osborne KJ, Gupta T, Ristanovic I, Ozturk S, Turner J, van Erp TGM, Mittal VA (2018) Hippocampal subregions across the psychosis spectrum. Schizophr Bull 44:1091–1099. https://doi.org/10.1093/schbul/sbx160
Papiol S, Popovic D, Keeser D, Hasan A, Schneider-Axmann T, Degenhardt F, Rossner MJ, Bickeböller H, Schmitt A, Falkai P, Malchow B (2017) Polygenic risk has an impact on the structural plasticity of hippocampal subfields during aerobic exercise combined with cognitive remediation in multi-episode schizophrenia. Transl Psychiatry 7:e1159. https://doi.org/10.1038/tp.2017.131
Chung AK, Chua SE (2011) Effects on prolongation of Bazett's corrected QT interval of seven second-generation antipsychotics in the treatment of schizophrenia: a meta-analysis. J Psychopharmacol 25:646–666. https://doi.org/10.1177/0269881110376685
Howell S, Yarovova E, Khwanda A, Rosen SD (2019) Cardiovascular effects of psychotic illnesses and antipsychotic therapy. Heart 105:1852–1859. https://doi.org/10.1136/heartjnl-2017-312107
Franklin BA, Thompson PD, Al-Zaiti SS, Albert CM, Hivert MF, Levine BD, Lobelo F, Madan K, Sharrief AZ, Eijsvogels TMH (2020) Exercise-related acute cardiovascular events and potential deleterious adaptations following long-term exercise training: placing the risks into perspective-an update: a scientific statement from the american heart association. Circulation. https://doi.org/10.1161/cir.0000000000000749
Herbsleb M, Schumann A, Malchow B, Puta C, Schulze PC, Gabriel HW, Bär KJ (2018) Chronotropic incompetence of the heart is associated with exercise intolerance in patients with schizophrenia. Schizophr Res 197:162–169. https://doi.org/10.1016/j.schres.2018.02.020
Herbsleb M, Keller-Varady K, Wobrock T, Hasan A, Schmitt A, Falkai P, Gabriel HHW, Bär KJ, Malchow B (2019) The influence of continuous exercising on chronotropic incompetence in multi-episode schizophrenia. Front Psychiatry 10:90. https://doi.org/10.3389/fpsyt.2019.00090
Warburton DE, Charlesworth SA, Foulds HJ, McKenzie DC, Shephard RJ, Bredin SS (2013) Qualified exercise professionals: best practice for work with clinical populations. Can Fam Physician 59:759–761
Gudrun DT, Christoph D, Bernd D, Harald VS (1990) Adapted physical activity: an interdisciplinary approach. Springer-Verlag, Berlin
Stubbs B, Firth J, Berry A, Schuch FB, Rosenbaum S, Gaughran F, Veronesse N, Williams J, Craig T, Yung AR, Vancampfort D (2016) How much physical activity do people with schizophrenia engage in? A systematic review, comparative meta-analysis and meta-regression. Schizophr Res 176:431–440. https://doi.org/10.1016/j.schres.2016.05.017
Stubbs B, Koyanagi A, Schuch F, Firth J, Rosenbaum S, Gaughran F, Mugisha J, Vancampfort D (2017) Physical activity levels and psychosis: a mediation analysis of factors influencing physical activity target achievement among 204 186 people across 46 low- and middle-income countries. Schizophr Bull 43:536–545. https://doi.org/10.1093/schbul/sbw111
Vancampfort D, De Hert M, Skjerven LH, Gyllensten AL, Parker A, Mulders N, Nyboe L, Spencer F, Probst M (2012) International organization of physical therapy in mental health consensus on physical activity within multidisciplinary rehabilitation programmes for minimising cardio-metabolic risk in patients with schizophrenia. Disabil Rehabil 34:1–12. https://doi.org/10.3109/09638288.2011.587090
Vancampfort D, Rosenbaum S, Schuch FB, Ward PB, Probst M, Stubbs B (2016) Prevalence and predictors of treatment dropout from physical activity interventions in schizophrenia: a meta-analysis. Gen Hosp Psychiatry 39:15–23. https://doi.org/10.1016/j.genhosppsych.2015.11.008
Firth J, Rosenbaum S, Stubbs B, Gorczynski P, Yung AR, Vancampfort D (2016) Motivating factors and barriers towards exercise in severe mental illness: a systematic review and meta-analysis. Psychol Med 46:2869–2881. https://doi.org/10.1017/s0033291716001732
Yung AR, Firth J (2017) How should physical exercise be used in schizophrenia treatment? Expert Rev Neurother 17:213–214. https://doi.org/10.1080/14737175.2017.1275571
Kolt GS, Rosenkranz RR, Vandelanotte C, Caperchione CM, Maeder AJ, Tague R, Savage TN, Van IA, Mummery WK, Oldmeadow C, Duncan MJ (2017) Using Web 2.0 applications to promote health-related physical activity: findings from the WALK 2.0 randomised controlled trial. Br J Sports Med 51:1433–1440. https://doi.org/10.1136/bjsports-2016-096890
McIntosh JRD, Jay S, Hadden N, Whittaker PJ (2017) Do E-health interventions improve physical activity in young people: a systematic review. Public Health 148:140–148. https://doi.org/10.1016/j.puhe.2017.04.001
Degroote L, Plaete J, De Bourdeaudhuij I, Verloigne M, Van Stappen V, De Meester A, Poppe L, Van der Mispel C, Crombez G (2018) The effect of the eHealth intervention 'MyPlan 1.0' on physical activity in adults who visit general practice: a quasi-experimental trial. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph15020228
Alvarez-Jimenez M, Alcazar-Corcoles MA, González-Blanch C, Bendall S, McGorry PD, Gleeson JF (2014) Online, social media and mobile technologies for psychosis treatment: a systematic review on novel user-led interventions. Schizophr Res 156:96–106. https://doi.org/10.1016/j.schres.2014.03.021
Naslund JA, Marsch LA, McHugo GJ, Bartels SJ (2015) Emerging mHealth and eHealth interventions for serious mental illness: a review of the literature. J Ment Health 24:321–332. https://doi.org/10.3109/09638237.2015.1019054
Rotondi AJ, Eack SM, Hanusa BH, Spring MB, Haas GL (2015) Critical design elements of e-health applications for users with severe mental illness: singular focus, simple architecture, prominent contents, explicit navigation, and inclusive hyperlinks. Schizophr Bull 41:440–448. https://doi.org/10.1093/schbul/sbt194
Brunette MF, Rotondi AJ, Ben-Zeev D, Gottlieb JD, Mueser KT, Robinson DG, Achtyes ED, Gingerich S, Marcy P, Schooler NR, Meyer-Kalos P, Kane JM (2016) Coordinated technology-delivered treatment to prevent rehospitalization in schizophrenia: a novel model of care. Psychiatr Serv 67:444–447. https://doi.org/10.1176/appi.ps.201500257
Gaebel W, Großimlinghaus I, Kerst A, Cohen Y, Hinsche-Böckenholt A, Johnson B, Mucic D, Petrea I, Rössler W, Thornicroft G, Zielasek J (2016) European Psychiatric Association (EPA) guidance on the quality of eMental health interventions in the treatment of psychotic disorders. Eur Arch Psychiatry Clin Neurosci 266:125–137. https://doi.org/10.1007/s00406-016-0677-6
Treisman GJ, Jayaram G, Margolis RL, Pearlson GD, Schmidt CW, Mihelish GL, Kennedy A, Howson A, Rasulnia M, Misiuta IE (2016) Perspectives on the use of ehealth in the management of patients with schizophrenia. J Nerv Ment Dis 204:620–629. https://doi.org/10.1097/nmd.0000000000000471
Rotondi AJ, Sinkule J, Haas GL, Spring MB, Litschge CM, Newhill CE, Ganguli R, Anderson CM (2007) Designing websites for persons with cognitive deficits: design and usability of a psychoeducational intervention for persons with severe mental illness. Psychol Serv 4:202–224. https://doi.org/10.1037/1541-1559.4.3.202
Kasckow J, Felmet K, Appelt C, Thompson R, Rotondi A, Haas G (2014) Telepsychiatry in the assessment and treatment of schizophrenia. Clin Schizophr Relat Psychoses 8:21–27a. https://doi.org/10.3371/csrp.kafe.021513
Ricci J, Gagnon L (2011) Evaluation du niveau d’activité physique et de condition physique. Clinic Prosport. https://www.ffsa.asso.fr/Pages/InCadres/GestClient/Communication/SportSante/Rassemblement/Evaluation_outils/test-ricci-gagnon_actif-inactif.pdf
Garber CE, Blissmer B, Deschenes MR, Franklin BA, Lamonte MJ, Lee IM, Nieman DC, Swain DP (2011) American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc 43:1334–1359. https://doi.org/10.1249/MSS.0b013e318213fefb
Bull FC, Maslin TS, Armstrong T (2009) Global Physical Activity Questionnaire (GPAQ): nine country reliability and validity study. J Phys Act Health 6:790–804. https://doi.org/10.1123/jpah.6.6.790
Borg G (1998) Borg's perceived exertion and pain scales. Borg's perceived exertion and pain scales. Human Kinetics, Champaign
Yushkevich PA, Pluta JB, Wang H, Xie L, Ding SL, Gertje EC, Mancuso L, Kliot D, Das SR, Wolk DA (2015) Automated volumetry and regional thickness analysis of hippocampal subfields and medial temporal cortical structures in mild cognitive impairment. Hum Brain Mapp 36:258–287. https://doi.org/10.1002/hbm.22627
Wechsler D (1981) WAIS-R manual: Wechsler adult intelligence scale-revised. The Psychological Corporation, New York
Wechsler D (2001) MEM-III, Échelle clinique de mémoire de Wechsler: manuel. Les Éd. du Centre de psychologie appliquée, cop., Paris
Rey A (1964) L’examen clinique en psychologie. Presses Universitaires de France, Paris
Stroop JR (1935) Studies of interference in serial verbal reactions. J Exp Psychol 18:643–662. https://doi.org/10.1037/h0054651
Reitan RM (1958) Validity of the trail making test as an indicator of organic brain damage. Percept Mot Ski 8:271–276. https://doi.org/10.2466/pms.1958.8.3.271
Brickenkamp R, Zillmer E (1998) D2—test of attention. Hogrefe & Huber, Göttingen
Cardebat D, Doyon B, Puel M, Goulet P, Joanette Y (1990) Formal and semantic lexical evocation in normal subjects. Performance and dynamics of production as a function of sex, age and educational level. Acta Neurol Belg 90:207–217
Kay SR, Fiszbein A, Opler LA (1987) The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophr Bull 13:261–276. https://doi.org/10.1093/schbul/13.2.261
Dollfus S, Mach C, Morello R (2016) Self-evaluation of negative symptoms: a novel tool to assess negative symptoms. Schizophr Bull 42:571–578. https://doi.org/10.1093/schbul/sbv161
Kirkpatrick B, Strauss GP, Nguyen L, Fischer BA, Daniel DG, Cienfuegos A, Marder SR (2011) The brief negative symptom scale: psychometric properties. Schizophr Bull 37:300–305. https://doi.org/10.1093/schbul/sbq059
Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta Psychiatr Scand 67:361–370. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x
Guy W (1976) ECDEU assessment manual for psychopharmacology, revised. US department of health, education, and welfare publication (ADM). National Institute of Mental Health, Rockville
Birchwood M, Smith J, Drury V, Healy J, Macmillan F, Slade M (1994) A self-report insight scale for psychosis: reliability, validity and sensitivity to change. Acta Psychiatr Scand 89:62–67. https://doi.org/10.1111/j.1600-0447.1994.tb01487.x
Waintraud L, Guelfi JD, Lancrenon S, Rouillon F (1995) Validation of M. Weissman's social adaptation questionnaire in its French version. Ann Med Psychol 153:274–277
Ryff CD, Keyes CL (1995) The structure of psychological well-being revisited. J Pers Soc Psychol 69:719–727. https://doi.org/10.1037//0022-3514.69.4.719
Saunders JB, Aasland OG, Babor TF, De La Fuente JR, Grant M (1993) Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction 88:791–804. https://doi.org/10.1111/j.1360-0443.1993.tb02093.x
Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO (1991) The fagerström test for nicotine dependence: a revision of the fagerström tolerance questionnaire. Br J Addict 86:1119–1127. https://doi.org/10.1111/j.1360-0443.1991.tb01879.x
Legleye S, Karila L, Beck F, Reynaud M (2007) Validation of the CAST, a general population Cannabis Abuse Screening Test. J Subst Use 12:233–242. https://doi.org/10.1080/14659890701476532
Denise P, Benoît O (2016) Actisomm. Logiciel d’analyse des données actimétriques
Cosgrave J, Wulff K, Gehrman P (2018) Sleep, circadian rhythms, and schizophrenia: where we are and where we need to go. Curr Opin Psychiatry 31:176–182. https://doi.org/10.1097/yco.0000000000000419
Johansson AS, Owe-Larsson B, Hetta J, Lundkvist GB (2016) Altered circadian clock gene expression in patients with schizophrenia. Schizophr Res 174:17–23. https://doi.org/10.1016/j.schres.2016.04.029
Youngstedt SD (2005) Effects of exercise on sleep. Clin Sports Med 24(355–365):xi. https://doi.org/10.1016/j.csm.2004.12.003
Chennaoui M, Arnal PJ, Sauvet F, Léger D (2015) Sleep and exercise: a reciprocal issue? Sleep Med Rev 20:59–72. https://doi.org/10.1016/j.smrv.2014.06.008
Kimhy D, Lauriola V, Bartels MN, Armstrong HF, Vakhrusheva J, Ballon JS, Sloan RP (2016) Aerobic exercise for cognitive deficits in schizophrenia—the impact of frequency, duration, and fidelity with target training intensity. Schizophr Res 172:213–215. https://doi.org/10.1016/j.schres.2016.01.055
Faul F, Erdfelder E, Lang AG, Buchner A (2007) G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 39:175–191. https://doi.org/10.3758/bf03193146
Wasserstein RL, Schirm AL, Lazar NA (2019) Moving to a World beyond “p %3c 0.05”. Am Stat 73:1–19. https://doi.org/10.1080/00031305.2019.1583913
Zhu W (2012) Sadly, the earth is still round (P %3c 0.05). J Sport Health Sci 1:9–11. https://doi.org/10.1016/j.jshs.2012.02.002
Zhu W (2016) p %3c 0.05, %3c 0.01, %3c 0.001, %3c 0.0001, %3c 0.00001, %3c 0.000001, or %3c 0.0000001. J Sport Health Sci 5:77–79. https://doi.org/10.1016/j.jshs.2016.01.019
Tumiel E, Wichniak A, Jarema M, Lew-Starowicz M (2019) Nonpharmacological interventions for the treatment of cardiometabolic risk factors in people with schizophrenia—a systematic review. Front Psychiatry 10:566–566. https://doi.org/10.3389/fpsyt.2019.00566
Marcus BH, Ciccolo JT, Sciamanna CN (2009) Using electronic/computer interventions to promote physical activity. Br J Sports Med 43:102–105. https://doi.org/10.1136/bjsm.2008.053744
Andersson G (2016) Internet-delivered psychological treatments. Annu Rev Clin Psychol 12:157–179. https://doi.org/10.1146/annurev-clinpsy-021815-093006
Sharma A, Sharma SD, Sharma M (2017) Mental health promotion: a narrative review of emerging trends. Curr Opin Psychiatry 30:339–345. https://doi.org/10.1097/yco.0000000000000347
van der Stouwe ECD, van Busschbach JT, de Vries B, Cahn W, Aleman A, Pijnenborg GHM (2018) Neural correlates of exercise training in individuals with schizophrenia and in healthy individuals: a systematic review. Neuroimage Clin 19:287–301. https://doi.org/10.1016/j.nicl.2018.04.018
Acknowledgements
We thank the DRCI (Délégation à la Recherche Clinique et à l’Innovation) and CRC (Centre de Recherche Clinique) staffs for their contribution to the study conception and for the promotion and management of the protocol proceedings. We also thank Pr Olivier Guillin from the University Hospital of Rouen and all associated investigators for their clinical contributions. We thank collaborators from GIP Cyceron, Nicolas Delcroix for MRI sequences, Frédéric Briend for MRI spectroscopy sequence and assessments, Mickael Naveau for the database, and Gaëlle Chetelat and Robin de Flores for hippocampal sequence. We thank Drs Perrine Brazo, Sophie Meunier-Cussac, Aurélie Montagne, Pierrick Lebain, Anaïs Vandevelde, for patient recruitment. Finally, we thank patients and healthy volunteers for their upcoming participation in the study.
Funding
The PEPSY European project is co-funded by the Normandy County Council, European Union in the framework of the ERDF-ESF operational program 2014–2020. This work was also supported by the Fondation Pierre Deniker. Funding sources were not involved in the study design, the collection, analysis and interpretation of data, the writing of the report, or the decision to submit the paper for publication.
Author information
Authors and Affiliations
Contributions
MT: participation in HE program conception and dispensation, subject recruitment, participant assessments, MRI assessments, data analysis, and manuscript drafting and revision. EL: HE program conception and dispensation, subject recruitment, MRI assessments, imaging pre- and postprocessing, data analysis, neurocognitive assessments, and manuscript revision. SJ: HE program conception and dispensation and neurocognitive assessments. PL: methods on the evaluation of APA. LB: APA video conferencing and SAPATIC platform management, participation in HE and APA program conception, and manuscript revision. AH: study conception and design, APA program conception, and SAPATIC platform conception and management. ER: exercise test dispensation. RM: methodological conception and manuscript revision. PAC: e-Celcius and Zephyr BioHarness® management. GQ: study conception and design, circadian data analysis, and manuscript revision. SD: study conception and design, principal investigator, patient recruitment, participant assessments, MRI assessments, data analysis, and manuscript revision. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
MT participated in educational conferences for the following industrial laboratories: Otsuka, Lundbeck, and Janssen. SD has been an expert and consultant or participated in educational conferences for the following industrial laboratories or companies: Gedeon Richter, Lundbeck Otsuka, Roche, Takeda, Fabre, Janssen, ONO Pharma and Verasci. She also has a license agreement on SNS with MedAvante-ProPhase. EL, SJ, PL, ER, RM and GQ have no competing conflicts. AH is the manager of the V@Si company, and LB is employed by V@Si. PA is employed by Bodycap Company.
Ethical approval
The protocol was submitted to the French Health Authority, namely, the Agence Nationale de Sécurité du Médicament et des produits de santé (ANSM), for formal approval to conduct the study conduct and to ensure that the study meets the local regulations of a properly constituted Ethics Committee. The project was approved by Health Authorities (ANSM) on 19 July 2016 (ID-RCB number 2016-A00930-51) and by the local ethical committee (Comité de Protection des Personnes, CPP Nord-Ouest IV, France) on 10 January 2017 in compliance with French regulations. The trial was registered at ClinicalTrial.gov on 25 August 2017 (NCT03261817). Initial information about the study is given to eligible participants by the regular staff during a routine appointment or by coworkers. Further detailed written and oral information about the trial are then provided by the project coworker. Voluntary participation is assured, and participants can withdraw at any time and receive standard treatment regardless of whether they choose to participate. Each participant provides written informed consent before any intervention is started.
Trial status
The current PEPSYV@SI protocol version is 5 dated 6 March 2018. The first participant was recruited in September 2017, and the study is currently enrolling participants. The study is expected to be completed in December 2021.
Additional information
Communicated by Peter Falkai.
Rights and permissions
About this article
Cite this article
Tréhout, M., Leroux, E., Bigot, L. et al. A web-based adapted physical activity program (e-APA) versus health education program (e-HE) in patients with schizophrenia and healthy volunteers: study protocol for a randomized controlled trial (PEPSY V@Si). Eur Arch Psychiatry Clin Neurosci 271, 325–337 (2021). https://doi.org/10.1007/s00406-020-01140-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-020-01140-z