Abstract
Purpose
The purpose of this study was to investigate the relations between functional hearing, language, social, bilateral coordination and manual dexterity skills in children with early cochlear implants (CIs).
Methods
Thirty children with CIs were included in this study. The manual dexterity and bilateral coordination development of the participants were evaluated with Manual Dexterity and Bilateral Coordination subtests of Bruininks-Oseretsky Motor Proficiency-2 (BOT-2). Their language skills were assessed by the Test of Early language Development-3. To assess the functional hearing of participants the Functioning After Pediatric Cochlear Implantation scale (FAPCI) was administered their caregivers. Also, the Social Skills Evaluation Scale was administered to participants’ teachers to asses their social skills.
Results
There were significant correlations between participants’ receptive and expressive language skills, Manual Dexterity, and FAPCI scores (p < 0.05). There were also significant relationships between the SSES and FAPCI scores of the participants (p < 0.05). However, the Bilateral Coordination subtest did not show any significant correlation with any of the measurements (p > 0.05).
Conclusion
The results suggest that the language, manual dexterity and functional hearing abilities of children with CIs are closely related. Although, there were no significant correlations between all of the measurement, it is important to look beyond hearing and speech evaluations to assess the whole child.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hearing is one of the earliest senses that develop, with the cochlea maturing by the 23rd week of gestation. Toddlers and children learn to communicate using oral language and develop cognitive skills through listening, but they can also interpret other people’s behavior and intentions [1].
Most children who are born deaf or become deaf before the age of 3 years lag behind their normal-hearing (NH) peers in spoken language skills. However, it is now known that early deafness affects nearly all aspects of general development, including cognitive, motor, and social domains [1]. The researchs suggest that prelingually deaf or hard of hearing children are at risk and may experience difficulty in developing social and emotional skills such as being able to recognize and manage emotions, appreciate the perspective of others, establish and maintain positive relationships [2, 3]. In addition, deaf children were found to be more likely to have deficiencies in motor abilities, including balance, coordination, visual-motor, and speed of movements [4, 5].
In order to prevent the negative effects of deafness, cochlear implants (CIs) have become widely accepted devices in the rehabilitation of deaf children [1]. According to research, age at implantation is an important factor in the outcomes of prelingually deaf children [6]. The rationale behind early implantation is based on neural plasticity and sensitive learning periods [7]. In human development, the first 3–4 years of life are defined as the most rapid synaptogenesis and highest central auditory nerve system plasticity. As a result, external auditory stimuli are crucial throughout the first 3–4 years of life for developing lower- and higher level neural connections [8].
It is well-known that no part of the brain works in isolation, early auditory deprivation alters the brain’s effective connectivity not only within the auditory system but also between auditory system and higher level cortex areas, such as the basal ganglia, cerebellum, entorhinal cortex, hippocampus, amygdala and frontal areas [9, 10]. These areas are crucial for motor development skills, executive functions and learning [9,10,11]. Recent studies revealed that bilateral coordination and manual dexterity skills involve a series of cerebral process including sensory input, perceptual and cognitive processing [12, 13]. Moreover, CI users have difficulty in cognitive skills [14]. Numerous studies have shown that early implantation improves spoken language, functional hearing and social abilities [7, 15, 16]. However, there have been few studies that investigate the relation between these abilities and bilateral coordination and manual dexterity motor developmental areas. In this study, we aimed to investigate the relations between functional hearing, language, social, bilateral coordination and manual dexterity development skills in children with early CIs.
Material and methods
This study was conducted at Hacettepe University Faculty of Health Sciences, Audiology Department and received ethical approval from the Hacettepe University Non-Interventional Clinic Research Ethics Board (GO20/762). The participants and their parents provided informed consent on the day of enrollment.
Participants
The study included a sample of 30 children with CIs (14 F, 16 M), aged between 4 and 6 years 11 months. The following inclusion criteria were used to determine the participants: (1) failing in the newborn hearing screening, (2) having prelingual severe to profound bilateral sensorineural hearing loss, (3) being a bilateral or unilateral CI user, (4) having the first CI surgery for up to 30 months, (5) having regular follow-up of medical, audiological, and auditory perception rehabilitation after surgery. Apart from these, children diagnosed with inner ear malformations, auditory neuropathy spectrum disorders, neurological or developmental disorders, learning difficulties, and other comorbidities were excluded.
Test battery
Test of Early Language Development (TELD-3)
The Turkish version of the Test of Early Language Development (TELD-3:T) was used to evaluate participants’ receptive and expressive language development. TELD-3 was developed by Hresko, Reid and Hammill [17]. The normative data for the Turkish validity and reliability of TELD-3 consisted of 1200 normally developing children aged between 18 months and 8 years. The results showed that the validity and reliability of TELD-3:T were strong and significant. Also, TELD-3:T accurately examined receptive and expressive language, and identified children with language delay and disorders [18]. The test comprises of verbal instructions provided to the child, as well as stimuli such as objects or drawings to which the child is expected to respond. In this study, we presented TELD-3:T scores as standard scores. Receptive and expressive language scores are calculated separately. The degree of spoken language development (very good, good, above average, average, below average, poor, very poor) was determined based on the combined scores of receptive and expressive language.
The Functioning After Pediatric Cochlear Implantation (FAPCI)
The Functioning After Pediatric Cochlear Implantation (FAPCI) was used to evaluate the functional hearing of participants. It is a family-centered communicative performance scale based on the World Health Organization’s conceptual model of functioning. It was developed by Lin et al. [19] to provide an objective assessment of the auditory performance of children with CIs. This scale evaluates verbal communication through educational and behavioral contexts rather than language skill. It consists of 23 questions, the lowest and highest possible scores are 23 and 115, respectively.
Turkish validity and reliability study of the FAPCI was conducted by Yücel et al. [20]. It was administered to families of children aged 2 to 6 years with NH and CIs, respectively. When the total scores of children with NH and CIs were evaluated for the construct validity of the scale, a significant difference was found between the scores of the 2 groups. FAPCI internal reliability consistency was also confirmed (Cronbach’s alpha coefficient > 0.90). The statistical analysis showed that Turkish version of FAPCI is a valid and reliable tool to evaluate the communication skills of children with CIs.
The Social Skills Evaluation Scale (SSES)
The Social Skills Assessment Scale (SSES), developed by Avcioglu [21] in 2007, was used to assess participant's social behavior skills. In the validity and reliability study, it was administered to teachers of children aged 4 to 6 years. For the content validity, an expert’s opinion was consulted. To determine the reliability of the scale Cronbach Alpha internal consistency was calculated and it was found 0.98. In this Likert-type scale consisting of 62 questions, evaluations were performed using the responses ‘always’, ‘very often’, ‘usually’, ‘very rarely’ and ‘never’. The minimum score obtainable on the scale is 62, and the maximum score is 310. A high score on the scale indicates that the child has adequate social abilities, whereas a low score suggests a lack of sufficient social skills. In this study, teachers providing special education and rehabilitation services rated the social skills of children who had not yet started kindergarten or school, while teachers rated the social skills of children who were enrolled in kindergarten or school.
Bruininks–Oseretsky Test of Motor Proficiency-2 (BOT-2)
The Bruininks–Oseretsky Test of Motor Proficiency-2 (BOT-2) was used to evaluate participants’ motor development skills. This is a performance-based test that evaluates the motor development and coordination skills of individuals aged 4 to 21 [22]. The test battery consists of four main components: (1) fine motor control, (2) dexterity coordination, (3) body coordination, (4) strength and agility, with eight sub-components: (1) fine motor precision, (2) fine motor integration, (3) manual dexterity, (4) bilateral coordination, (5) balance, (6) running speed and quality, (7) upper limb coordination, and (8) strength.
The BOT-2 standardization scores are based on normative data obtained from 1520 children and adolescents aged 4 to 21 years in the United States. It has well-established validity and reliability. The BOT-2’s content validity was confirmed through test content development, and it discriminates between different clinical groups and typically developing children. Inter-rater reliability of the BOT-2 is good ranging from 0.92 to 0.99 for the composite scores and test–retest reliability is good to excellent.
Four assessment options are available for the BOT-2: (1) complete form, (2) short form, (3) selected components, (4) selected sub-components. In this study, manual dexterity (making dots in circles, transferring pennies, placing pegs into a pegboard, sorting cards, stringing blocks) and bilateral coordination (touching nose with index fingers-eye closed, jumping jacks, jumping in place-same sides synchronized, jumping in place- same sides synchronized, pivoting thumbs and index fingers, tapping feet and fingers-same sides synchronized, tapping feet and fingers-opposite sides synchronized) sub-components of the test battery were included. The raw scores of sub-components are converted to the standard scores based on age and gender using the BOT-2 manual’s normative data. The standard scores also described into five categories: well-above average, above average, average, below average, and well-below average.
Statistical analysis
Statistical analysis was carried out using SPSS version 23. The variables’ normality was determined using histograms, probability plots, and Kolmogorov–Smirnov/Shapiro–Wilk’s test. Descriptive statistics were reported as mean, standard deviation for parametric variables, and reported as median, interquartile range (IQR) for non-parametric variables. The categorical variables were presented as frequencies and percentages. Pearson’s correlation coefficient was used to analyze the correlation between parametric variables, whereas Spearman’s correlation coefficient was used to analyze the correlation between non-parametric variables. Correlations were considered statistically significant when the p value was less than 0.05.
Results
Demographic and clinical characteristics of the participants
The sample comprised 30 children with CIs, consisting of 14 females and 16 males. The age range of the children was from 48 to 81 months, with a mean age of 60.73 ± 9.74 (months). Of the participants, 24 used bilateral CIs, while 6 used unilateral CI. Thirteen of the bilateral CIs users received their CIs sequentially, while eleven of them received their CIs simultaneously. The participants’ other clinical details are presented in Table 1.
Measurement outcomes
TELD-3 outcomes
The mean receptive language standard score was 85.53 ± 16.77 (min: 52, max: 112), and the mean expressive language standard score was 84.83 ± 21.69 (min: 50, max: 119). When the degree of spoken language development was examined, 30% (n = 9) of the participants were very poor, 10% (n = 3) were poor, 16.7% (n = 5) were below average, 33.3% (n = 10) were average, and 10% (n = 3) at the above average degree.
FAPCI outcomes
The assessment form has a maximum score of 115 and a minimum score of 23. The participants in this study had a mean FAPCI score of 93.77 ± 14.81, with a minimum score of 60 and a maximum score of 114.
SSES outcomes
The SSES has a maximum score of 310 and a minimum score of 62. The participants in this study had a mean SSES score of 198.67 ± 45.15, with a minimum score of 116 and a maximum score of 290.
BOT-2 outcomes
In the Manual Dexterity subtest, the mean standard score of the participants was found 11.37 ± 5.40. When the category of participants was examined, 10% of the participants were well-below average, 50% were below average, 30% were average, and 10% were above average category.
In the Bilateral Coordination subtest, the mean standard score of the participants was found 20.37 ± 4.59. When the category of participants was examined, 40% of the participants were average, 40% were above average, and 20% were well-above average category.
Correlation analysis outcomes
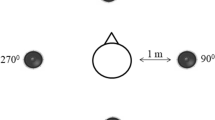
In the correlation analysis, the receptive language has a strong positive correlation with FAPCI scores (r = 0.67, p < 0.001) and a moderate positive correlation with Manual Dexterity (r = 0.47, p = 0.008) (Figs. 1, 2). Similarly, expressive language has a strong positive correlation with FAPCI scores (r = 0.76, p < 0.001) and a moderate positive correlation with the Manual Dexterity (r = 0.57, p = 0.001) (Figs. 3, 4). The FAPCI has a strong positive correlation with SSES (r = 0.70, p = 0.005) and a weak positive correlation with Manual Dexterity subtest scores (r = 0.03, p = 0.006) (Figs. 5, 6). There was no significant correlation found between the Bilateral Coordination subtest scores of the participants and their scores in language, FAPCI, and SSES (Table 2).
Discussion
This study investigated the relations between language abilities, functional hearing, social skills, bilateral coordination and manual dexterity skills in children with early CIs. Because the brain is an interconnected operating system, it is possible that an early period of auditory deprivation may have secondary neurological effects in addition to the obvious hearing-related effects [14]. Therefore, it is important to investigate the non-auditory and non-verbal abilities along with auditory and language skills in children with CIs.
CIs provide a significant advantage for individuals with prelingual HL through supporting the speech and language development [23]. In this study, we found that the degree of spoken language development of participants were mainly average. This is encouraging evidence in regards to the potential benefits of implantation. Kutlu et al. [24] noted that the acquisition of receptive and expressive language skills and functional hearing are related to each other. Functional hearing is about the how individual use their hearing to gather information, how they make sense of this information in various environments throughout the day [25]. Hence, evaluating the functional hearing enables us to gather insights into the communication skills of children in their daily lives. The study revealed the expected finding of a significant correlation between the receptive and expressive language and the functional hearing. This suggests that children with well-developed functional hearing skills are able to acquire language skills more quickly, enabling them to use their receptive and expressive language more efficiently.
The body of research indicates that the process of acquiring language is highly related to perceptual, computational, social, and neural systems, which also involve the motor development [26, 27]. It was suggested that early motor development provide opportunities for language acquisition supporting interaction and social engagement [28]. At the same time, the early exposure to language and the development of motor skills have a significant impact on the development of language acquisition, emphasizing important associations between objects, actions, and thoughts [27]. Brooks et al. [29] explained this connection via a neuropsychological approach in which brain regions associated with motor control, speech, and language abilities are connected. Several studies have shown disturbances in various aspects of motor performance in children with CIs. For example, Schlumberger et al. [30] and Conway et al. [14] found in their study that children with CIs experienced difficulties in the development of complex motor sequence production. In this study, we evaluated the participants’ manual dexterity skills using the Manual Dexterity subtest, which requires fine motor skills. The findings indicated that the participants’ manual dexterity development was generally below the typical norm values. The study also showed an association between manual dexterity skills and receptive and expressive language skills, as well as functional hearing. Similarly to the current study, Aslan et. al. [31] used to TELD-3 and BOT-2 to measure the language skills and motor development of children with inner ear malformations who received CIs. They found a significant correlation between participants’ motor skills and language development. In their review study, Gonzalez et al. [27] stated that most of the studies in the literature have established a significant relation between fine motor skills and language abilities. Additionally, they claimed that language studies focus more on gross motor skills than fine motor skills [27]. The relation between bilateral coordination skills, which mostly encompass gross motor skills, and language and functional hearing abilities was also investigated in this study, and no significant relationship was found. The findings demonstrated that participants’ bilateral coordination abilities were generally average or above average when compared to typical norm values. According to existing literature, gross motor abilities have a significant relationship with language abilities [32,33,34]. However, the majority of studies have been conducted during infancy and toddlerhood rather than childhood, which limits our interpretation of findings for older age ranges. In addition, Conway et al. [14] suggested that auditory deprivation can disrupt aspects of non-verbal cognition, particularly skills related to visual-motor patterns, even if hearing is restored with a CI. Because, visual-motor abilities require representation and organization of serial task [14]. As a result, many children with CIs are still likely to experience delays in the development of neural pathways that underlying these information processing systems [14, 35]. In this study, the Manual Dexterity subtest includes tasks that require higher visual-motor abilities than the Bilateral Coordination subtest. It was thought that this discrepancy in task requirements could explain the participants' more difficulty in the Manual Dexterity subtest in comparison to the Bilateral Coordination subtest.
Further, we evaluated the participants’ social skills in this study. Because social skills are crucial for the development of joint attention, reciprocation, and awareness of others' intentions and hearing-impaired children have social difficulties when compated to their NH peers [36]. Research has shown that CIs enable children with hearing impairments to prevent social isolation and actively engage in social interactions [37, 38]. The widely recognized advantage of the CIs mainly results from their impact on language and functional auditory abilities [16, 39]. The study revealed a significant correlation between the functional hearing abilities and social skills. However, there was not a significant relationship between social skills and receptive and expressive language abilities. Given the existing studies and the close connection between social and language skills [16, 38, 40], we were expecting to find a significant relationship between receptive and expressive language skills and social skills. Considering the children attended various special education services, schools, and kindergartens, SSES was rated by different teachers. We predicted that differences among raters could have subjectively affected the outcomes. Furthermore, it was observed that a variety of evaluation tools are used in research performed to evaluate social skills. This could be considered a contributing factor to the differences between the obtained results and the results reported in the current body of literature.
The study also examined the correlation between social skills and motor developmental skills, but no significant relationship was found. Studies have indicated a correlation between the development of the motor system and social interaction in children with typically developing and neurodevelopmental disorders [41, 42]. Especially, it was stated that gross motor skills predict social function in children with autism spectrum disorders [41]. In children with CIs, no previous research has investigated the correlation between the motor development abilities and social skills in the literature. Therefore, further research is needed to investigate the relationship between social abilities and motor development skills in children with CIs.
There were several limitations in this study. We did not include a control group with normal hearing. It was the main limitation of our study. Including normal-hearing group would have strengthened this study as it allowed comparisons between two groups. Furthermore, the study might have been strengthened by including children with severe to profound congenital hearing loss who did not use any amplification devices or only used hearing aids. This would have allowed for a more comprehensive evaluation of the early cochlear implant’s impact on language development, functional hearing abilities, social abilities, and motor development skills. Second, the participants were not homogenous in terms of amplification use. Six of the participants were unilateral CI users, and 24 were bilateral users. Additionally, to reflect the development of children with CIs, these assessments and analyses should be performed before and after implantation.
In sum, the present study provide an opportunity to examine the relations between functional hearing, language, social, bilateral coordination and manual dexterity development skills in children with early CIs. Our findings suggest that although children with CIs show age-typical levels of performance on bilateral coordination skills, they appear to be impaired on manual dexterity skills. Furthermore, manual dexterity skills, functional hearing abilities and receptive and expressive language outcomes were closely related with each other in these children. These findings suggest that professionals need to use a holistic approach in the evaluation and rehabilitation of children with CIs.
Data availability
Not applicable.
References
Paluch P et al (2019) Early general development and central auditory system maturation in children with cochlear implants—a case series. Int J Pediatr Otorhinolaryngol 126:109625. https://doi.org/10.1016/j.ijporl.2019.109625
Luckner JL, Movahedazarhouligh S (2019) Social–emotional interventions with children and youth who are deaf or hard of hearing: a research synthesis. J Deaf Stud Deaf Educ 24(1):1–10. https://doi.org/10.1093/deafed/eny030
Suarez M (2000) Promoting social competence in deaf students: the effect of an intervention program. J Deaf Stud Deaf Educ 5(4):323–333
Gheysen F, Loots G, Van Waelvelde H (2008) Motor development of deaf children with and without cochlear implants. J Deaf Stud Deaf Educ 13(2):215–224. https://doi.org/10.1093/deafed/enm053
de Sousa AMM, de França BJ, de Sousa Neto BM (2012) Postural control in children with typical development and children with profound hearing loss. Int J Gen Med. https://doi.org/10.2147/IJGM.S28693
Bruijnzeel H et al (2016) A systematic review to define the speech and language benefit of early (< 12 months) pediatric cochlear implantation. Audiol Neurotol. 21(2):113–126. https://doi.org/10.1159/000443363
Yoshinaga-Itano C et al (2018) Language outcomes improved through early hearing detection and earlier cochlear implantation. Otol Neurotol 39(10):1256–1263. https://doi.org/10.1097/MAO.0000000000001976
Cardon G, Campbell J, Sharma A (2012) Plasticity in the developing auditory cortex: evidence from children with sensorineural hearing loss and auditory neuropathy spectrum disorder. J Am Acad Audiol 23(06):396–411. https://doi.org/10.3766/jaaa.23.6.3
Hu Z et al (2021) Deficient sensory and cognitive processing in children with cochlear implants: An event-related potential study. Hear Res 408:108295. https://doi.org/10.1016/j.heares.2021.108295
Kral A et al (2016) Neurocognitive factors in sensory restoration of early deafness: a connectome model. Lancet Neurol 15(6):610–621. https://doi.org/10.1016/S1474-4422(16)00034-X
Luz C, Rodrigues LP, Cordovil R (2015) The relationship between motor coordination and executive functions in 4th grade children. Eur J Dev Psychol 12(2):129–141. https://doi.org/10.1080/17405629.2014.966073
Higashionna T et al (2017) Relationship between motor coordination, cognitive abilities, and academic achievement in Japanese children with neurodevelopmental disorders. Hong Kong J Occup Ther 30(1):49–55. https://doi.org/10.1016/j.hkjot.2017.10.002
Bonzano L et al (2023) Don’t plan, just do it: cognitive and sensorimotor contributions to manual dexterity. Neuroimage 280:120348. https://doi.org/10.1016/j.neuroimage.2023.120348
Conway CM et al (2011) Nonverbal cognition in deaf children following cochlear implantation: motor sequencing disturbances mediate language delays. Dev Neuropsychol 36(2):237–254. https://doi.org/10.1080/87565641.2010.549869
Sharma SD et al (2020) Hearing and speech benefits of cochlear implantation in children: a review of the literature. Int J Pediatr Otorhinolaryngol 133:109984. https://doi.org/10.1016/j.ijporl.2020.109984
İkiz M, Yücel E (2022) Examination of language, behavioral, academic, and social skills of cochlear implant users in early primary education. J Am Acad Audiol. https://doi.org/10.1055/a-1889-6534
Hresko WP, Reid DK, Hammill DD. TELD-3: Test of early language development; 1999. Pro-ed.
Topbaş S, Güven S (2013) TEDİL: Türkçe Erken Dil Gelişim Testi Kullanım Klavuzu. Detay Yayıncılık, Ankara
Lin FR et al (2007) Development of a communicative performance scale for pediatric cochlear implantation. Ear Hear 28(5):703–712. https://doi.org/10.1097/AUD.0b013e31812f71f4
ÖZkan HB et al (2020) Pediatrik Koklear İmplantasyon Sonrası İletişim Becerilerinin Değerlendirilmesi Ölçeği’nin Türkçe Sürümünün Geçerlilik ve Güvenirlilik Çalışması. Validity and reliability study of the Turkish version of the assessment of communication skills after pediatric cochlear implantation scale. Turkiye Klinikleri J Health Sci 5(2):264–271. https://doi.org/10.5336/healthsci.2019-71533
Avcıoğlu H (2007) Sosyal becerileri değerlendirme ölçeğinin geçerlik ve güvenirlik çalışması (4–6 yaş). Abant İzzet Baysal Üniversitesi Eğitim Fakültesi Dergisi 7(2):93–103
Bruininks RH, Bruininks BD. BOT2: Bruininks-Oseretsky test of motor proficiency; 2005. Pearson, Assessments. https://doi.org/10.1037/t14991-000
Hunter CR et al (2017) Early postimplant speech perception and language skills predict long-term language and neurocognitive outcomes following pediatric cochlear implantation. J Speech Language Hear Res 60(8):2321–2336. https://doi.org/10.1044/2017_JSLHR-H-16-0152
Kutlu S, Ozkan HB, Yucel E (2021) A study on the association of functional hearing behaviors with semantics, morphology and syntax in cochlear-implanted preschool children. Int J Pediatr Otorhinolaryngol 148:110814. https://doi.org/10.1016/j.ijporl.2021.110814
Grugel L et al (2011) Measuring communicative performance with the German version of the FAPCI-instrument: normative data and longitudinal results. Int J Pediatr Otorhinolaryngol 75(4):543–548. https://doi.org/10.1016/j.ijporl.2011.01.014
Calignano G et al (2023) Interconnected pathways: postural stability and vocabulary skills in preschool-aged children. Children 10(12):1891. https://doi.org/10.3390/children10121891
Gonzalez SL, Alvarez V, Nelson EL (2019) Do gross and fine motor skills differentially contribute to language outcomes? A systematic review. Front Psychol 10:2670. https://doi.org/10.3389/fpsyg.2019.02670
Brown T, Lane H (2014) Comparing a parent-report and a performance-based measure of children’s motor skill abilities: are they associated? Occup Ther Health Care 28(4):371–381. https://doi.org/10.3109/07380577.2014.933381
Obeid R, Brooks PJ (2018) Associations between manual dexterity and language ability in school-age children. Lang Speech Hear Serv Sch 49(4):982–994. https://doi.org/10.1044/2018_LSHSS-17-0124
Schlumberger E, Narbona J, Manrique M (2004) Non-verbal development of children with deafness with and without cochlear implants. Dev Med Child Neurol 46(9):599–606
Aslan F et al (2023) Unimodal versus bimodal auditory stimulation in inner ear malformations: cognitive, language, and motor performance. Laryngosc Investig Otolaryngol 8(5):1401–1409. https://doi.org/10.1002/lio2.1153
Muluk NB, Bayoğlu B, Anlar B (2016) A study of language development and affecting factors in children aged 5 to 27 months. Ear Nose Throat J 95(1):23–29
Houwen S et al (2016) The interrelationships between motor, cognitive, and language development in children with and without intellectual and developmental disabilities. Res Dev Disabil 53:19–31. https://doi.org/10.1016/j.ridd.2016.01.012
He M, Walle EA, Campos JJ (2015) A cross-national investigation of the relationship between infant walking and language development. Infancy 20(3):283–305. https://doi.org/10.1111/infa.12071
Horn DL, Pisoni DB, Miyamoto RT (2006) Divergence of fine and gross motor skills in prelingually deaf children: implications for cochlear implantation. Laryngoscope 116(8):1500–1506. https://doi.org/10.1097/01.mlg.0000230404.84242.4c
Hardman G et al (2022) Pre-linguistic social communication skills and post implant language outcomes in deaf children with cochlear implants. J Commun Disord 100:106275. https://doi.org/10.1016/j.jcomdis.2022.106275
Choo O-S et al (2021) Effect of age at cochlear implantation in educational placement and peer relationships. Ear Hear 42(4):1054–1061
Punch R, Hyde M (2011) Social participation of children and adolescents with cochlear implants: a qualitative analysis of parent, teacher, and child interviews. J Deaf Stud Deaf Educ 16(4):474–493. https://doi.org/10.1093/deafed/enr001
Aslan F, Yücel E (2019) Auditory reasoning skills of cochlear implant users. J Int Adv Otol 15(1):70. https://doi.org/10.5152/iao.2018.5400
Topcu O et al (2021) Social competence in children with cochlear implants: is it possible to catch up with their peers? Eur Arch Otorhinolaryngol 278:2775–2780. https://doi.org/10.1007/s00405-020-06363-3
Holloway JM, Long TM (2019) The interdependence of motor and social skill development: influence on participation. Phys Ther 99(6):761–770. https://doi.org/10.1093/ptj/pzz025
Lidstone DE, Mostofsky SH (2021) Moving toward understanding autism: Visual-motor integration, imitation, and social skill development. Pediatr Neurol 122:98–105. https://doi.org/10.1016/j.pediatrneurol.2021.06.010
Acknowledgements
This research did not receive any funding. The authors grateful to the children and their families who participated in the research.
Funding
Open access funding provided by the Scientific and Technological Research Council of Türkiye (TÜBİTAK).
Author information
Authors and Affiliations
Contributions
Şevval Utku Arat contributed to acquisition of data, statistical analysis and interpretation, and manuscript preparation. Merve İkiz Bozsoy contributed to interpretation of the data, and manuscript preparation; Esra Yücel contributed to study concept and design, analysis and interpretation of the data, and final approval of the article.
Corresponding author
Ethics declarations
Conflict of ınterest
No conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Arat, Ş.U., İkiz Bozsoy, M. & Yücel, E. The relationships between language, functional hearing, social, and motor development skills in children with early cochlear implants. Eur Arch Otorhinolaryngol (2024). https://doi.org/10.1007/s00405-024-08635-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00405-024-08635-8