Abstract
Purpose
Study the efficacy of olfactory training in smell recovery.
Methods
An extensive search was performed through different databases in order to find articles analyzing the efficacy of olfactory training as a treatment for olfactory dysfunction. Methodological quality of primary studies within the final sample was assessed following PRISMA guidelines. Standardized mean differences in pre–post olfactory training groups, and also in experimental-control and pre-follow up if possible, were computed by Hedges’ g effect size statistic. Each effect size was weighted by its inverse variance.
Results
Final sample was composed of 36 articles (45 pre–post effect sizes). Contrasts were performed separately for odor identification, odor discrimination, odor threshold and general olfactory function. Moderate to large and heterogeneous effect was obtained for olfactory function (g = 0.755, k = 45, SE = 0.093, CI 95% = [0.572, 0.937]), different moderators had a significant effects, such as, training duration, age and anosmia diagnosis.
Conclusion
Olfactory training was found to have a positive and significant effect on rehabilitating the olfactory function.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Olfactory dysfunctions (OD) are a problem to which less attention is usually paid because it is considered to have a less serious clinical impact, because olfactory dysfunctions are rarely fatal, patients often do not receive adequate medical care. An impaired sense of smell can have a negative effect on quality of life and safety, and can be a sign of other health problems [1,2,3].
Recent investigations have shown that OD occurs at a much higher rate than previously assumed. The frequency of a decreased olfactory performance was estimated as high as 16%, with approximately 5% of the general population being functionally anosmic [4]. In adults aged 50 years and above, the prevalence of impaired olfaction was found to be 25%, implicating that aging is an important factor associated with olfactory loss [5, 6]. In addition, sinonasal disease, upper respiratory tract infections, and trauma are among the most frequent causes of dysosmia [7].
In patients with OD, an impact is usually observed on activities of daily living, personal hygiene, safety and sexual behavior [8, 9]. It has been suggested that the malnutrition associated with age is due OD alone or associated with taste alteration derived by retronasal olfactory alterations [10].
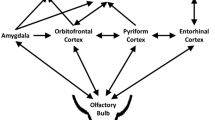
Currently, there is no generally approved way to treat olfactory impairment, however, the neural plasticity quality of the olfactory system offers possibilities regarding treatment. Regenerative capacities of the olfactory pathway include mechanisms ranging from changes in membrane excitability to changes in synaptic efficacy to neurogenesis and apoptosis [11]. More importantly, it has been shown that exposure to an odor may modulate this regenerative capacity [12, 13]. As odors can influence this regenerative capacity, olfactory training (OT) has been a basis of research conducted in various smell and taste studies [14].
In the absence of effective pharmacological treatment [15,16,17,18]. OT has emerged as a first tool for the treatment of olfactory loss. The concept of training is analogous to physical therapy following a cerebrovascular accident, a stroke or other neurological condition. In the face of an event that generates a deficit, existing neurological pathways can be strengthened and trained to compensate [19]. Olfactory training is based on retraining the brain to correctly interpret the neurological signals received when odorants are presented and generate an impulse that travels through the olfactory nerve, the olfactory bulb and the olfactory cortex. Olfactory training involves the deliberate and repeated exposure of a set of odorants over a period of time. Studies have demonstrated its efficacy in post-infection patients on rehabilitating olfactory function [20, 21].
Two modalities of olfactory training have been described: classic olfactory training where patients are exposed to the same 4 odorants (rose, eucalyptus, lemon, and clove) during the rehabilitation process, and personalized or modified olfactory training, adapted to the patient’s results in the tests measuring quantity and quality of olfactory loss or based on different concentrations [22], and other olfactory training modalities were also included such as, aromatherapy [23] or essential mineral oils [24], where patients are exposed to different groups of odorants that are modified periodically throughout the intervention, and must be smelled for at least 5 min, 2 times a day and for at least 6 weeks [25,26,27].
Nonetheless, given that there are open discussions about the effectiveness of OT and that not under all circumstances the training proved to lead to significant smell improvement (e.g. in elderly) [28, 29].
In view of the open discussions about olfactory training effectiveness, this study was conducted with the view to summarize, update and obtain reliable and precise estimates of overall training benefit on the olfactory function, and to analyze the heterogeneity between the available studies to date before its wide application in clinical practice.
Methods and materials
Search strategy
An extensive literature search and review was carried out to identify studies that conducted an olfactory evaluation before and after olfactory training. Articles whose publication period was between 2010 and March, 2022 were taken into account.
Initially, articles were searched in English, Spanish and Portuguese. Electronic database retrieval included ProQuest, Pubmed, Scopus, Web of science using the following keywords: “olfactory”, “smell”, “smelling”, “odor”, “sniffin”, “olfaction”, “anosmia”, “olfactory dysfunction”, “olfactory function”, “olfactory performance” combined with “treatment”, “stimulation”, “trial”, “therapy”, “intervention”, “olfactory treatment”, “training” and “rehabilitation”. Keywords were adapted for each database. Moreover, references of all studies were also examined for possible additional publications. Later on, another search was yielded using Google Academic in order to retrieve possible additional studies that may have been left over on the initial search.
Review strategy
According to the research topic and summary, two researchers independently (AHDL and MLDL) identified possible valid studies based on title and abstract. Following, a pair of raters selected abstracts for full review based on inclusion/exclusion criteria. Two of the authors (AHDL and JB), using a standardized form, extracted data, narrative synthesis and vote counting methods were used to summarize and interpret study data. Any disagreement was resolved by consulting a third party investigator (MLDL). The current study was reported in accordance with the latest PRISMA guidelines [30].
Quality assessment
Qualitative assessment of the risk of bias for each primary study included within the final sample was performed. The Risk Of Bias In Non-randomized Studies of Interventions (ROBINS-I) [31] tool was chosen in order to accomplish this quality assessment. The ROBINS-I is an instrument from the Cochrane Collaboration whose main function is to assess non-randomized studies of interventions. Overall risk-of-bias is judged under six potential sources of bias: confounding bias risk, Selection bias risk, bias risk due to classification of interventions, bias risk due to deviation from intended intervention, measurement bias risk and reporting bias risk. Within each domain or source of potential bias, assessments are made for one or more items, which may cover different aspects of the domain, or different outcomes.
Potential risk-of-bias for each source/domain may range from Low to Moderate to Serious to Critical [or NI (not informed), if that would be the case]. Two researchers (AHDL and JB) performed the assessment and discussed all differences in order to establish an agreement for each study’s risk-of-bias.
Eligibility criteria
The primary outcome of this study is olfactory training. All papers selected for final consideration met the following criteria: (i) participants signed informed study consent; (ii) participants were submitted to an olfactory evaluation test previous to training; (iii) participants were submitted to a otorhinolaryngology exploration previous to training; (iv) the treatment provided was non-pharmacological olfactory training or a combination of both; (v) participants were provided an olfactory training kit or the means to stimulate olfactory function; (vi) training consisted of a minimum of 6 weeks; (vii) participants were evaluated after finalizing the training period; (viii) results of olfactory training were reported.
Coding procedures
Two of the authors (AHDL and JB) independently coded each article for relevant information including sample selection, sample size, main statistics necessary to the computation of effect size, and information necessary for the moderator analyses.
Statistical methods
The complete set of analyses was performed with the metafor package [32] of R software, version 3.5.2 [33]. All analyses were performed with significance level set at α = 0.05.
Firstly, effect sizes were calculated as Hedges’ g (standardized mean differences, SMD). Three different effect sizes were computed for each study: pre–post (SMD between pre and post olfactory scores in training groups), experimental-control (SMD between post scores of training and control groups) and pre-follow up (SMD between pre and follow-up olfactory scores in training groups). For some studies, mean and standard deviations were not available, so F tests or t-statistics were used to calculate effect size. Differences between study sample sizes were controlled by weighting each study according to its inverse variance estimate. This procedure was formulated by Hedges [34].
Once Hedges’ g and variance estimates were computed for each primary study, random-effect models were estimated in order to obtain meta-analytic effect sizes. Meta-analytic effect size was calculated for olfactory identification, olfactory discrimination, olfactory threshold and olfactory function (TDI) in pre–post, experimental-control and pre-follow up categories. Furthermore, Cochran’s Q tests were performed for each model to study effect size homogeneity across primary studies. In addition, publication bias was addressed by four different approaches. Firstly, evidence of publication bias was searched through visual inspection of funnel plots. Then, Egger’s regression test [35] was performed in order to assess potential asymmetry of those funnel plots. Finally, Duval and Tweedie’s trim and fill [36] method was applied, alongside with the computation of fail-safe N number (number of null studies which are required to be introduced into the meta-analysis to cancel the observed effect) by Rosenthal [37] method.
Moderators
As statistically significant heterogeneity within meta-analytic models is expected, key moderators of interest were coded for each study. Moderator analysis comprised the following variables: (i) olfactory diagnosis (categorical; hyposmia, anosmia or others (diagnosis was obtain in each study included, when it was not provided in the study, it was obtained by the TDI 10th cut-off point to discriminate between hyposmia and anosmia, as established in the original study by Hummel and colleagues [38]), (ii) etiology of olfactory loss (categorical; otorhinolaryngological issues, respiratory infection, head trauma, laryngeal tumor, idiopathic alterations, persistent COVID-19 or healthy individuals), (iii) type of treatment (categorical; only olfactory training, olfactory training combined with prescribed medication or others), (iv) olfactory training type (categorical; classic training, personalized training or other), (v) age (numeric, mean age of participants), and (vi) training duration in weeks (numeric).
In addition, in experimental vs control analysis, olfactory diagnosis of control groups (categorical; hyposmia, anosmia, others or healthy individuals) was also included as moderator. In pre vs follow-up analysis, weeks between pre and follow-up assessments were included.
Results
Search results
Overall, 7451 articles were found in the initial search. The relation between databases and articles is as follows: Scopus (3299 titles), ProQuest (2761 titles), Pubmed (1206 titles) and Web of Science (185 titles). Additionally, a thorough manual review of articles was performed using cross-references from identified original articles and reviews (2 titles). Before any other action, 5700 duplicates were removed. The remaining 1751 references were screened, first, by title (1516 excluded) and then by abstract (189 excluded). Finally, 46 references were intended to be retrieved and 36 studies were eventually included in the final sample (45 pre–post comparisons). Search results are summarized in PRISMA Flow Diagram (Fig. 1).
A brief summary of these 36 studies is exposed in Table 1. Each study is characterized with Author, Year and Nationality. Methodological variables are the olfactory assessment instrument, olfactory scores obtained with this instrument, presence of a control group and a brief description of the olfactory intervention carried out. Results of quality assessment with Cochrane’s ROBINS-I tool are exposed in Table 2.
Pre vs post meta-analysis results
Olfactory function
Overall analysis of olfactory training on olfactory function shows pre–post meta-analytical effect of g = 0.755 (k = 45, SE = 0.093, CI 95% = [0.572, 0.937]). As heterogeneity within study effect sizes is statistically different from 0 (I2 = 86.64%, Q(44) = 286.545, p < 0.0001), moderator analysis was performed.
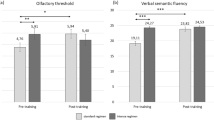
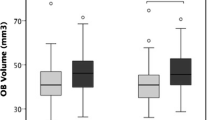
Moderator analysis of potential predictors shows a statistically significant positive effect of duration of training period (k = 45, b = 0.027, Z = 2.145, p = 0.032) and age (k = 45, b = 0.025, Z = − 2.812, p = 0.005). Hence, longer training periods statistically predicts higher effect sizes and olfactory training effect tends to be higher in younger participants. No other moderator was able to account for model variability (p > 0.05). Regarding the model, heterogeneity accounted is R2 = 0.332 (Fig. 2).
Olfactory identification
Analysis of olfactory training efficacy on olfactory identification performance shows pre–post meta-analytical effect of g = 0.843 (k = 35, SE = 0.139, CI 95% = [0.571, 1.114]). Heterogeneity percentage is similar to olfactory function, having I2 = 90.92% (Q(34) = 322.143, p < 0.0001). In this case, moderator analysis also points to duration of training (k = 24, b = 0.063, Z = 2.206, p = 0.027) and anosmia diagnosis (k = 24, b = 1.86, Z = 3.139, p = 0.0017) as predictors whose effects are positive and statistically significant. Therefore, regarding olfactory identification, longer training periods are related to higher effect sizes and, pre–post effect sizes tend to be higher in anosmic training groups. No other moderator was able to account for model variability (p > 0.05). Model with moderators accounts a R2 = 0.395 (Fig. 3).
Olfactory discrimination
Pre–post meta-analytical effect of olfactory training on olfactory discrimination function is g = 0.585 (k = 32, SE = 0.119, CI 95% = [0.351, 0.818]). Heterogeneity within study effect sizes is also significant (I2 = 86.26%, Q(31) = 206.526, p < 0.0001). Therefore, moderator analysis of potential predictors was performed. In this case, other training (not classic nor personalized) statistically predicts lower effect sizes compared to only personalized training (k = 23, b = − 1.411, Z = − 2.586, p = 0.009). Besides, training tends to show higher effect sizes in olfactory discrimination in patients whose etiology is respiratory infections compared to other otorhinolaryngological issues (k = 23, b = 0.906, Z = 2.028, p = 0.042). No other predictor is statistically significant within the model (p > 0.05). Model with moderator’s accounts for R2 = 0.393 (Fig. 4).
Olfactory threshold
Pre–post effect sizes on olfactory threshold function resulted in a meta-analytic effect of g = 0.406 (k = 35, SE = 0.104, CI 95% = [0.202, 0.61]). As heterogeneity within study effect sizes is statistically different from 0 (I2 = 84.67%, Q(35) = 207.067, p < 0.0001), moderator analysis was performed, but no predictor was able to account for model variability (p > 0.05; Fig. 5).
Experimental vs control meta-analysis results
Olfactory function
For the results of this section, meta-analysis was performed on experimental vs control effect sizes. Overall analysis of olfactory training on olfactory function shows experimental vs control meta-analytical effect of g = 2.124 (k = 8, SE = 0.363, CI 95% = [1.412, 2.836]). In this case, heterogeneity within study effect sizes is statistically different from 0 (I2 = 86.31%, Q(7) = 42.497, p < 0.0001). Therefore, moderator analysis was performed. Mean age shows a potential positive effect (k = 8, b = 0.036, Z = 2.393, p = 0.016). This effect could imply a tendency of olfactory training increasing its effect with age. However, this effect might be a statistical artifact, with only 8 primary results. By categorizing mean age moderator in [18–40), [40–60) and [60, > 60], we found just 2 studies with mean age below 40 years. Effect size in this group [18–40) is significantly lower within moderator analysis (b = − 1.96, Z = − 2.135, p = 0.033). Hence, this result may be explained by this statistical artifact. No other statistically significant effect was in any potential moderator variable (p > 0.05).
Olfactory identification
Analysis of olfactory training effectiveness on olfactory identification performance shows experimental vs control meta-analytical effect of g = 1.486 (k = 10, SE = 0.335, CI 95% = [0.829, 2.143]). Heterogeneity percentage is I2 = 89.37% (Q(9) = 87.248, p < 0.0001), so moderator analysis was performed. In this case, mean age (k = 9, b = 0.036, Z = 2.393, p = 0.016), duration of training period (k = 9, b = 0.053, Z = 2.565, p = 0.0103) and diagnosis of anosmia (k = 9, b = 0.894, Z = 2.056, p = 0.039) are suitable and statistically significant predictors of effect sizes. Hence, training effect size tends to be higher in older cohorts, also in samples with diagnosis of anosmia and with longer training periods.
Olfactory discrimination
Experimental vs control effect sizes on olfactory discrimination performance resulted in a meta-analytic effect of g = 1.088 (k = 9, SE = 0.219, CI 95% = [0.66, 1.517]). As heterogeneity within study effect sizes is statistically different from 0 (I2 = 74.99%, Q(35) = 31.502, p < 0.0001), moderator analysis was performed. However, no statistically significant predictor was found within the model (p > 0.05).
Olfactory threshold
Meta-analysis of olfactory training effectiveness on olfactory threshold function points that there is no evidence to support an experimental vs control meta-analytical effect different from 0 (g = 0.087, k = 9, SE = 0.097, CI 95% = [− 0.103, 0.278]). No further analyses were performed in this case (Fig. 6).
Pre vs follow-up meta-analysis results
Olfactory function
Finally, pre and follow up effect sizes were meta-analyzed. Overall analysis of olfactory training on olfactory function shows pre and follow up meta-analytical effects of g = 1.751 (k = 9, SE = 0.712, CI 95% = [0.352, 3.149]). Heterogeneity within study effect sizes is also statistically different from 0 (I2 = 98.02%, Q(8) = 211.262, p < 0.0001); so moderator analysis was performed. Anosmia diagnosis was found as a statistically significant predictor within the model (k = 6, b = 4.229, Z = 3.13, p = 0.0017), accounting for a R2 = 0.834.
Olfactory identification
Pre and follow up effect sizes on olfactory threshold function resulted in a meta-analytic effect of g = 1.355 (k = 10, SE = 0.421, CI 95% = [0.529, 2.18]). As heterogeneity within study effect sizes is statistically different from 0 (I2 = 94.63%, Q(9) = 137.627, p < 0.0001), moderator analysis was performed. Nevertheless, no predictor was found statistically different from 0 within the model (p > 0.05).
Olfactory discrimination
Analysis of olfactory training effectiveness on olfactory threshold function shows experimental vs control meta-analytical effect of g = 1.498 (k = 8, SE = 0.54, CI 95% = [0.442, 2.554]). Heterogeneity percentage is similar to olfactory function, having I2 = 95.41% (Q(7) = 129.536, p < 0.0001). However, moderator analysis points to no variable as a statistically significant predictor within the model (p > 0.05).
Olfactory threshold
Finally, pre and follow up effect sizes on olfactory threshold function resulted in a meta-analytic effect of g = 0.295 (k = 8, SE = 0.102, CI 95% = [0.084, 0.504]). Analysis of heterogeneity within study effect sizes gives an I2 = 15.99%, which gives no evidence of being statistically different from 0 (Q(7) = 7.767, p = 0.353). Therefore, no moderator analysis was performed (Fig. 7).
Publication bias
Analyses of publication bias were performed over pre and post meta-analysis models (TDI, Olfactory Identification, Olfactory Discrimination and Olfactory Threshold scores), as those ones comprise the complete sample of studies. Experimental vs. Control and Pre and Follow up meta-analyses were estimated with subsamples (not every study had control group or follow-up measurement). Having this in mind, several analyses were performed in order to account for publication bias.
Firstly, funnel plots for pre–post effects are shown in Fig. 8. Visual inspection of the funnel plot for olfactory function (A) shows a slight left asymmetry, which may imply an underestimation of meta-analytic effect size. However, Egger’s test does not allow interpreting this potential asymmetry as statistically significant (Z = 1.303, p = 0.193). Following, Duval and Tweedie’s trim and fill method was applied to this model. This procedure points that no significant number of studies were missing from analysis, as a very similar effect size was estimated (g = 0.756). To conclude, fail-safe N was calculated through Rosenthal [37] procedure and 6912 null studies would be required to cancel the observed effect.
Regarding olfactory identification model, funnel plot (B) also points to visual asymmetry, with few studies showing effects sizes higher than g = 2 and other studies with effect sizes closer to 0. In this case, Egger’s test also does not allow interpreting this potential asymmetry as statistically significant (Z = 1.886, p = 0.059). Besides, trim and fill method was applied, giving an estimated effect of g = 0.843, pretty close to the original one. Hence, no missing studies might confound the estimated effect size. Fail-safe N indicates that 4007 null studies would be necessary to include in the analysis to elude the estimated effect size.
Preceding, olfactory discrimination funnel plot (C) is presented, which shows no visual evidence of asymmetry. Egger’s test is consistent with it, as there is no evidence of potential bias in the funnel plot (Z = 0.34, p = 0.734). Duval and Tweedie’s trim and fill analysis agrees with this line, as no missing studies are disturbing the analysis (trim and fill effect size of g = 0.585). Finally, fail-safe N equals to 1823 null studies in order to cancel the estimated effect size.
Finally, potential publication bias was analyzed on the olfactory threshold model. Its funnel plot (D) is also slightly asymmetrical on the left, but Egger’s test gives no evidence of an underestimation of effect size (Z = 0.855, p = 0.392). Trim and fill analysis reveals that no missing studies are noising the effect size estimation (g = 0.406) and fail-safe N points that 1015 null studies should be added to the model in order to fade the effect.
To conclude, these results support the statement that the current sample of primary studies might be a representative sample of all the studies about the efficacy of smell training in olfactory dysfunction.
Discussion
Olfactory dysfunction affects different categories of quality of life and daily life activities (ADLs), such as food enjoyment, personal hygiene, vital personal security, and it reduces the retrieval of memories associated with olfaction [1, 3, 68]. Emphasizing the hazardous effects that lead to inability to sense noxious chemicals, smoke, gas and spoiled food [69, 70] presents a great threat to one’s safety. Considering the importance of the sense of smell, studies have investigated its link with cognition and emotional status, they have observed olfactory deterioration in patients with neurodegenerative diseases [43, 44, 71]. Previous studies have reported that 25% to 33% of patients with olfactory dysfunction have symptoms of depression, and 27% to 30% indicate severe distress on general quality of life questionnaires due to their reduced sense of smell [3]. Further, physiologic anorexia, common in geriatric populations, may be partly due to diminished olfaction [3, 72].
Olfactory dysfunction is a problem with a variety of proposed etiologies, with postinfectious, posttraumatic, chronic inflammatory (rhinosinusitis, rhinitis), neurodegeneration causes being among the most common [72,73,74,75,76,77].
Olfactory loss is a challenging clinical problem with few proven therapeutic options. A wide range of treatment modalities for anosmia and hyposmia including corticosteroids [58], theophylline [78], antibiotics [79], and acupuncture have been attempted [79]. Non-pharmacological and non-invasive approaches have also been studied, such as olfactory training as a therapeutic approach [29, 80].
In the presented meta-analysis, it was analyzed previous smell training studies to provide a quantitative estimate of the effectiveness of olfactory training across four different olfactory domains—smell identification, discrimination, threshold and olfactory function (TDI), as well as specifying the potential moderator variables that influence olfactory recovery.
The primary objective of present meta-analysis was to evaluate the effectiveness of olfactory training as a therapeutic intervention for the rehabilitation of olfactory dysfunction. This study’s analyses demonstrate a positive and statistically significant effect of olfactory training in all olfactory abilities: with large effects of training on identification (g = 0.843), discrimination (g = 0.585) and TDI-score (g = 0.755), and small-to-moderate effect of threshold for odor detection (g = 0.406). When comparing pre–post performance in experimental groups (those who were submitted to the OT process due their OD). Those statistically significant effects were also observed when comparing olfactory capacity post olfactory training in experimental and control groups identification (g = 1.486), discrimination (g = 1.088) threshold (g = 0.087) and TDI-score (g = 2.124). And maintained when comparisons were drawn between pre and follow-up analysis identification (g = 1.355), discrimination (g = 1.498) threshold (g = 0.295) and TDI-score (g = 1.751). This overall effectiveness of the olfactory training is encouraging, given the importance of olfaction and inconsistent results regarding other forms of olfactory dysfunction treatment.
When comparing the experimental and control group there was no significant evidence to support OT effectiveness. In addressing the limited improvement in olfactory threshold observed following OT, it’s essential to assess the training protocol’s specific components. It is known that OT training protocols are more focused on discrimination and identification tasks, rather than targeting olfactory threshold directly, this could explain the modest improvements. Future studies should explore tailored training techniques explicitly designed to enhance olfactory threshold, such as incorporating exercises that challenge participants’ ability to detect minimal scent concentrations.
The second objective of this meta-analysis was to investigate the relationship between the observed olfactory training outcomes, duration of the training period, participants characteristics such as age, etiology and type of OD and OT method.
Interestingly, when comparing the results between experimental and control groups, in olfactory function (TDI), age presented a significant positive effect (b = 0.036, Z = 2.393, p = 0.016), although being known to having a negative impact on olfactory function [80,81,82,83,84,85]. This could be attributed to a statistical artifact. We categorized the mean age moderator in [18–40), [40–60) and [60, > 60] cohorts, with just 2 studies with mean age below 40 years. Meta-analytical effect size in these 2 studies is significantly lower compared with the other age groups and age cohorts are too reduced in sample size of studies to establish a conclusion. Age is widely recognized as a significant factor influencing olfactory function, with a notable decline typically observed around the age of 60 [64, 80, 83], Interestingly, the majority of studies included in this meta-analysis featured samples composed of participants aged 40 years or older [42, 46, 48]. This trend may be attributed to two primary factors. Firstly, younger participants are often associated with higher levels of neural plasticity, rendering them more susceptible to spontaneous improvements in olfactory function [11]. Secondly, volunteer-based investigations, which commonly comprise the participant pool in research studies, may inherently skew towards older age groups due to various biases [86].
Anosmia was considered a moderator variable due to its potential impact on the effectiveness of olfactory training interventions. Patients with anosmia typically exhibit a more pronounced olfactory dysfunction at baseline, reflecting the severity of their condition. Consequently, they often have a larger scope for improvement in olfactory function following interventions like olfactory training. This is because the extent of improvement can be more noticeable and impactful in individuals with anosmia, who start from a lower baseline level of olfactory function. Consequently, anosmia was considerate as a moderator in this meta-analysis since it allows researchers to explore how the severity of olfactory deficits influences the response to olfactory training interventions.
Statistical analysis also pointed out that “training duration” and “anosmia diagnosis” are predictors, whose effect on the outcome of olfactory training, was found to be positive and significant in olfactory identification on both pre–post and experimental-control analysis.
The same result regarding “duration of training” was observed on the meta-analysis of Sorokowska et al. [87], as well as in other studies [45, 55]. Nonetheless, it is noteworthy to specify that there is a probable ceiling effect after a certain training period, the potential ceiling effect of olfactory training presents an important consideration in its efficacy. Olfactory training involves repetitive exposure to odorants to stimulate olfactory neural pathways and improve olfactory function [88,89,90]. However, there may be a limit to the extent of improvement achievable through this method. Over time, individuals may reach a plateau where further gains in olfactory function become increasingly challenging to attain. This ceiling effect could be attributed to various factors, including the severity of olfactory dysfunction, the duration and intensity of training, and individual differences in neural plasticity [20, 45]. To address this, it's crucial to tailor olfactory training protocols to individual needs, considering factors such as baseline olfactory function and response to training. Additionally, determining the optimal duration for olfactory training is essential. Regarding OT, the duration of the training period remains a topic of ongoing debate [25, 27, 29]. The evidence presented in the literature showcases a range of perspectives, highlighting both the potential benefits of longer training periods and the practical considerations surrounding the optimal duration. It has been observed an improvement in olfactory function of 11% to 68% after 12–16 weeks of OT [26, 44].
However, Konstantinidis et al. [55] compared patients who performed OT for 16 and 56 weeks and found that the prolonged training benefited the proportion of subjects exhibiting clinically significant improvement (58% vs 71%, respectively). Nevertheless, the same study by Konstantinidis provides valuable insights into the stability of OT effects over time. For it showed that the effects of OT are stable over time and the improved olfactory performance of patients who underwent 16 weeks-long OT remained unchanged for the next 40 weeks, leading to the belief that OT should be extended to a minimum of training period of 16 weeks.
Regarding the “anosmia diagnosis” positive relationship with OT, it was seen in previous studies that anosmic patients, for being those who naturally had more to benefit from OT, presented better results after the training period, increasing their overall olfactory capacity [27, 91, 92].
The analysis revealed that the type of treatment administered did not yield statistically significant differences in outcomes. Whether studies exclusively utilized olfactory training or combined it with medication, the results did not demonstrate a substantial variation. It’s important to consider that some patients may have been receiving medications unrelated to olfactory loss (e.g. for hypertension or anti-Parkinson’s treatment). This introduces a potential confounding factor that could influence the outcomes of the analysis. Despite the presence of these medications, the results still did not indicate a statistically significant difference based on the type of treatment administered. This suggests that even in the presence of medications targeting other conditions, the combined approach of olfactory training with additional medications did not show a clear advantage over olfactory training alone in improving olfactory function.
When drawing comparisons between experimental and control groups the meta-analytical effect was close to 0 (g = 0.087], meaning that there is no statistical difference between both groups. A statistically significant difference was only found in the Kolldorfer and colleagues study [54], and such significance might be due the small sample size.
The same comparison between experimental and control groups, also pointed out that patients with OD due to post-viral or respiratory etiology gained more from OT, which was also observed in different studies [45, 52, 71, 87].
This meta-analysis revealed a substantial level of heterogeneity exceeding 80% in all conducted analyses. This heterogeneity could potentially be attributed to the limited sample sizes of the participants in the included studies. Furthermore, the overall quality assessment of the included studies indicated a moderate risk of bias, consistent with other meta-analyses investigating olfactory training [87, 93]. These findings emphasize the importance of addressing methodological limitations and enhancing the rigor of future studies in this field.
Another limitation that should be considered in future studies is the inclusion of disease duration, it's crucial to acknowledge that the inclusion of disease duration represents an important factor that could significantly impact the results. Therefore, it should be treated as a potential moderator and explored in future research.
The current study suggests that olfactory training might be a therapeutic modality for olfactory dysfunction. The majority of the studies reported positive outcomes in olfactory function without those possible side effects that can be seen if pharmacological or surgical interventions [90, 93]. This meta-analysis was consistent with the reported results on individual studies [26, 55, 92] and on systematic reviews and meta-analysis [87, 88] published with revealing improvements on olfactory function after training.
Conclusion
This study reveals a notable and statistically significant positive impact of olfactory training on the enhancement of all domains of olfactory function. Olfactory dysfunction represents a recurring challenge encountered across diverse etiologies. Although the precise mechanism by which olfactory training effectively restores or improves olfactory function remains elusive, this comprehensive meta-analysis provides compelling evidence that justifies further exploration of this therapeutic modality. Moreover, considering its proven efficacy, cost-effectiveness, and non-invasive nature, olfactory training merits careful consideration and integration into clinical practice as an efficacious and safe intervention.
Data availability
This is a meta-analysis of published work. All data are in the public domain in the form of manuscripts. Any and all data that we report are presented in either the body of the manuscript or the online supplemental material.
References
Frasnelli J, Hummel T (2005) Olfactory dysfunction and daily life. Eur Arch Otorhinolaryngol 262:231–235. https://doi.org/10.1007/s00405-004-0796-y
Neuland C, Bitter T, Marschner H, Gudziol H, Guntinas-Lichius O (2011) Health-related and specific olfaction-related quality of life in patients with chronic functional anosmia or severe hyposmia. Laryngoscope 121(4):867–872. https://doi.org/10.1002/lary.21387
Croy I, Nordin S, Hummel T (2014) Olfactory disorders and quality of life—an updated review. Chem Senses 39:185–194
Vennemann MM, Hummel T, Berger K (2008) The association between smoking and smell and taste impairment in the general population. J Neurol 255:1121–1126. https://doi.org/10.1007/s00415-008-0807-9
Murphy C (2002) Prevalence of olfactory impairment in older adults. JAMA 288:2307. https://doi.org/10.1001/jama.288.18.2307
Mackay-Sim A, Johnston ANB, Owen C, Burne THJ (2006) Olfactory ability in the healthy population: reassessing presbyosmia. Chem Senses 31:763–771. https://doi.org/10.1093/chemse/bjl019
Doty RL (2015) Olfactory dysfunction and its measurement in the clinic. World J Otorhinolaryngol-Head Neck Surg 1:28–33. https://doi.org/10.1016/j.wjorl.2015.09.007
Papazian EJ, Pinto JM (2007) Olfactory loss and aging: connections with health and well-being. Chem Senses 46:bjab045. https://doi.org/10.1093/chemse/bjab045
Yoo HS, Jeon S, Chung SJ et al (2018) Olfactory dysfunction in Alzheimer’s disease- and Lewy body-related cognitive impairment. Alzheimers Dement 14:1243–1252. https://doi.org/10.1016/j.jalz.2018.05.010
Morley JE (1997) Anorexia of aging: physiologic and pathologic. Am J Clin Nutr 66:760–773. https://doi.org/10.1093/ajcn/66.4.760
Wilson DA, Best AR, Sullivan RM (2004) Plasticity in the olfactory system: lessons for the neurobiology of memory. Neuroscientist 10:513–524. https://doi.org/10.1177/1073858404267048
Youngentob SL, Kent PF (1995) Enhancement of odorant-induced mucosal activity patterns in rats trained on an odorant identification task. Brain Res 670(1):82–88. https://doi.org/10.1016/0006-8993(94)01275-M
Hudson R, Distel H (1998) Induced peripheral sensitivity in the developing vertebrate olfactory system. Ann N Y Acad Sci 855:109–115. https://doi.org/10.1111/j.1749-6632.1998.tb10552.x
Wang L, Chen L, Jacob T (2004) Evidence for peripheral plasticity in human odour response: olfactory plasticity in humans. J Physiol 554:236–244. https://doi.org/10.1113/jphysiol.2003.054726
Blomqvist EH, Lundblad L, Bergstedt H, Stjärne P (2003) Placebo-controlled, randomized, double-blind study evaluating the efficacy of fluticasone propionate nasal spray for the treatment of patients with hyposmia/anosmia. Acta Otolaryngol 123:862–868. https://doi.org/10.1080/00016480310002140
Reden J, El-Hifnawi D, Zahnert T, Hummel T (2011) The effect of a herbal combination of primrose, gentian root, vervain, elder flowers, and sorrel on olfactory function in patients with a sinonasal olfactory dysfunction. Rhinology 49:342–346. https://doi.org/10.4193/Rhino10.151
Reden J, Herting B, Lill K et al (2011) Treatment of postinfectious olfactory disorders with minocycline: a double-blind, placebo-controlled study: postinfectious olfactory dysfunction. Laryngoscope 121:679–682. https://doi.org/10.1002/lary.21401
Reden J, Lill K, Zahnert T et al (2012) Olfactory function in patients with postinfectious and posttraumatic smell disorders before and after treatment with vitamin A: a double-blind, placebo-controlled, randomized clinical trial. Laryngoscope 122:1906–1909. https://doi.org/10.1002/lary.23405
Kollndorfer K, Fischmeister FPS, Kowalczyk K et al (2015) Olfactory training induces changes in regional functional connectivity in patients with long-term smell loss. NeuroImage Clin 9:401–410. https://doi.org/10.1016/j.nicl.2015.09.004
Whitcroft KL, Hummel T (2019) Clinical diagnosis and current management strategies for olfactory dysfunction: a review. JAMA Otolaryngol Head Neck Surg 145:846–853. https://doi.org/10.1001/jamaoto.2019.1728
Whitcroft KL, Hummel T (2020) Olfactory dysfunction in COVID-19: diagnosis and management. JAMA 323(24):2512–2514. https://doi.org/10.1001/jama.2020.8391
Rezaeyan A, Asadi S, Kamrava SK et al (2022) Reorganizing brain structure through olfactory training in post-traumatic smell impairment: an MRI study. J Neuroradiol 49:333–342. https://doi.org/10.1016/j.neurad.2021.04.035
Oleszkiewicz A, Bottesi L, Pieniak M et al (2022) Olfactory training with aromastics: olfactory and cognitive effects. Eur Arch Otorhinolaryngol 279:225–232. https://doi.org/10.1007/s00405-021-06810-9
Jiang R-S, Twu C-W, Liang K-L (2017) The effect of olfactory training on the odor threshold in patients with traumatic anosmia. Am J Rhinol Allergy 31:317–322. https://doi.org/10.2500/ajra.2017.31.4466
Saatci O, Altundag A, Duz OA, Hummel T (2020) Olfactory training ball improves adherence and olfactory outcomes in post-infectious olfactory dysfunction. Eur Arch Otorhinolaryngol 277:2125–2132. https://doi.org/10.1007/s00405-020-05939-3
Konstantinidis I, Tsakiropoulou E, Bekiaridou P et al (2013) Use of olfactory training in post-traumatic and postinfectious olfactory dysfunction: olfactory training short-term effect. Laryngoscope 123:E85–E90. https://doi.org/10.1002/lary.24390
Pellegrino R, Han P, Reither N, Hummel T (2019) Effectiveness of olfactory training on different severities of posttraumatic loss of smell: olfactory training in traumatic smell loss. Laryngoscope 129:1737–1743. https://doi.org/10.1002/lary.27832
Schriever VA, Lehmann S, Prange J, Hummel T (2014) Preventing olfactory deterioration: olfactory training may be of help in older people. J Am Geriatr Soc 62:384–386. https://doi.org/10.1111/jgs.12669
Altundag A, Cayonu M, Kayabasoglu G et al (2015) Modified olfactory training in patients with postinfectious olfactory loss: treatment of olfactory loss. Laryngoscope 125:1763–1766. https://doi.org/10.1002/lary.25245
Arya S, Kaji AH, Boermeester MA (2021) PRISMA reporting guidelines for meta-analyses and systematic reviews. JAMA Surg 156:789–790. https://doi.org/10.1001/jamasurg.2021.0546
Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M et al (2016) ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. https://doi.org/10.1136/bmj.i4919
Balduzzi S, Rücker G, Schwarzer G (2019) How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health 22:153–160. https://doi.org/10.1136/ebmental-2019-300117
R Core Team (2016) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. http://www.R-project.org/
Hedges LV (1982) Estimation of effect size from a series of independent experiments. Psychol Bull 92:490–499. https://doi.org/10.1037/0033-2909.92.2.490
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634. https://doi.org/10.1136/bmj.315.7109.629
Duval S, Tweedie R (2000) Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56:455–463. https://doi.org/10.1111/j.0006-341x.2000.00455.x
Rosenthal R (1979) The file drawer problem and tolerance for null results. Psychol Bull 86:638–641. https://doi.org/10.1037/0033-2909.86.3.638
Hummel T, Sekinger B, Wolf SR et al (1997) Sniffin” sticks’: olfactory performance assessed by the combined testing of odor identification, odor discrimination and olfactory threshold. Chem Senses 22:39–52
Abdelhafeez M, Elkholi SMA (2022) Efficacy of olfactory training program in conjunction with nasal steroid irrigation in treating persistent smell loss in COVID-19 patients. Arch Otolaryngol Rhinol 8(1):1–6. https://doi.org/10.17352/aor
Birte-Antina W, Ilona C, Antje H, Thomas H (2018) Olfactory training with older people. Int J Geriatr Psychiatry 33:212–220. https://doi.org/10.1002/gps.4725
Bratt M, Moen KG, Nordgård S et al (2020) Treatment of posttraumatic olfactory dysfunction with corticosteroids and olfactory training. Acta Otolaryngol 140:761–767. https://doi.org/10.1080/00016489.2020.1767301
Damm M, Schmitl L, Müller CA, Welge-Lüssen A, Hummel T (2019) Diagnostics and treatment of olfactory dysfunction. HNO 67:274–281. https://doi.org/10.1007/s00106-019-0614-x
Denis F, Septans A-L, Periers L et al (2021) Correction: Olfactory training and visual stimulation assisted by a web application for patients with persistent olfactory dysfunction after SARS-CoV-2 infection: observational study. J Med Internet Res 23:e32120. https://doi.org/10.2196/32120
Fleiner F, Lau L, Göktas Ö (2012) Active olfactory training for the treatment of smelling disorders. Ear Nose Throat J 91:198–203, 215. https://doi.org/10.1177/014556131209100508
Geißler K, Reimann H, Gudziol H et al (2014) Olfactory training for patients with olfactory loss after upper respiratory tract infections. Eur Arch Otorhinolaryngol 271:1557–1562. https://doi.org/10.1007/s00405-013-2747-y
Gellrich J, Han P, Manesse C et al (2018) Brain volume changes in hyposmic patients before and after olfactory training. Laryngoscope 128:1531–1536. https://doi.org/10.1002/lary.27045
Genetzaki S, Tsakiropoulou E, Nikolaidis V et al (2021) Postinfectious olfactory dysfunction: oral steroids and olfactory training versus olfactory training alone: is there any benefit from steroids? ORL J Otorhinolaryngol Relat Spec 83:387–394. https://doi.org/10.1159/000516316
Gürbüz D, Kesimli MC, Bilgili AM, Durmaz HÖ (2022) Olfactory rehabilitation and olfactory bulb volume changes in patients after total laryngectomy: a prospective randomized study. Braz J Otorhinolaryngol 88:607–612. https://doi.org/10.1016/j.bjorl.2021.02.013
Haehner A, Tosch C, Wolz M, Klingelhoefer L, Fauser M, Storch A et al (2013) Olfactory training in patients with Parkinson’s disease. PLoS ONE 8(4):e61680. https://doi.org/10.1371/journal.pone.0061680
Hosseini K, Zare-Sadeghi A, Sadigh-Eteghad S et al (2020) Effects of olfactory training on resting-state effective connectivity in patients with posttraumatic olfactory dysfunction. Acta Neurobiol Exp (Wars) 80:381–388. https://doi.org/10.21307/ane-2020-035
Jiang R-S, Twu C-W, Liang K-L (2019) The effect of olfactory training on odor identification in patients with traumatic anosmia. Int Forum Allergy Rhinol 9:1244–1251. https://doi.org/10.1002/alr.22409
Jiramongkolchai P, Jones MS, Peterson A et al (2021) Association of olfactory training with neural connectivity in adults with postviral olfactory dysfunction. JAMA Otolaryngol Head Neck Surg 147:502–509. https://doi.org/10.1001/jamaoto.2021.0086
Knudsen K, Flensborg Damholdt M, Mouridsen K, Borghammer P (2015) Olfactory function in Parkinson’s disease-effects of training. Acta Neurol Scand 132:395–400. https://doi.org/10.1111/ane.12406
Kollndorfer K, Kowalczyk K, Hoche E et al (2014) Recovery of olfactory function induces neuroplasticity effects in patients with smell loss. Neural Plast 2014:140419. https://doi.org/10.1155/2014/140419
Konstantinidis I, Tsakiropoulou E, Constantinidis J (2016) Long term effects of olfactory training in patients with post-infectious olfactory loss. Rhinology 54:170–175. https://doi.org/10.4193/Rhino15.264
Lamira JM, Soler ZM, Schlosser RJ (2019) A pilot study of olfactory training in older hyposmicadults. Am J Rhinol Allergy 33(6):650–656. https://doi.org/10.1177/1945892419858793
Langdon C, Lehrer E, Berenguer J et al (2018) Olfactory training in post-traumatic smell impairment: mild improvement in threshold performances: results from a randomized controlled trial. J Neurotrauma 35:2641–2652. https://doi.org/10.1089/neu.2017.5230
Bon L, Konopnicki SD, Pisarski D et al (2021) Efficacy and safety of oral corticosteroids and olfactory training in the management of COVID-19-related loss of smell. Eur Arch Otorhinolaryngol 278:3113–3117. https://doi.org/10.1007/s00405-020-06520-8
Liu DT, Sabha M, Damm M et al (2021) Parosmia is associated with relevant olfactory recovery after olfactory training. Laryngoscope 131:618–623. https://doi.org/10.1002/lary.29277
Mahmut MK, Oelschlägel A, Haehner A, Hummel T (2022) The impact of olfactory training using a nasal clip and extended periods of odor exposure. J Sens Stud. https://doi.org/10.1111/joss.12721
Mahmut MK, Musch M, Han P, Abolmaali N, Hummel T (2020) The effect of olfactory training on olfactory bulb volumes in patients with idiopathic olfactory loss. Rhinology 58(4):410–412. https://doi.org/10.4193/Rhin20.223
Morquecho-Campos P, Larsson M, Boesveldt S, Olofsson JK (2019) Achieving olfactory expertise: training for transfer in odor identification. Chem Senses 44:197–203. https://doi.org/10.1093/chemse/bjz007
Negoias S, Pietsch K, Hummel T (2017) Changes in olfactory bulb volume following lateralized olfactory training. Brain Imaging Behav 11:998–1005. https://doi.org/10.1007/s11682-016-9567-9
Oleszkiewicz A, Hanf S, Whitcroft KL et al (2018) Examination of olfactory training effectiveness in relation to its complexity and the cause of olfactory loss: OT complexity does not influence its effectiveness. Laryngoscope 128:1518–1522. https://doi.org/10.1002/lary.26985
Qiao X-F, Wang G-P, Li X et al (2019) Analysis of the clinical effect of olfactory training on olfactory dysfunction after upper respiratory tract infection. Acta Otolaryngol 139:643–646. https://doi.org/10.1080/00016489.2019.1614224
Yan XG, Gao X, Sun ZF et al (2018) Efficacy and associated factors of olfactory training in the treatment of olfactory dysfunction. Zhonghua er bi yan hou tou Jing wai ke za zhi=. Zhonghua er bi yan hou tou Jing wai ke za zhi= Chin J Otorhinolaryngol Head Neck Surg 53:815–819. https://doi.org/10.3760/cma.j.issn.1673-0860.2018.11.004
Choi BY, Jeong H, Noh H et al (2021) Effects of olfactory training in patients with postinfectious olfactory dysfunction. Clin Exp Otorhinolaryngol 14:88–92. https://doi.org/10.21053/ceo.2020.00143
Auinger AB, Besser G, Liu DT, Renner B, Mueller CA (2021) Long-term impact of olfactory dysfunction on daily life. Wien Klin Wochenschr 133:1004–1011. https://doi.org/10.1007/s00508-020-01751-5
Miwa T, Furukawa M, Tsukatani T et al (2001) Impact of olfactory impairment on quality of life and disability. Arch Otolaryngol Head Neck Surg 127:497–503. https://doi.org/10.1001/archotol.127.5.497
Doty RL (2009) The olfactory system and its disorders. Semin Neurol 29:74–81. https://doi.org/10.1055/s-0028-1124025
Helman SN, Adler J, Jafari A et al (2022) Treatment strategies for postviral olfactory dysfunction: a systematic review. Allergy Asthma Proc 43:96–105. https://doi.org/10.2500/aap.2022.43.210107
Schiffman SS, Warwick ZS (1988) Flavor enhancement of foods for the elderly can reverse anorexia. Neurobiol Aging 9:24–26. https://doi.org/10.1016/s0197-4580(88)80009-5
Marin C, Vilas D, Langdon C et al (2018) Olfactory dysfunction in neurodegenerative diseases. Curr Allergy Asthma Rep 18:42. https://doi.org/10.1007/s11882-018-0796-4
Addison AB, Wong B, Ahmed T et al (2021) Clinical olfactory working group consensus statement on the treatment of postinfectious olfactory dysfunction. J Allergy Clin Immunol 147:1704–1719. https://doi.org/10.1016/j.jaci.2020.12.641
Coelho DH, Costanzo RM (2016) Posttraumatic olfactory dysfunction. Auris Nasus Larynx 43:137–143. https://doi.org/10.1016/j.anl.2015.08.006
Guss J, Doghramji L, Reger C, Chiu AG (2009) Olfactory dysfunction in allergic rhinitis. ORL J Otorhinolaryngol Relat Spec 71:268–272. https://doi.org/10.1159/000242429
Lee JJ, Peterson AM, Kallogjeri D et al (2022) Smell changes and efficacy of nasal theophylline (SCENT) irrigation: a randomized controlled trial for treatment of post-viral olfactorydysfunction. Am J Otolaryngol 43:103299. https://doi.org/10.1016/j.amjoto.2021.103299
Wang J-J, Chen J, Doty RL (2018) Impact of antibiotics on smell dysfunction. World J Otorhinolaryngol-Head Neck Surg 4:33–38. https://doi.org/10.1016/j.wjorl.2018.03.002
Tanaka O, Mukaino Y (1999) The effect of auricular acupuncture on olfactory acuity. Am J Chin Med 27:19–24. https://doi.org/10.1142/S0192415X99000045
Doty R, Kamath V (2014) The influences of age on olfaction: a review. Front Psychol 5:20. https://doi.org/10.3389/fpsyg.2014.00020
Kondo K, Kikuta S, Ueha R, Suzukawa K, Yamasoba T (2020) Age-related olfactory dysfunction: epidemiology, pathophysiology, and clinical management. Front Aging Neurosci 12:208. https://doi.org/10.3389/fnagi.2020.00208
Pinto JM (2011) Olfaction. Proc Am Thorac Soc 8(1):46–52. https://doi.org/10.1513/pats.201005-035RN
Pinto JM, Wroblewski KE, Kern DW et al (2015) The rate of age-related olfactory decline among the general population of older U.S. adults. J Gerontol A Biol Sci Med Sci 70:1435–1441. https://doi.org/10.1093/gerona/glv072
Delgado-Losada ML, Delgado-Lima AH, Bouhaben J (2020) Spanish validation for olfactory function testing using the Sniffin’ sticks olfactory test: threshold, discrimination, and identification. Brain Sci 10:943. https://doi.org/10.3390/brainsci10120943
Delgado-Lima AH, Bouhaben J, Martínez-Zujeros S et al (2023) Could olfactory identification be a prognostic factor in detecting cognitive impairment risk in the elderly? GeroScience. https://doi.org/10.1007/s11357-023-00779-5
Andreeva VA, Salanave B, Castetbon K, Deschamps V, Vernay M, Kesse-Guyot E et al (2015) Comparison of the sociodemographic characteristics of the large NutriNet-Santé e-cohort with French census data: the issue of volunteer bias revisited. J Epidemiol Community Health 69:893–898. https://doi.org/10.1136/jech-2014-205263
Sorokowska A, Drechsler E, Karwowski M, Hummel T (2017) Effects of olfactory training: a meta-analysis. Rhinology 55:17–26. https://doi.org/10.4193/Rhino16.195
Hellings PW, Rombaux P (2009) Medical therapy and smell dysfunction. B-ENT 5(Suppl 13):71–75
Liang KL (2020) The effect of olfactory training on olfactory function in patients with olfactory loss: a systematic review and meta-analysis. Int Forum Allergy Rhinol 10(1):39–46. https://doi.org/10.1002/alr.22498
Hummel T, Nordin S (2005) Olfactory disorders and their consequences for quality of life. Acta Otolaryngol 125(2):116–121. https://doi.org/10.1080/00016480410022787
Damm M, Pikart LK, Reimann H et al (2014) Olfactory training is helpful in postinfectious olfactory loss: a randomized, controlled, multicenter study: olfactory training. Laryngoscope 124:826–831. https://doi.org/10.1002/lary.24340
Seiden AM (2004) Postviral olfactory loss. Otolaryngol Clin N Am 37:1159–1166. https://doi.org/10.1016/j.otc.2004.06.007
Pekala K, Chandra RK, Turner JH (2016) Efficacy of olfactory training in patients with olfactory loss: a systematic review and meta-analysis: systematic review of olfactory training. Int Forum Allergy Rhinol 6:299–307. https://doi.org/10.1002/alr.21669
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature.
Author information
Authors and Affiliations
Contributions
Conceptualization, M.L.D.-L. and A.H.D.-L.; methodology, A.H.D.-L., M.L.D.-L., and J.B.; data collection, A.H.D.-L., and J.B.; formal analysis, J.B.; investigation, A.H.D.-L. and M.L.D.-L.; writing—original draft preparation, M.L.D.-L., A.H.D.-L., and J.B; writing—review and editing, M.L.D.-L., A.H.D.-L., and J.B. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None declared.
Ethical approval
This is a meta-analysis of published work. All data are in the public domain in the form of manuscripts. Any and all data that we report are presented in either the body of the manuscript or the online supplemental material. We are happy to share the final collated data set.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Delgado‑Lima, A.H., Bouhaben, J. & Delgado‑Losada, M.L. The efficacy of olfactory training in improving olfactory function: a meta-analysis. Eur Arch Otorhinolaryngol 281, 5267–5284 (2024). https://doi.org/10.1007/s00405-024-08733-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-024-08733-7