Abstract
Purpose
Revision stapes surgery is a challenging procedure performed in relatively small numbers compared to other middle ear procedures. Despite numerous data on hearing results of different middle ear surgeries, the audiological standards for successful outcome of this procedure are still not clarified. On the basis of well-documented data, we wanted to determine what the expected audiological results and complications are after revision stapes surgery in order to set a realistic threshold for surgical success.
Methods
After the protocol registration in the PROSPERO database, a systematic review was performed in multiple databases (PubMed, Cochrane, Web of Science, Scopus, ScienceOpen, ClinicalTrials.gov, Google Scholar) according to PRISMA guidelines. Twelve articles were reviewed according to the inclusion criteria. A total of 1032 cases were obtained for evaluation. A modified version of Newcastle–Ottawa Scale (NOS) was used to assess publication quality.
Results
Average air–bone gap (ABG) gain was 17.3 dB, average air conduction (AC) gain was 17.5 dB. The average postoperative air–bone gap was 11.1 dB. The postoperative ABG distribution was the following 0–10 dB: 53.3%, > 10–20 dB: 28.2%, > 20 dB: 18.5%. SNHL as a surgical complication was described in a total of 17 cases (1.6%), no equilibrium disorder was reported.
Conclusion
The pooled data suggest that revision stapes surgery is an effective solution after failure of previous stapes surgery. However, the results are clearly inferior to those of primary stapedotomies. Hence, we need to apply different expectations and use different standards in the indication and evaluation of this type of surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The history of modern stapes surgery began in 1956 when Shea [1] performed the first stapedectomy with proper reconstruction of the ossicular chain. Since then, stapes surgery has made great progress and by the beginning of the twenty-first century, in Shea’s words, it “became so successful, the problem has now largely disappeared” [2]. Today, it is truly a flawless procedure at first glance, with high success rates, but in 3–13% of the cases [3], the results after primary surgery are not sufficient and these are the cases where problems are “reappearing”. The results of revision surgery appear to be inferior to primary surgery [4], for several reasons, some of them may be due to previous surgery. The impact of the previous procedure on the success of the revision varies. The most common and hardly reversible problem appears to be the formation of intratympanic adhesion [5, 6], which makes surgery challenging, while other issues such as prosthesis dislocations could be resolved with better results. The diversity of these problems leads to different outcomes. While expectations for primary stapes surgery are quite clear and the standards for success are well established, these standards are lacking in revision cases. According to the literature, a postoperative ABG of 10 dB or less is considered as success in stapes surgery [7,8,9]. In revision cases, the situations the surgeons have to deal with are different, and expectations before surgery are not as straightforward as in primary stapedotomy. The question is what level of hearing outcomes can be expected after revision stapes surgeries. The results of revision stapes surgery have been the subject of several publications, but individually the number of cases and the quality of data are limited. Our goal was to collect well-documented data from these previous publications to provide information to better understand the outcomes of revision stapedotomy. This information will lead to more realistic expectations, which is necessary for making appropriate counselling and indications, and it is useful in defining the standards of surgical success.
Materials and methods
The Preferred Reporting Items for Systematic Reviews and Meta-analysis.
(PRISMA) guidelines were used to report the results.
Eligibility criteria: The PICO search strategy protocol was used, and the protocol for this study was registered at PROSPERO (ID: CRD42022242662). Patients (P) aged at least 16 years, with a diagnosis of stapes fixation (clinically, or surgically diagnosed), and who had undergone previous stapes surgery without the presence of osteogenesis imperfecta, congenital middle ear or inner ear deformity were involved. Only revision stapes surgeries (I) were involved in the investigation. Publications with inadequate surgical methodology were excluded. Due to the original question (C), the comparison was not applicable. The examined outcome (O) was postoperative average audiometry results measured at least 12 months after surgical intervention and postoperative morbidity. Only measurements according to the AAO HNS reporting guidelines with a follow-up of at least 12 months were included. Meta-analyses, systematic reviews, randomized controlled Trials, research studies or articles, case reports or series were all included in the search. Research reports or other grey literature and clinical practice guidelines were excluded.
Search and selection: A systematic literature search was performed in multiple databases: PubMed, Cochrane, Web of Science, Scopus, ScienceOpen, ClinicalTrials.gov, Google Scholar dating from January 1st 1991 to January 1st 2021, using the following search strategy: ("revision") AND ("stapes" OR "stapedotomy" OR "stapedectomy" OR "otosclerosis") Only English literature was included. The result studies were imported to EndNote X9.1 citation manager software (Thomson Reuters). Study selection was performed by two authors L.Á. and SZ.L. under the supervision of the senior author P.G..
Data extraction and outcome measurement: Data extraction was performed by two independent reviewers under the supervision of the senior author. Data were transferred to an Excel sheet, author, year of publication, study design, demographics, number of interventions, follow-up time, and specific outcome: pre- and postoperative PTA levels, complications, type of prosthesis, and surgical approach. Audiological results such as AC, ABG, BC Hearing Gain, ABG Gain, and averages were expressed in dBs. The mean of the thresholds at frequencies 0.5, 1, 2, and 3 or 4 kHz was used to form a four-tone pure-tone average. The pooled data were narratively reviewed and compared to former literature data on stapes surgery outcomes.
Risk of bias (ROB) assessment: Assessment was performed by the three authors in the same setting. The Modified Newcastle‐Ottawa Scale (NOS) was used in all cases, as all the involved manuscripts were nRCTs.
Results
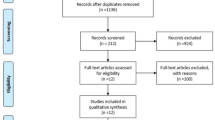
Study selection: The search and selection process is shown in the PRISMA flow diagram (Fig. 1). After the first search, 1230 papers were found. After duplications were removed, 507 manuscripts were screened by title, abstract and full text. Fifteen publications met the eligibility criteria, of which three [10,11,12] were removed due to insufficient data after full-text screening. Twelve studies were included in the final review process[13,14,15,16,17,18,19,20,21,22,23,24], which represents 1032 cases. Article characteristics are shown in Table 1. Risk of bias assessment according to the modified version of NOS can be found in Supplement 1.
Patients and procedure: According to the pooled data, the average age was 47.8 years, ranging from 16 to 88 years. The female to male ratio was 61–39%.
Hearing results: Pre- and postoperative AC levels were available in 484 cases. Mean preoperative AC level was 61.1 dB, mean postoperative AC was 43.6 dB, which means an average of 17.5 dB hearing gain after the procedure. Pre- and postoperative ABG levels were available in 571 and 712 cases, respectively. The average preoperative ABG was 28.4 dB, postoperative ABG was 11.1 dB, this represents an average ABG gain of 17.3 dB (Table 2). Postoperative ABG distribution in 10 dB bins was available in 875 cases. ABG closure of 10 dB or less was achieved in 53.3% of the cases, whereas in 28.2%, ABG was between 10 and 20 dB, and in 18.5% of the cases, postoperative ABG remained 20 dB or higher (Fig. 2).
Surgical technique and findings
Numerical data about stapes prosthetics was available in 10 publications. The type of the revised prosthesis was available in 278 cases. Retrieved prosthesis showed a wide range of variation with a relatively high number of wire type prosthetics, and autologous reconstructions (Table 3). Data about newly inserted prosthetics was available in 678 cases. In the majority of the cases (59%) classic piston type prosthetics was used, autologous and wire type solutions were used in minimal numbers. Malleovestibulopexy was performed in 23% of the cases and in 4 of the 140 cases malleus relocation with malleovestibulopexy was performed using reshaped necrosed incus [16].
Regarding the surgical findings, we found relevant data in 846 cases. In the publications sometimes multiple concomitant causes were reported for the same operation. The most common problem reported was necrosis of the long process of incus in 41%, followed by prosthesis dislocation in 36% and periprosthetic scarring in 23%. Tympanic membrane pathologic findings were not mentioned numerically (Table 4).
Separate audiological data in relevant numbers could be found related to two specific situations: cases where malleovestibulopexy was performed and cases where cause of failure was incus necrosis. In case of malleovestibulopexy the data of 129 cases were processed and ABG closure of 10 dB or less, 11–20 dB, and > 20DB was found in 36, 46 and 18% respectively (Table 5a). Concerning incus necrosis according to data of 251 cases ABG closure was 60, 30, and 10% respectively (Table 5b).
Complications: Severe complications were observed in 17 cases (1.6%). All of them were severe SNHL that occurred after surgery, 2 cases had profound hearing loss. Transient taste disturbance (most likely related to injury of the chorda tympani) and transient tinnitus were mentioned. Numerical data for these latter two complications were not available. These mentioned complications completely resolved within 3–6 weeks after surgery. Permanent vertigo was reported in 2 cases. In one additional case, vertigo and disequilibrium occurred one year after the revision, however, in this case further investigation did not prove direct connection with the revision surgery.
Discussion
Interpretation of the results
The results of our review suggest that revision stapes surgery is a viable option in cases of failure or relapse after primary surgery. We also found a relevant ABG closure and hearing gain rates, whereas complication rate was about 1.6%. At first glance, the ABG gain of 17.3 dB can be compared with primary stapedotomy results, where the average ABG closure and hearing gain is about 20 dB, with most reports in the range of 18–24 dB [3, 7, 25, 26], still a negative difference of nearly 15%. Complication rates after primary surgery ranged between 0.5 and 2% [3, 27, 28] but were mainly reported below 1%, although the complication rate at revisions was 1.6%. Thus, the probability of developing a permanent adverse situation is about two-fold. The vast majority of these cases are severe SNHL, vestibular symptoms appear to be rare, dysgeusia was not documented in detail in the involved publications. ABG levels are always reported in papers on stapes surgery; however, definitive AC levels and hearing gains are often missing, even in otherwise high-quality papers. Due to the above-mentioned phenomenon, reporting exclusively ABG results after revision surgery can be misleading. In terms of the distribution of the results, looking at the literature we can see comparable outcomes. One of the most cited publications in the topic is Robert Vincent’s Prospective Study of 652 Cases [29], which couldn’t be involved because of our inclusion criteria (inferior age limit was 16 years). In this publication the minimum one year follow up was achieved in 278 cases. The postoperative 10 dB distribution is the following: 10 dB or less 65%, 11–20 dB 9%, > 20 dB 26%. The results at one year follow up (n = 197) was: 10 dB or less 67.5%, 11–20 dB 15.5%, > 20 dB 17%. According to the 875 cases reviewed ABG closure of 10 dB or less was achieved in 53.3%, 10–20 dB 28.2%, > 20 dB 18.5%. The results of Vincent are somewhat above the average of the data analysed in the review.
Comparing this result with primary stapes surgery we could see the following: surgical success (ABG 10 dB or less) was achieved in 53.3% of the revision cases vs. 70 and 94% of primary surgery outcomes [3, 7, 26, 30, 31]. The ABG range of 20 dB or less was achieved in 81.5% of the cases. The same 0–20 dB ABG interval is seen in 92–98% [3, 7, 31] of primary surgeries. In 18.5% of the cases, the ABG remained above 20 dB, which can be considered as an unsuccessful intervention. On the basis of all this information, it is clear that the results and expectations for revision surgeries are not the same as for primary procedures. It has been shown that hearing improvement can be achieved in general, but outcomes are usually more modest compared to primary stapes surgeries. In terms of the distribution of results, the variability of outcomes appears to be greater when revisions are performed. When revisions are compared to primary surgeries, the probability of moderate results (ABG between 10 and 20 dB) is quite similar. The main difference between the upper and the bottom section of results is seen with a range far worse below 10 dB to above 20 dB ratio, which is around 0.35 for revision cases vs. around 0.03–0.1 for primary surgeries [3, 7] in the literature. This means that the postoperative audiological results of ineffective revision surgeries not only fall into the mid-range, but often right into the unsuccessful range. This variability is due to various intratympanic scenarios, influenced by the original pathology, previous surgery, and post-surgical reactions.
According to analysed data, no numerical analysis could be performed regarding the type of retrieved prosthesis and hearing outcome. However, it looks like the former use of older “wire type” prosthesis leads more frequently to incus necrosis [18, 20]. Looking at the prosthetics inserted during revision, classic piston type and other modern prosthetics (e.g. soft clip, shape-memory pistons) are dominating, while autologous and “wire types” are hardly in use anymore. In case of severe incus necrosis, incus luxation or ankylosis malleovestibulopexy is a therapeutical option, which was performed in 23% of the operations. This intervention led to < 20 dB ABG closure in 82%, which is very close to the results of revision surgeries in general. Other results from the literature suggest incudovestibulopexies are superior to malleovestibulopexies from audiological standpoint [21, 33]. Still, the latter is definitely a viable and recommended solution in case of damaged incus for ossicular chain reconstruction.
Certain situations, such as intratympanic scarring, appear to be negative predictors of surgical success [6, 10], whereas prosthesis related problems might be easier to manage [8, 32]. According to the data, in cases of incus necrosis alone without any fibrosis ABG could be closed below 10 dB in 60% and below 20 dB in 90% of the cases. These numbers are nearly 10 percent better than results in revision surgery in general. Thus, incudovestibulopexy should be preferred vs. malleovestibulopexy if it can be performed reasonably.
The technique of the previous surgery also seems to be determinant. Partial and total removal of the stapes footplate has a detrimental effect on outcomes according to literature. It has been reported in certain cases that the long-term AC gain after revision stapedectomy can be as low as 7 dB [8, 32, 34]. All the above-mentioned aspects should be taken into consideration when discussing possible postoperative expectations. Therefore, preoperative workup with HRCT imaging is strongly recommended, even if the evaluation is often challenging [35, 36], and it is not always possible to assess the exact problem underlying the inadequate hearing results.
In none of the included publications was the issue of advanced otosclerosis addressed. According to the review of Adrien A. Eshraghi and his team on this topic [37], stapedotomy alone, promises good results in cases with speech recognition scores higher than 50%, and minor retrofenestral involvement, in contrary cases with major retrofenestral involvement and a speech recognition score less than 30% are proven to have unsatisfactory results. In these latter cases a combination with traditional hearing aids may provide a sufficient solution with measurable hearing improvement and patient contentment. In cases where stapedotomy alone or in combination with traditional hearing aid still do not result in sufficient audiological results, cochlear implantation should be considered, however, electrode insertion may be challenging due to sclerosis and spongiosis. As an alternative in certain cases active middle ear implants may provide an efficient solution in conductive or mixed hearing losses [38, 39]. As in primary surgeries, conventional hearing aids alone could be possible alternatives of revision operations as well.
Concerning the indication of the surgery we have take all these aspects into consideration. Mostly the indications for revision is relative and are based on the possibility of hearing improvement. In general, it is realistic to set 20 dB ABG gain and 17.5 dB AC gain as achievable goal and the indication should be made accordingly. In certain situations, the expectable outcomes are better, like in cases of incus necrosis without malleovestibulopexy. That is why the use of CT scanning could help to predict the most likely outcomes.
Conclusion
Our review consolidate that different audiological outcomes may be expected after revisions with different causes of failure.
Audiological data suggest that AC gain and ABG gain results were similar after revision stapes surgeries. However, it seems that there is a greater chance of sensorineural threshold shift with repeated interventions, so it would be also useful to assess not only ABG results but also AC results. While ABG is an important indicator in conductive hearing loss, the quality of life is ultimately determined by the AC threshold. This is why we recommend that AC levels and gains should always be reported after revision surgery. Generally speaking, the results are worse compared to primary surgery. A maximum of 10 dB ABG is widely accepted as success after primary stapes surgery. However, as we saw earlier, it is unrealistic to have the same expectations for revisions. While the 10 dB threshold can only be achieved in 53.3%, the range below 20 dB can be achieved in 81.5%. The latter percentage is similar to the success rates (≤ 10 dB) of primary surgery (70–94%). In our opinion, it is realistic to consider the range below 20 dB as a success range after revision stapes surgery. However, if we are talking about individual cases, it is important to assess the preoperative hearing status to set our goals. The mean 17.5 dB AC gain could be another cornerstone of expectations, and achieving this range of AC gain may also be an indicator of surgical success.
Data availability
Not applicable.
Abbreviations
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- NOS:
-
Newcastle–Ottawa Scale
- SNHL:
-
Sensorineural hearing loss
- ABG:
-
Air bone ap
- AC:
-
Air conduction
- BC:
-
Bone conduction
- PTA:
-
Pure tone audiometry
- RCT:
-
Randomised controlled trial
References
Shea JJ Jr (1958) Fenestration of the oval window. Ann Otol Rhinol Laryngol 67(4):932–951
Shea JJ Jr (1998) A personal history of stapedectomy. Am J Otol 19(5 Suppl):S2-12
Vincent R, Sperling NM, Oates J, Jindal M (2006) Surgical findings and long-term hearing results in 3050 stapedotomies for primary otosclerosis: a prospective study with the otology-neurotology database. Otol Neurotol 27(8 Suppl 2):S25-47
Magliulo G, Cristofari P, Terranova G (1997) Functional hearing results in revision stapes surgery. Am J Otol 18(4):408–412
Kanona H, Bhutta MF, Lavy J (2017) Our approach to revision stapes surgery and the outcomes from 49 procedures at a UK tertiary centre. Clin Otolaryngol 42(4):931–935
Polony G, Gáborján A, Tamás L, Székely L (2022) Revision stapedotomies: the role of periprosthetic scar tissue formation in the development of unsatisfactory hearing results after stapedotomy. Int Arch Otorhinolaryngol. https://doi.org/10.1055/s-0041-1740100
Strömbäck K, Lundman L, Bjorsne A, Grendin J, Stjernquist-Desatnik A, Dahlin-Redfors Y (2017) Stapes surgery in Sweden: evaluation of a national-based register. Eur Arch Otorhinolaryngol 274(6):2421–2427
Wegner I, Vincent R, Derks LSM, Rauh SP, Heymans MW, Stegeman I, Grolman W (2018) An internally validated prognostic model for success in revision stapes surgery for otosclerosis. Laryngoscope 128(10):2390–2396
Committee on Hearing and Equilibrium guidelines for the evaluation of results of treatment of conductive hearing loss. AmericanAcademy of Otolaryngology-Head and Neck Surgery Ffoundation, Inc. (1995) Otolaryngol Head Neck Surg. 113(3): 186–187
Hammerschlag PE, Fishman A, Scheer AA (1998) A review of 308 cases of revision stapedectomy. Laryngoscope 108(12):1794–1800
Sarac S, McKenna MJ, Mikulec AA, Rauch SD, Nadol JB Jr, Merchant SN (2006) Results after revision stapedectomy with malleus grip prosthesis. Ann Otol Rhinol Laryngol 115(4):317–322
Van Rompaey V, Claes G, Somers T, Offeciers E (2011) Erosion of the long process of the incus in revision stapes surgery: malleovestibular prosthesis or incus reconstruction with hydroxyapatite bone cement? Otol Neurotol 32(6):914–918
Babighian GG, Albu S (2009) Failures in stapedotomy for otosclerosis. Otolaryngol Head Neck Surg 141(3):395–400
Bernardeschi D, Canu G, De Seta D, Russo FY, Ferrary E, Mosnier I, Sterkers O (2018) Revision stapes surgery: a review of 102 cases. Clin Otolaryngol 43(6):1587–1590
Fisch U, Acar GO, Huber AM (2001) Malleostapedotomy in revision surgery for otosclerosis. Otol Neurotol 22(6):776–785
Ghonim M, Shabana Y, Ashraf B, Salem M (2017) Revision stapedectomy with necrosis of the long process of the incus: does the degree of necrosis matter? A retrospective clinical study. J Int Adv Otol 13(1):28–31
Han WW, Incesulu A, McKenna MJ, Rauch SD, Nadol JB Jr, Glynn RJ (1997) Revision stapedectomy: intraoperative findings, results, and review of the literature. Laryngoscope 107(9):1185–1192
Krieger LW, Lippy WH, Schuring AG, Rizer FM (1998) Revision stapedectomy for incus erosion: long-term hearing. Otolaryngol Head Neck Surg 119(4):370–373
Lippy WH, Wingate J, Burkey JM, Rizer FM, Schuring AG (2002) Stapedectomy revision in elderly patients. Laryngoscope 112(6):1100–1103
Ozüer MZ, Olgun L, Gültekin G (2012) Revision stapes surgery. Otolaryngol Head Neck Surg 146(1):109–113
Puxeddu R, Ledda GP, Pelagatti CL, Salis G, Agus G, Puxeddu P (2005) Revision stapes surgery for recurrent transmissional hearing loss after stapedectomy and stapedotomy for otosclerosis. Acta Otorhinolaryngol Ital 25(6):347–352
Schmid P, Häusler R (2009) Revision stapedectomy: an analysis of 201 operations. Otol Neurotol 30(8):1092–1100
Skrivan J, Cada Z, Kluh J, Boucek J, Profant O, Betka J (2014) Revision operations after previous stapes surgery for persisting hearing loss. Bratisl Lek Listy 115(7):442–444
Vartiainen E, Nuutinen J, Virtaniemi J (1992) Long-term results of revision stapes surgery. J Laryngol Otol 106(11):971–973
Bartel R, Huguet G, Cruellas F, Hamdan M, Gonzalez-Compta X, Cisa E (2021) Laser vs drill for footplate fenestration during stapedotomy: a systematic review and meta-analysis of hearing results. Eur Arch Otorhinolaryngol 278(1):9–14
Szekely L, Gaborjan A, Danos K, Szaloki T, Fent Z, Tamas L, Polony G (2020) Mid-term evaluation of perioperative i.v. corticosteroid treatment efficacy on overall and audiological outcome following CO2 laser stapedotomy: a retrospective study of 84 cases. Eur Arch Otorhinolaryngol 277(4):1031–1038
Mann WJ, Amedee RG, Fuerst G, Tabb HG (1996) Hearing loss as a complication of stapes surgery. Otolaryngol Head Neck Surg 115(4):324–328
Wegner I, Kamalski DMA, Tange RA, Vincent R, Stegeman I, van der Heijden GJM, Grolman W (2014) Laser versus conventional fenestration in stapedotomy for otosclerosis: a systematic review. Laryngoscope 124(7):1687–1693
Vincent R, Rovers M, Zingade N, Oates J, Sperling N, Deveze A, Grolman W (2010) Revision stapedotomy: operative findings and hearing results—a prospective study of 652 cases from the otology-neurotology database. Otol Neurotol 31(6):875–82
Wegner I, Swartz JE, Bance ML, Grolman W (2016) A systematic review of the effect of different crimping techniques in stapes surgery for otosclerosis. Laryngoscope 126(5):1207–1217
Dhooge I, Desmedt S, Maly T, Loose D, Van Hoecke H (2018) Long-term hearing results of stapedotomy: analysis of factors affecting outcome. Eur Arch Otorhinolaryngol 275(5):1111–1119
Lesinski SG (2002) Causes of conductive hearing loss after stapedectomy or stapedotomy: a prospective study of 279 consecutive surgical revisions. Otol Neurotol 23(3):281–288
De La Cruz A, Fayad JN (2000) Revision stapedectomy. Otolaryngol Head Neck Surg 123(6):728–732
Somers T, Govaerts P, de Varebeke SJ, Offeciers E (1997) Revision stapes surgery. J Laryngol Otol 111(3):233–239
Whetstone J, Nguyen A, Nguyen-Huynh A, Hamilton BE (2014) Surgical and clinical confirmation of temporal bone CT findings in patients with otosclerosis with failed stapes surgery. AJNR Am J Neuroradiol 35(6):1195–1201
Naggara O, Williams T, Ayache D, Heran F, Piekarski JD (2005) Imaging of postoperative failures and complications in stapes surgery for otosclerosis. J Radiol 86(12 Pt 1):1749–1761
Eshraghi AA, Ila K, Ocak E, Telischi FF (2018) Advanced otosclerosis: stapes surgery or cochlear implantation? Otolaryngol Clin North Am 51(2):429–440
Baumgartner WD, Boheim K, Hagen R, Muller J, Lenarz T, Reiss S, Schlogel M, Mlynski R, Mojallal H, Colletti V, Opie J (2010) The vibrant soundbridge for conductive and mixed hearing losses: European multicenter study results. Adv Otorhinolaryngol 69:38–50
Venail F, Lavieille JP, Meller R, Deveze A, Tardivet L, Magnan J (2007) New perspectives for middle ear implants: first results in otosclerosis with mixed hearing loss. Laryngoscope 117(3):552–555
Funding
Open access funding provided by Semmelweis University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. We have no conflicts of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Székely, L., Uri, I., Luka, Á. et al. Audiological outcomes after revision stapes surgeries: a systematic review. Eur Arch Otorhinolaryngol (2024). https://doi.org/10.1007/s00405-024-08741-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00405-024-08741-7